Abstract
Background
α-Klotho was first identified as an aging gene and was later shown to be a regulator of phosphate metabolism. Fibroblast growth factor 23 (FGF23) is the key regulator of phosphate metabolism. Serum levels of soluble α-Klotho in chronic kidney disease (CKD) patients have not previously been determined, especially in relation with FGF23 and creatinine levels. This study was designed to investigate whether serum soluble α-Klotho levels are modulated by renal function, age, and FGF23 level in CKD patients. This study is the first report on the utility of measuring soluble α-Klotho levels in human CKD.
Methods
A total of 292 CKD patients were enrolled. Serum samples were collected, and FGF23 and soluble α-Klotho levels were measured using enzyme-linked immunosorbent assay kits. In addition, serum creatinine, hemoglobin, albumin, calcium, and phosphate levels were measured.
Results
Serum soluble α-Klotho levels were associated positively with estimated glomerular filtration rate (eGFR) (P < 0.0001) and inversely with serum creatinine level (P < 0.01). Interestingly, α-Klotho levels were significantly decreased in stage 2 CKD compared with stage 1 (P = 0.0001). Serum FGF23 levels were associated positively with serum creatinine and negatively with eGFR. FGF23 levels were significantly increased in stage 5 compared with stage 1 CKD. Soluble α-Klotho was associated inversely with log-transformed FGF23 level (P < 0.01).
Conclusion
Our data indicate that soluble α-Klotho levels are significantly decreased in stage 2 CKD compared to stage 1, and not only in the advanced stages of the disease. Soluble α-Klotho may thus represent a new biomarker for the diagnosis of CKD, especially in the early stage.






Similar content being viewed by others
References
Zhang QL, Rothenbacher D. Prevalence of chronic kidney disease in population-based studies: systematic review. BMC Public Health. 2008;8:117.
Manjunath G, Tighiouart H, Ibrahim H, Mac LB, Salem DN, Griffiht JL, et al. Level of kidney function as s risk factor for atherosclerotic cardiovascular outcomes in the community. J Am Coll Cardiol. 2003;41:47–55.
Baigent C, Burbury K, Wheeler D. Premature cardiovascular disease in chronic renal failure. Lancet. 2000;356:147–52.
Coresh J, Astor BC, Greene T, Eknoyan G, Levey AS. Prevalence of chronic kidney disease and decreased kidney function in the adult US population. Third National Health and Nutrition Examination Survey. Am J Kidney Dis. 2003;41:1–12.
Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298:2038–47.
Menon V, Shlipak MG, Wang X, Coresh J, Greene T, Stevens L, et al. Cystatin C as a risk factor for outcomes in chronic kidney disease. Ann Intern Med. 2007;147:19–27.
Tamara I, Huiliang X, Wei Y, Dawei X, Amanda HA, Julia S, et al. Fibroblast growth factor 23 and risks of mortality and end-stage disease in patients with chronic kidney disease. JAMA. 2011;305:2432–9.
Silvia MT, Roberto Z, Fabiliana GG, Luciene MR, Rui TB, Vanda J, et al. FGF23 as a predictor of renal outcome in diabetic nephropathy. J Am Soc Nephrol. 2011;6:241–7.
Sarah S, Birgit R, Daniel R, Eric S, Danilo F, Gunnar H. FGF-23 and future cardiovascular events in patients with chronic kidney disease before initiation of dialysis treatment. Nephrol Dial Transplant. 2010;25:3983–9.
Kurosu H, Ogawa Y, Miyoshi M, Yamamoto M, Nandi A, Rosenblantt KP, et al. Regulation of fibroblast growth factor-23 signaling by klotho. J Biol Chem. 2006;281:6120–3.
Urakawa I, Yamazaki Y, Shimada T, Iijima K, Hasegawa H, Okawa K, et al. Klotho converts canonical FGF receptor into a specific receptor for FGF23. Nature. 2006;444:770–4.
Nakatani T, Sarraj B, Ohnishi M, Densmore MJ, Taguchi T, Goetz R, et al. In vivo genetic evidence for klotho-dependent, fibroblast growth factor 23 (Fgf23)-mediated regulation of systemic phosphate homeostasis. FASEB J. 2009;23:433–41.
Kuro-o M, Matsumura Y, Aizawa H, Kawaguchi H, Suga T, Utsugi T, et al. Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature. 1997;390:45–51.
Hu MC, Shi M, Zhang J, Pastor J, Nakatani T, Lanske B, et al. Klotho: a novel phosphaturic substance acting as an autocrine enzyme in the renal proximal tubule. FASEB J. 2010;24:3438–50.
Kato Y, Arakawa E, Kinoshita S, Shirai A, Furuya A, Yamano K, et al. Establishment of the anti-Klotho monoclonal antibodies and detection of Klotho protein in kidneys. BBRC. 2000;267:597–602.
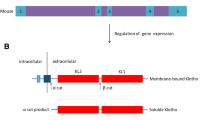
Chen CD, Podvin S, Gillespie E, Leeman SE, Abraham CR. Insulin stimulates the cleavage and release of the extracellular domain of Klotho by ADAM10 and ADAM17. Proc Natl Acad Sci USA. 2007;104:19796–801.
Bloch L, Sineshchekova O, Reichenbach D, Reiss K, Saftig P, Kuro-o M, et al. Klotho is a substrate for alpha-, beta- and gamma-secretase. FEBS Lett. 2009;583:3221–4.
Imura A, Iwano A, Tohyama O, Tsuji Y, Nozaki K, Hashimoto N, et al. Secreted Klotho protein in sera and CSF: Implication for post-translational cleavage in release of Klotho protein from cell membrane. FEBS Lett. 2004;565:143–7.
Chang Q, Hoefs S, van der Kemp AW, Topala CN, Bindels RJ, Hoenderop JG. The beta-glucosidase klotho hydrolyzes and activates the TRPV5 channel. Science. 2005;310:490–3.
Cha SK, Ortega B, Kurose H, Rosenblatt KP, Kuro-o M, Huang CL. Removal of sialic acid involving Klotho causes cell-surface retention of TRPV5 channel via binding to galactin-1. Proc Natl Acad Sci USA. 2008;105:9805–10.
Cha SK, Hu MC, Kurosu H, Kuro-o M, Moe O, Huang CL. Regulation of renal outer medullary potassium channel and renal K(+) excretion by klotho. Mol Pharmacol. 2009;76:38–46.
Yamazaki Y, Imura A, Urakawa I, Shimada T, Murakami J, Aono Y, et al. Establishment of sandwich ELISA for soluble alpha-Klotho measurement: age-dependent change of soluble alpha-Klotho levels in healthy subjects. BBRC. 2010;398:513–8.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009;53:982–92.
Yamazaki Y, Okazaki R, Shibata M, Hasegawa Y, Satoh K, Tajima T, et al. Increased circulatory level of biologically active full-length FGF-23 in patients with hypophosphatemic rickets/osteomalacia. J Clin Endocrinol Metab. 2002;87:4957–60.
Martin B, Marc V, Piet W, Gerjan N. Cross talk between the renin–angiotensin–aldosterone system and vitamin D–FGF-23–klotho in chronic kidney disease. J Am Soc Nephrol. 2011;22:1603–9.
Aizawa H, Saito Y, Nakamura T, Inoue M, Imanari T, Ohyama Y, et al. Downregulation of the Klotho gene in the kidney under sustained circulatory stress in rats. BBRC. 1998;249:865–71.
Koh N, Fujimori T, Nishiguchi S, Tamori A, Shiomi S, Nakatani T, et al. Severely reduced production of klotho in human chronic renal failure kidney. BBRC. 2001;280:1015–20.
Haruna Y, Kashihara N, Satoh M, Tomita N, Namikoshi T, Sasaki T, et al. Amelioration of progressive renal injury by genetic manipulation of Klotho gene. Proc Natl Acad Sci USA. 2007;104:2331–6.
Hu MC, Shi M, Zhang J, Quinones H, Griffith C, Kuro-o M, et al. Klotho deficiency causes vascular calcification in chronic kidney disease. J Am Soc Nephrol. 2011;22:124–36.
Tomiyama K, Maeda R, Urakawa I, Yamazaki Y, Tanaka T, Ito S, et al. Relevant use of Klotho in FGF19 subfamily signaling system in vivo. Proc Natl Acad Sci USA. 2010;107:1666–71.
Segawa H, Yamanaka S, Ohno Y, Onitsuka A, Shiozawa K, Aranami F, et al. Correlation between hyperphosphatemia and type II Na–Pi cotransporter activity in klotho mice. Am J Physiol Renal Physiol. 2007;292:F769–79.
Acknowledgments
This work was supported by Daiwa Memorial foundation, Japanese Kidney foundation, and a grant from the Ministry of Education, Science, Culture and Sports of Japan (to Y. S., K. I., K. O., S. F., and Y. T.) and a grant of Kochi Organization for Medical Reformation and Renewal to Y.T. We thank Ms. Reiko Matumoto, Ms. Sekie Saito for technical assistances.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Shimamura, Y., Hamada, K., Inoue, K. et al. Serum levels of soluble secreted α-Klotho are decreased in the early stages of chronic kidney disease, making it a probable novel biomarker for early diagnosis. Clin Exp Nephrol 16, 722–729 (2012). https://doi.org/10.1007/s10157-012-0621-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10157-012-0621-7