Abstract
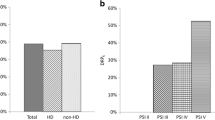
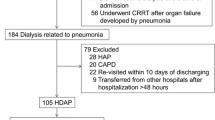
Although hemodialysis-associated pneumonia (HDAP) was included among the healthcare-associated pneumonias (HCAP) in the 2005 American Thoracic Society (ATS)/Infectious Diseases Society of America (IDSA) guideline, little information relevant to clinical epidemiology, especially microbiological characteristics, is available. This study aimed to reveal microbiological characteristics and clinical outcomes of HDAP and to assess whether HDAP should be included in the HCAP category. We retrospectively analyzed 69 HDAP patients [42 with moderate and 27 with severe disease based on A-DROP (age, dehydration, respiratory failure, orientation disturbance, and low blood pressure)] in whom sputum cultures were performed at our hospital between 2007 and 2009. The most common pathogens were Staphylococcus aureus (37.7%), which were composed of methicillin-resistant S. aureus (MRSA) (27.5%) and methicillin-sensitive S. aureus (MSSA) (10.1%), followed by Streptococcus pneumoniae (10.1%), Klebsiella pneumoniae (8.7%), Haemophilus influenzae (7.2%), and Moraxella catarrhalis (5.8%). This distribution mostly resembled the microbiological characteristics of HCAP reported previously, except that the frequency of multi-drug-resistant (MDR) gram negatives such as Pseudomonas aeruginosa (2.9%) was clearly lower and that of MRSA was higher. There were no significant differences in microbiological findings, including the incidence of MDR pathogens, between the two severity groups. Despite most cases (82.6%) receiving only monotherapy, the prognosis (30-day survival and in-hospital mortality rates were 88.4% and, 17.4%, respectively) was similar to the past HCAP reports, but there were no significant correlations between prognosis and presence of MDR pathogens (30-day mortality rates 18.2% in MDR positive vs. 8.5% in MDR negative; p = 0.242). Assessment for not only MDR pathogens, but also severity of illness by the A-DROP system made it possible to conduct stratification based on prognosis. Our results suggest that HDAP should be included in the HCAP category, while understanding that there are some differences.

Similar content being viewed by others
References
Nakai S, Masakane I, Shigematsu T, Hamano T, Yamagata K, Watanabe Y, et al. An overview of regular dialysis treatment in Japan (As of 31 December 2007). Ther Apher Dial. 2009;13:457–504.
Muraya Y, Oozono Y, Kadota J, Miyazaki M, Hashimoto A, Iida K, et al. Clinical and immunological evaluation of infection in patients on Hemodialysis. J Infect Chemother. 1996;2:247–53.
Sarnak MJ, Jaber BL. Pulmonary infectious mortality among patients with end-stage renal disease. Chest. 2001;120:1883–7.
Committee for the Japanese Respiratory Society Guidelines for the Management of Respiratory Infections. The Japanese Respiratory Society guidelines for the management of community-acquired pneumonia in adults. Respirology. 2006;11:S79–133.
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, et al. Infectious Disease Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44:S27–72.
British Thoracic Society Research Committee. Community-acquired pneumonia in adults in British hospitals in 1982–1983: a survey of aetiology, mortality, prognostic factors, and outcome. Q J Med. 1987;62:195–220.
Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, et al. Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Thorax. 2003;58:377–82.
American Thoracic Society, Infectious Disease Society of America. Guidelines for the management of adults with hospital-acquired, ventilator- associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2005;171:388–416.
Kollef MH, Marrow LE, Baughman RP, Craven DE, McGowan JE, Micek ST, et al. Health care-associated pneumonia (HCAP): a critical appraisal to improve identification, management, and outcomes-proceedings of the HCAP summit. Clin Infect Dis. 2008;46:296S–334S.
Kollef MH, Shorr A, Tabak YP, Gupta V, Liu LZ, Johannes RS. Epidemiology and outcome of health-care-associated pneumonia; results from a large US database of culture-positive pneumonia. Chest. 2005;128:3854–62.
Micek ST, Kollef KE, Reichley RM, Roubinian N, Kollef MH. Health care-associated pneumonia and community-acquired pneumonia: a single-center experience. Antimicrob Agents Chemother. 2007;51:3568–73.
Shindo Y, Sato S, Maruyama E, Ohashi T, Ogawa M, Hashimoto N, et al. Health-care-associated pneumonia among hospitalized patients in Japanese community hospital. Chest. 2009;135:633–40.
Ishida T, Hashimoto T, Arita M, Ito I, Osawa M. Etiology of community-acquired pneumonia in hospitalized patients. 1998;114:1588–1593.
Woodhead M. Community-acquired pneumonia guideline-an international comparison: a view from Europe. Chest. 1998;113:183S–7S.
Slinin Y, Foley RN, Collins AJ. Clinical epidemiology of pneumonia in hemodialysis patients: the USRDS waves 1, 3, and 4 study. Kidney Int. 2006;70:1135–41.
Guo H, Liu J, Collins AJ, Foley RN. Pneumonia in incident dialysis patients—the United States Renal Data System. Nephrol Dial Transplant. 2008;23:680–6.
Wakino S, Imai E, Yoshioka K, Kamayachi T, Minakuchi H, Hayashi K, et al. Clinical importance of Stenotrophomonas maltophilia nosocomial pneumonia due to its high mortality in hemodialysis patients. Ther Apher Dial. 2009;13:193–8.
Duran N, Ocak S, Eskiocak AF. Staphylococcus aureus nasal carriage among the diabetic and non-diabetic haemodialysis patients. Int J Clin Pract. 2006;60:1204–9.
Lederer SR, Riedelsdorf G, Schiffl H. Nasal carriage of meticillin resistant Staphylococcus aureus: the prevalence, patients at risk and the effect of elimination on outcomes among outclinic haemodialysis patients. Eur J Med Res. 2007;12:284–8.
Aarts MA, Hancock JN, Heyland D, McLeod RS, Marshall JC. Empiric antibiotic therapy for suspected ventilator-associated pneumonia: a systematic review and meta-analysis of randomized trials. Crit Care Med. 2008;36:108–17.
Heyland DK, Dodek P, Mscedere J, Day A, Cook D. Randomized trial of combination versus monotherapy for the empiric treatment of suspected ventilator-associated pneumonia. Crit Care Med. 2008;36:737–44.
Brito V, Niederman MS. Healthcare-associated pneumonia is a heterogeneous disease, and all patients do not need the same broad-spectrum antibiotic therapy as complex nosocomial pneumonia. Curr Opin Infect Dis. 2009;22:316–25.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kawasaki, S., Aoki, N., Kikuchi, H. et al. Clinical and microbiological evaluation of hemodialysis-associated pneumonia (HDAP): should HDAP be included in healthcare-associated pneumonia?. J Infect Chemother 17, 640–645 (2011). https://doi.org/10.1007/s10156-011-0228-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10156-011-0228-z