Abstract
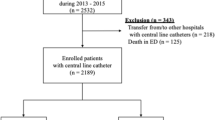
We aimed to evaluate the risk factors, including the hospital epidemiology of methicillin-resistant Staphylococcus aureus (MRSA), for central venous line-associated and laboratory-confirmed bloodstream infections (CLA-BSI and LC-BSI, respectively). The risk factors examined included the age and sex of patients, whether or not they were in the surgery service, the number of days of central line (CL) placement, the monthly number of inpatients and those positive for MRSA, and whether the standard or maximal barrier precautions were observed at CL insertion. As the outcome factors, we selected CLA-BSI and LC-BSI, while precluding repeated isolation within 28 days. Of a total of 22 723 device days in 927 patients with CL placement, we observed 81 CLA-BSIs and 40 LC-BSIs, rates of 3.56 and 1.76 (/1000 device-days), respectively. Logistic regression analysis revealed a single significant factor, CL placement of more than 30 days, with odds ratios of 3.038 [95% confidence interval (CI) 1.733–5.326; P < 0.001] for CLA-BSI and 3.227 (95% CI 1.427–7.299; P = 0.005) for LC-BSI. Both BSIs included MRSA in seven events without temporal clusters. We conclude that the factor of long CL placement outweighs other risk factors, including the hospital epidemiology of MRSA.
Similar content being viewed by others
References
Yoshida J, Ishimaru T, Fujimoto M, Hirata N, Matsubara N, Koyanagi N. Risk factors for central venous catheter-related bloodstream infection: a 1073-patient study. J Infect Chemother. 2008;14:399–403.
Marschall J, Mermel LA, Classen D, Arias KM, Podgorny K, Anderson DJ et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals. Infect Control Hosp Epidemiol. 2008;29:S22–30.
Centers for Diseases Control and Prevention. Appendix A. Examples of clinical definitions for catheter-related infections. MMWR Morb Mortal Wkly Rep. 2002; 5:127–8.
Weber DJ, Sickbert-Bennett EE, Brown V, Rutala WA. Comparison of hospital wide surveillance and targeted intensive care unit surveillance of healthcare-associated infections. Infect Control Hosp Epidemiol. 2007;28:1361–6.
Raad I, Hanna H, Dvorak T, Chaiban G, Hachem R. Optimal antimicrobial catheter lock solution, using different combinations of minocycline, EDTA, and 25-percent ethanol, rapidly eradicates organisms embedded in biofilm. Antimicrob Agents Chemother. 2007;51:78–83.
Johnston BL, Conly JM. What do central venous catheter-associated bloodstream infections have to do with bundles? Can J Infect Dis Med Microbiol. 2005;16:215–8.
Zack J. Zeroing in on zero tolerance for central line-associated bacteremia. Am J Infect Control. 2008;36:S176.e1–2.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Yoshida, J., Ishimaru, T., Kikuchi, T. et al. Central line-associated bloodstream infection: is the hospital epidemiology of methicillin-resistant Staphylococcus aureus relevant?. J Infect Chemother 16, 33–37 (2010). https://doi.org/10.1007/s10156-009-0018-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10156-009-0018-z