Abstract
Background
Invasion of submucosa (ISM) is required for the pathological diagnosis of colorectal cancer according to the WHO criteria. A large proportion of colorectal cancers may be underdiagnosed as high-grade intraepithelial neoplasia (HGIN) because ISM is not identified in the preoperative biopsy. The aim of this study was to investigate the clinicopathologic features that are associated with missing the diagnosis of ISM in biopsy specimens of invasive colorectal cancer.
Methods
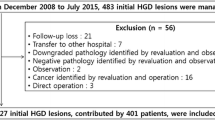
Three hundred and sixteen patients diagnosed with colorectal cancer between January 2007 and December 2008 with well-preserved preoperative biopsy specimens were enrolled in the study. Three hundred and eleven patients had an isolated lesion, and five had two lesions. Biopsy specimens were reevaluated by two senior pathologists. Clinicopathologic features, biopsy pathology and surgical pathology results of all patients were analyzed by univariate and multivariate analyses.
Results
ISM was identified in 216 cases (67.3 %) by biopsy-based pathological examination, and missed in 105 (32.7 %) cases, 72 of which were diagnosed as HGIN. Univariate analysis indicated that in colorectal cancer patients with smaller biopsy specimens (P = 0.042), mucinous or signet-ring cell carcinoma (P = 0.003), higher WHO tumor grade (P = 0.001) and positive lymph nodes (P = 0.011), ISM was more likely to be missed. There was a trend toward an increased diagnosis of ISM with the increase in the number of biopsy specimens (P = 0.105). On multivariate logistic regression analysis, smaller biopsy specimens (OR, 1.810; 95 % CI, 1.081–3.032; P = 0.024) and higher WHO tumor grade (OR, 2.073; 95 % CI, 1.046–4.107; P = 0.037) were the only factors associated with failure to identify ISM.
Conclusions
A large number of invasive colorectal cancers are at risk of being underdiagnosed as HGIN by biopsy-based pathology. The smaller the biopsy size, the less likely it is that the muscularis mucosae is included in the specimen. Also, in the more advanced or aggressive colorectal cancers, ISM is more likely to be missed on biopsy, which may be due to the destruction of the muscularis mucosae by more aggressive cancers.


Similar content being viewed by others
References
Colleypriest BJ, Marden PF, Linehan JD (2009) What is the optimal number of biopsies to diagnose a tumor found during colonoscopy? J Clin Gastroenterol 43:1012–1013
Rubio CA (2003) Gastrointestinal epithelial neoplasia. Gut 52:455–456
MacDonald AW, Tayyab M, Arsalani-Zadeh R, Hartley JE, Monson JR (2009) Intramucosal carcinoma on biopsy reliably predicts invasive colorectal cancer. Ann Surg Oncol 16:3267–3270
West AB, Mitsuhashi T (2005) Cancer or high-grade dysplasia? The present status of the application of the terms in colonic polyps. J Clin Gastroenterol 39:4–6
Hurlstone DP, Shorthouse AJ, Brown SR, Tiffin N, Cross SS (2008) Salvage endoscopic submucosal dissection for residual or local recurrent intraepithelial neoplasia in the colorectum: a prospective analysis. Colorectal Dis 10:891–897
Bujanda L, Cosme A, Gil I, Arenas-Mirave JI (2010) Malignant colorectal polyps. World J Gastroenterol 16:3103–3111
Cooper HS (2004) Intestinal neoplasms. In: Mills SE, Carter D, Greenson JK et al (eds) Sternberg’s diagnostic surgical pathology, 4th edn. Lippincott Williams & Wilkins, Philadelphia, pp 1543–1602
Hamilton SR, Aaltonen LA (eds) (2000) Pathology and genetics of tumours of the digestive system. World Health Organization classification of tumours. IARC Press, Lyon, pp 103–113
Dixon MF (2002) Gastrointestinal epithelial neoplasia: Vienna revisited. Gut 51:130–131
Schlemper RJ, Iwashita A (2004) Classification of gastrointestinal epithelial neoplasia. Curr Diagn Pathol 10:128–139
Wu W, Wu YL, Zhu YB et al (2009) Endoscopic features predictive of gastric cancer in superficial lesions with biopsy-proven high grade intraepithelial neoplasia. World J Gastroenterol 15:489–495
Tominaga K, Fujinuma S, Endo T, Saida Y, Takahashi K, Maetani I (2009) Efficacy of the revised Vienna Classification for diagnosing colorectal epithelial neoplasias. World J Gastroenterol 15:2351–2356
Chen LW, Yu BM, Zhang M, Fu J, Fei CS, Shen Y (2009) Diagnostic significance and management principles of colorectal intraepithelial neoplasia. Zhonghua Wai Ke Za Zhi 47:992–994
Livstone EM, Troncale FJ, Sheahan DG (1977) Value of a single forceps biopsy of colonic polyps. Gastroenterology 73:1296–1298
Pugliese V, Gatteschi B, Aste H et al (1981) Value of multiple forceps biopsies in assessing the malignant potential of colonic polyps. Tumori 67:57–62
Fenoglio CM, Kaye GI, Lane N (1973) Distribution of human colonic lymphatics in normal, hyperplastic, and adenomatous tissue. Its relationship to metastasis from small carcinomas in pedunculated adenomas, with two case reports. Gastroenterology 64:51–66
Hamilton SR, Aaltonen LA (2000) Pathology and genetics of tumours of the digestive system. IARC Press, Lyon, pp 105–119
Cerar A, Zidar N, Vodopivec B (2004) Colorectal carcinoma in endoscopic biopsies; additional histologic criteria for the diagnosis. Pathol Res Pract 200:657–662
Japanese Society for Cancer of the Colon and Rectum (1997) Japanese classification of colorectal carcinoma, 1st edn, Kanehara, Tokyo, pp 73-88
Machida H, Sano Y, Hamamoto Y et al (2004) Narrow-band imaging in the diagnosis of colorectal mucosal lesions: a pilot study. Endoscopy 36:1094–1098
Abdalla SA, Jeziorska M, Schofield P, Woolley DE, Haboubi NY (1997) Gelatinase B (MMP-9) expression and survival in colorectal cancer patients. Int J Colorectal Dis 12:342–343
Ban S, Kamada K, Mitsuki N et al (2000) Phenotypic change of muscularis mucosae in early invasive colorectal adenocarcinoma. J Clin Pathol 53:878–881
Ban S, Shimizu M (2009) Muscularis mucosae in desmoplastic stroma formation of early invasive rectal adenocarcinoma. World J Gastroenterol 15:4976–4979
Jeziorska M, Haboubi NY, Schofield PF, Ogata Y, Nagase H, Woolley DE (1994) Distribution of gelatinase B (MMP-9) and type IV collagen in colorectal carcinoma. Int J Colorectal Dis 9:141–148
Elmunzer BJ, Higgins PD, Kwon YM et al (2008) Jumbo forceps are superior to standard large-capacity forceps in obtaining diagnostically adequate inflammatory bowel disease surveillance biopsy specimens. Gastrointest Endosc 68:273–278
Morson BC (1974) Evolution of cancer of the colon and rectum. Proc Inst Med Chic 30:145–148
Schlemper RJ, Kato Y, Stolte M (2001) Review of histological classifications of gastrointestinal epithelial neoplasia: differences in diagnosis of early carcinomas between Japanese and Western pathologists. J Gastroenterol 36:445–456
Schlemper RJ, Kato Y, Stolte M (2000) Diagnostic criteria for gastrointestinal carcinomas in Japan and Western countries: proposal for a new classification system of gastrointestinal epithelial neoplasia. J Gastroenterol Hepatol 15:G49–G57
Conflict of interest
The authors declare that no conflict of interest exists.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wei, X.B., Gao, X.H., Wang, H. et al. More advanced or aggressive colorectal cancer is associated with a higher incidence of “high-grade intraepithelial neoplasia” on biopsy-based pathological examination. Tech Coloproctol 16, 277–283 (2012). https://doi.org/10.1007/s10151-012-0827-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-012-0827-4