Abstract
Background
Defecation is a complex process and up to 25% of the population suffer from symptoms of defecatory dysfunction. For functional testing, diagnostics, and therapy of anorectal disorders, it is important to know the optimal defecation position. is The aim of this study was to evaluate defecation pressure patterns in side lying, seated and squatting defecation positions in normal subjects using a simulated stool device called Fecobionics.
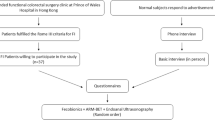
Methods
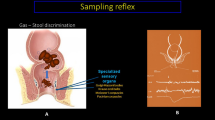
The Fecobionics expulsion parameters were assessed in an interventional study design conducted from May 29 to December 9 2019. Subjects were invited to participate in the study through advertisement at The Chinese University of Hong Kong. The Fecobionics device consisted of a core containing pressure sensors at the front (caudal end) and rear (cranial end) and a polyester-urethane bag spanning most of the core length which also contained sensors. The Fecobionics bag was distended to 50 ml in the rectum of normal subjects (no present and past symptoms of defecatory disorders, no prior abdominal surgery, medication or chronic diseases). Studies were done in side lying (left lateral recumbent position), seated (hip flexed 90°) and squatting position (hip flexed 25°). Pressure endpoints including the rear-front pressure diagram and defecation indices were compared between positions.
Results
Twelve subjects (6 females/6 males, mean age 26.3 ± 2.6 [19.0–48.0] years) were included and underwent the planned procedures. The resting anal pressure for side lying and seated positions were 33.1 ± 4.1 cmH2O and 37.1 ± 4.0 cmH2O (p > 0.3). The anal squeeze pressure for side lying and seated positions were 98.4 ± 6.9 cmH2O and 142.3 ± 16.4 cmH2O (p < 0.05). The expulsion duration for the side lying, seated and squatting positions were 108.9 ± 8.3 s, 15.0 ± 2.1 s and 16.1 ± 2.9 s, respectively (p < 0.01 between lying and the two other positions). The maximum evacuation pressure for seated and squatting were 130.1 ± 12.4 cmH2O and 134.0 ± 11.1 cmH2O (p > 0.5). Rear-front pressure diagrams and distensibility indices demonstrated distinct differences in pressure patterns between the side lying position group and the other positions.
Conclusions
The delay in expelling the Fecobionics device in the lying position was associated with dyssynergic pressure patterns on the device. Quantitative differences were not found between the seated and squatting position.
Trial Registration http://www.clinicaltrials.gov Identifier: NCT03317938.





Similar content being viewed by others
References
Gregersen H, Christensen J (2016) Clinical mechanics in the gut: an introduction. Bentham Science Publishers, London
Rao SS, Bharucha AE, Chiarioni G, Felt-Bersma R, Knowles C, Malcolm A, Wald A (2016) Anorectal disorders. Gastroenterology. https://doi.org/10.1053/j.gastro.2016.02.009
Suares NC, Ford AC (2011) Prevalence of, and risk factors for, chronic idiopathic constipation in the community: systematic review and meta-analysis. Am J Gastroenterol 106(9):1582–1591
Rao SS, Kavlock R, Rao S (2006) Influence of body position and stool characteristics on defecation in humans. Am J Gastroenterol 101(12):2790–2796
Wu GJ, Xu F, Lin L, Pasricha PJ, Chen JDZ (2017) Anorectal manometry: should it be performed in a seated position? Neurogastroenterol Motil 29:5. https://doi.org/10.1111/nmo.12997
Sharma M, Muthyala A, Feuerhak K, Puthanmadhom Narayanan S, Bailey KR, Bharucha AE (2020) Improving the utility of high-resolution manometry for the diagnosis of defecatory disorders in women with chronic constipation. Neurogastroenterol Motil 32(10):e13910. https://doi.org/10.1111/nmo.13910
Modi RM, Hinton A, Pinkhas D, Groce R, Meyer MM, Balasubramanian G, Levine E, Stanich PP (2019) Implementation of a defecation posture modification device: impact on bowel movement patterns in healthy subjects. J Clin Gastroenterol 53(3):216–219. https://doi.org/10.1097/MCG.0000000000001143
Sakakibara R, Tsunoyama K, Hosoi H, Takahashi O, Sugiyama M, Kishi M, Ogawa E, Terada H, Uchiyama T, Yamanishi T (2010) Influence of body position on defecation in humans. LUTS 2(1):16–21
Sikirov D (2003) Comparison of straining during defecation in three positions: results and implications for human health. Dig Dis Sci 48(7):1201–1205
Rad S (2002) Impact of ethnic habits on defecographic measurements. Arch Iranian Med 5(2):115–117
Takano S, Sands DR (2016) Influence of body posture on defecation: a prospective study of “The Thinker” position. Tech Coloproctol 20(2):117–121. https://doi.org/10.1007/s10151-015-1402-6
Gregersen H, Krogh K, Liao D (2018) Fecobionics: integrating anorectal function measurements. Clin Gastroenterol Hepatol 16(6):981–983. https://doi.org/10.1016/j.cgh.2017.09.057
Sun D, Huang Z, Zhuang Z, Ma Z, Man LK, Liao D, Gregersen H (2019) Fecobionics: a novel bionics device for studying defecation. Ann Biomed Eng 47(2):576–589. https://doi.org/10.1007/s10439-018-02149-1
Gregersen H, Lo KM (2018) What is the future of impedance planimetry in gastroenterology? J Neurogastroenterol Motil 24(2):166–181. https://doi.org/10.5056/jnm18013
Gregersen H, Chen SC, Leung WW, Wong C, Mak T, Ng S, Futaba K (2019) Novel fecobionics defecatory function testing. Clin Transl Gastroenterol 10(12):e00108. https://doi.org/10.14309/ctg.0000000000000108
Liao D, Chen SC, Lo KM, Zhao J, Futaba K, Gregersen H (2019) Theoretical tools to analyze anorectal mechanophysiological data generated by the fecobionics device. J Biomech Eng 141:9. https://doi.org/10.1115/1.4044134
Chen S-C, Futaba K, Leung WW, Wong C, Mak T, Ng S, Gregersen H (2020) Simulated stool for assessment of anorectal physiology. Am J Physiol Gastrointest Liver Physiol 319(4):G462–G468. https://doi.org/10.1152/ajpgi.00242.2020
Gregersen H, Chen SC, Leung WW, Wong C, Mak T, Ng S, Futaba K (2020) Fecobionics characterization of patients with fecal incontinence. Clin Gastroenterol Hepatol. https://doi.org/10.1016/j.cgh.2020.10.043
Palit S, Thin N, Knowles CH, Lunniss PJ, Bharucha AE, Scott SM (2016) Diagnostic disagreement between tests of evacuatory function: a prospective study of 100 constipated patients. Neurogastroenterol Motil 28(10):1589–1598. https://doi.org/10.1111/nmo.12859
Grossi U, Carrington EV, Bharucha AE, Horrocks EJ, Scott SM, Knowles CH (2016) Diagnostic accuracy study of anorectal manometry for diagnosis of dyssynergic defecation. Gut 65(3):447–455. https://doi.org/10.1136/gutjnl-2014-308835
Agachan F, Chen T, Pfeifer J, Reissman P, Wexner SD (1996) A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum 39(6):681–685. https://doi.org/10.1007/bf02056950
Rockwood TH (2004) Incontinence severity and QOL scales for fecal incontinence. Gastroenterology 126(1 Suppl 1):S106-113. https://doi.org/10.1053/j.gastro.2003.10.057
Heaton KW, Radvan J, Cripps H, Mountford RA, Braddon FE, Hughes AO (1992) Defecation frequency and timing, and stool form in the general population: a prospective study. Gut 33(6):818–824. https://doi.org/10.1136/gut.33.6.818
Lam TC, Islam N, Lubowski DZ, King DW (1993) Does squatting reduce pelvic floor descent during defaecation? Aust N Z J Surg 63(3):172–174. https://doi.org/10.1111/j.1445-2197.1993.tb00512.x
Tagart REB (1966) The anal canal and rectum: their varying relationship and its effect on anal continence. Dis Colon Rectum 9(6):449–452. https://doi.org/10.1007/bf02617443
Takeuchi M, Odake M, Takaoka H, Hayashi Y, Yokoyama M (1992) Comparison between preload recruitable stroke work and the end-systolic pressure-volume relationship in man. Eur Heart J 13:80–84. https://doi.org/10.1093/eurheartj/13.suppl_e.80
Norton NJ (2004) The perspective of the patient. Gastroenterology 126(1 Suppl 1):S175-179. https://doi.org/10.1053/j.gastro.2003.10.081
Whitehead WE, Borrud L, Goode PS, Meikle S, Mueller ER, Tuteja A, Weidner A, Weinstein M, Ye W, Pelvic Floor Disorders N (2009) Fecal incontinence in US adults: epidemiology and risk factors. Gastroenterology 137(2):512-517.e5172. https://doi.org/10.1053/j.gastro.2009.04.054
Chakrabarti SD, Ganguly R, Chatterjee SK, Chakravarty A (2002) Is squatting a triggering factor for stroke in Indians? Acta Neurol Scand 105(2):124–127. https://doi.org/10.1034/j.1600-0404.2002.1o196.x
Chew G, Liao WB, Hsu TS, Bullard MJ (1996) Defecation induced deep venous thrombosis. A case report Jpn Heart J 37(3):409–415. https://doi.org/10.1536/ihj.37.409
Funding
The Chinese University of Hong Kong (strategic recruitment funding), RCG grant #14106717, and HMRF grant #07180856.
Author information
Authors and Affiliations
Contributions
HG, KF, TM, and SN designed the study and supervised the experimental work. SC, KF, WL, CW, and HG participated with the experiments. Data analysis was conducted by SC and HG and interpreted by all authors. All authors had access to the data, revised the manuscript and approved the final version for submission.
Corresponding author
Ethics declarations
Conflict of interest
HG is the inventor and filed patent applications. No other conflicts of interest noted.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, SC., Futaba, K., Leung, W.W. et al. Fecobionics assessment of the effect of position on defecatory efficacy in normal subjects. Tech Coloproctol 25, 559–568 (2021). https://doi.org/10.1007/s10151-021-02439-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-021-02439-2