Abstract
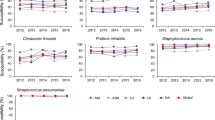
For the purpose of a nationwide surveillance of the antimicrobial susceptibility of bacterial respiratory pathogens in patients in Japan, the Japanese Society of Chemotherapy conducted their second year survey, during the period from January to August, 2007. A total of 1178 strains were collected from clinical specimens obtained from adult patients with well-diagnosed respiratory tract infections. Susceptibility testing was evaluable for 1108 strains (226 Staphylococcus aureus, 257 Streptococcus pneumoniae, 6 Streptococcus pyogenes, 206 Haemophilus influenzae, 120 Moraxella catarrhalis, 122 Klebsiella pneumoniae, and 171 Pseudomonas aeruginosa). A total of 44 antibacterial agents, including 26 β-lactams (four penicillins, three penicillins in combination with β-lactamase inhibitors, four oral cephems, eight parenteral cephems, one monobactam, five carbapenems, and one penem), three aminoglycosides, four macrolides (including ketolide), one lincosamide, one tetracycline, two glycopeptides, six fluoroquinolones, and one oxazolidinone were used for the study. Analysis was conducted at the central reference laboratory according to the method recommended by the Clinical and Laboratory Standards Institute (CLSI). The incidence of methicillinresistant Staphylococcus aureus (MRSA) was high, at 59.7%, and the incidences of penicillin-intermediateresistant and -resistant Streptococcus pneumoniae (PISP and PRSP) were 30.4% and 5.1%, respectively. Among Haemophilus influenzae strains, 19.9% of them were found to be β-lactamase-non-producing ampicillin (ABPC)-intermediately-resistant (BLNAI), 29.1% to be β-lactamasenon-producing ABPC-resistant (BLNAR), and 6.7% to be β-lactamase-producing ABPC-resistant (BLPAR) strains. Extended-spectrum β-lactamase-producing Klebsiella pneumoniae was not isolated. Two isolates (1.2%) of Pseudomonas aeruginosa were found to be metallo-β-lactamase-producing strains, including one (0.6%) suspected multidrug-resistant strain showing resistance to imipenem, amikacin, and ciprofloxacin. These data will be a useful reference for future periodic surveillance studies and for investigations to control resistant infections as well. Continued surveillance is required to prevent the further spread of these antimicrobial resistances.
Similar content being viewed by others
References
Niki Y, Hanaki H, Yagisawa M, Kohno S, Aoki N, Watanabe A, et al. The first nationwide surveillance of bacterial respiratory pathogens conducted by the Japanese Society of Chemotherapy. Part 1: a general view of antibacterial susceptibility. J Infect Chemother 2008;14:279–290.
Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing, 17th informational supplement M100-S17 and M45-A. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically; approved standard. 7th ed. Document M7-A7. Wayne, PA: Clinical and Laboratory Standards Institute; 2007.
Hanaki H, Kubo R, Nakano T, Kurihara M, Sunagawa K. Characterization of HMRZ-86: a novel chromogenic cephalosporin for the detection of extended-spectrum beta-lactamases. J Antimicrob Chemother 2004;53:888–889.
Colodner R, Reznik B, Gal V, Yamazaki H, Hanaki H, Kubo R. Evaluation of a novel kit for the rapid detection of extended-spectrum beta-lactamases. Eur J Clin Microbiol Infect Dis 2006;25:49–51.
Jenkins SG, Farrell DJ, Patel M, Lavin BS. Trends in anti-bacterial resistance among Streptococcus pneumoniae isolated in the USA, 2000–2003: PROTEKT US years 1–3. J Infect 2005;51:355–363.
Barada K, Hanaki H, Ikeda S, Yamaguchi Y, Akama H, Nakae T, et al. Trends in the gentamicin and arbekacin susceptibility of methicillin-resistant Staphylococcus aureus and the genes encoding aminoglycoside-modifying enzymes. J Infect Chemother 2007; 13:74–78.
Mochizuki T, Okamoto N, Yagishita T, Takuhiro K, Mashiko K, Ogawa F, et al. Analysis of antimicrobial drug resistance of Staphylococcus aureus strains by WHONET 5: microbiology laboratory database software. J Nippon Med Sch 2004;71:345–351.
Kamiya H, Kato T, Togashi T, Iwata S, Kurosaki T, Baba S, et al.; The Research Group on Streptococcus pneumoniae Serotypes among Children. Epidemiological survey of pneumococcus serotypes in pediatric patients with acute suppurative otitis media (in Japanese; abstract in English). Kansenshogaku Zasshi 2007; 81:59–66.
Chiba N, Kobayashi R, Hasegawa K, Morozumi M, Nakayama E, Tajima T, et al.; Acute Respiratory Diseases Study Group. Antibiotic susceptibility according to genotype of penicillin-binding protein and macrolide resistance genes, and serotype of Streptococcus pneumoniae isolates from community-acquired pneumonia in children. J Antimicrob Chemother 2005;56:756–760.
Karlowsky JA, Thornsberry C, Critchley IA, Jones ME, Evangelista AT, Noel GJ, Sahm DF. Susceptibilities to levofloxacin in Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis clinical isolates from children: results from 2000–2001 and 2001–2002 TRUST studies in the United States. Antimicrob Agents Chemother 2003;47:1790–1797.
Hasegawa K, Kobayashi R, Takada E, Ono A, Chiba N, Morozumi M, et al.; Nationwide Surveillance for Bacterial Meningitis. High prevalence of type b beta-lactamase-non-producing ampicillinresistant Haemophilus influenzae in meningitis: the situation in Japan where Hib vaccine has not been introduced. J Antimicrob Chemother 2006;57:1077–1082.
Muratani T, Matsumoto T. Urinary tract infection caused by fluoroquinolone- and cephem-resistant Enterobacteriaceae. Int J Antimicrob Agents 2006;28(Suppl 1):10–13.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Niki, Y., Hanaki, H., Matsumoto, T. et al. Nationwide surveillance of bacterial respiratory pathogens conducted by the Japanese Society of Chemotherapy in 2007: general view of the pathogens’ antibacterial susceptibility. J Infect Chemother 15, 156–167 (2009). https://doi.org/10.1007/s10156-009-0674-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10156-009-0674-z