Abstract
Background
The aim of this prospective study was to analyse the efficacy of Surgisis mesh for closure of rectovaginal fistulas. Prospective data were collected from two centres.
Methods
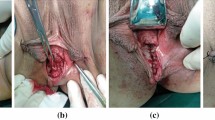
All patients with a rectovaginal fistula who underwent definitive surgery using Surgisis mesh were prospectively enrolled in this study. Inclusion criteria included a rectovaginal fistula in the lower two-thirds of the rectovaginal septum. Surgery was performed with a standardized technique including combined transrectal and transvaginal excision of the rectovaginal fistula with transvaginal placement of the mesh. Success was defined as closure of both internal and external (perianal and vaginal) openings, absence of drainage without further intervention, and no abscess formation.
Results
Over a period of 16 months, a total of 21 mesh procedures were performed in two centres. The mean age of the patients was 47 years (18–59 years). Of the 21 patients, 18 (86%) had recurrent rectovaginal fistula, and the mean number of prior attempts was 2.3 (0–8). The majority of patients (nine) had Crohn’s disease-associated fistula, followed by six with iatrogenic fistula, two with radiation-induced fistula, two with obstetric injuryinduced fistula, and two with idiopathic fistula. The mesh procedure was performed under faecal diversion in eight patients (38%). The mean operative time was 38 min; no intraoperative morbidity occurred. Patients were discharged from hospital on day 4. After a mean follow-up of 12 months (range, 3–18 months), the overall success rate after primary mesh procedure was 71% (15/21; 6 patients had failure or recurrence). All patients with failure or recurrence were reoperated upon. Out of these six patients who were reoperated upon, four had definite healing (75%). Among the eight patients who had faecal diversion, four (50%) had reversal of their stoma.
Conclusion
The preliminary success rate for this innovative technique using Surgisis mesh for the closure of rectovaginal fistulas is promising. Further studies are needed to assess the definite role of this novel technique in comparison to traditional surgical procedures
Similar content being viewed by others
References
Pye PK, Dada T, Duthie G et al (2004) Surgisis™ mesh: a novel approach to repair of a recurrent rectovaginal fistula. Dis Colon Rectum 47:1554–1556
Ellis CN (2008) Outcomes after repair of rectovaginal fistulas using bioprosthetics. Dis Colon Rectum 51:1084–1088
Saclarides TJ (2002) Rectovaginal fistula. Surg Clin North Am 82:1261–1272
Scott NA, Nair A, Hughes LE (1992) Anovaginal and rectovaginal fistula in patients with Crohn’s disease. Br J Surg 79:1379–1380
Levy C, Tremaine WJ (2002) Management of internal fistulas in Crohn’s disease. Inflamm Bowel Dis 8:106–111
Fry RD, Shemesh EI, Kodner IJ et al (1989) Techniques and results in the management of anal and perianal Crohn’s disease. Surg Gynecol Obstet 168:42–48
Lichtenstein GR (2000) Treatment of fistulizing Crohn’s disease. Gastroenterology 119:1132–1147
Greenwald JC, Hoexter B (1978) Repair of rectovaginal fistulas. Surg Gynecol Obstet 146:443–445
Cohen JL, Stricker JW, Schoetz DJ et al (1989) Rectovaginal fistula in Crohn’s disease. Dis Colon Rectum 32:825–828
Crim RW, Fazio VW, Laveri IC (1990) Rectal advancement flap repair in Crohn’s disease. Factors predictive of failure. Dis Colon Rectum 33:P3
Makowiec F, Jehle EC, Becker HD et al (1999) Clinical course after transanal advancement flap repair of perianal fistula in patients with Crohn’s disease. Br J Surg 82:603–606
Hull TL, Fazio VW (1997) Surgical approaches to low anovaginal fistula in Crohn’s disease. Am J Surg 173:95–98
Kodner IJ, Mazor A, Shemesh EI et al (1993) Endorectal advancement flap repair of rectovaginal and other complicated anorectal fistulas. Surgery 114:682–690
Sonoda T, Hull T, Piedmonte MR et al (2002) Outcomes of primary repair of anorectal and rectovaginal fistulas using the endorectal advancement flap. Dis Colon Rectum 45:1622–1628
Zimmerman DD, Gosselink MP, Briel JW et al (2002) The outcome of transanal advancement flap repair of rectovaginal fistulas is not improved by an additional labial fat transposition. Tech Coloproctol 6:37–42
Mizrahi N, Wexner SD, Zmora O et al (2002) Endorectal advancement flap: are there predictors of failure? Dis Colon Rectum 45:1616–1621
Sher ME, Bauer JJ, Gelernt I (1991) Surgical repair of rectovaginal fistulas in patients with Crohn’s disease: transvaginal approach. Dis Colon Rectum 34:641–648
Berman IR (1991) Sleeve advancement anorectoplasty for complicated anorectal/vaginal fistula. Dis Colon Rectum 34:1032–1037
Marchesa P, Hull TL, Fazio VW (1998) Advancement sleeve flaps for treatment of severe perianal Crohn’s disease. Br J Surg 85:1695–1698
Simmang CL, Lacey SW, Huber PJ (1998) Rectal sleeve advancement: repair of rectovaginal fistula associated with anorectal stricture in Crohn’s disease. Dis Colon Rectum 41:787–789
Joo JS, Weiss EG, Nogueras JJ et al (1998) Endorectal advancement flap in perianal Crohn’s disease. Am Surg 64:147–150
Onodera H, Nagayama S, Kohmoto I et al (2003) Novel surgical repair with bilateral gluteus muscle patching for intractable rectovaginal fistula. Tech Coloproctol 7:198–202
Chitrathara K, Namratha D, Francis V et al (2001) Spontaneous rectovaginal fistula and repair using bulbocavernosus muscle flap. Tech Coloproctol 5:47–49
Heyen F, Winslet MC, Andrews H et al (1989) Vaginal fistulas in Crohn’s disease. Dis Colon Rectum 32:379–383
Devesa JM, Devesa M, Velasco GR et al (2007) Benign rectovaginal fistulas: management and results of a personal series. Tech Coloproctol 11:128–134
Andreani SM, Dang HH, Grondona P et al (2007) Rectovaginal fistula in Crohn’s disease. Dis Colon Rectum 50:2215–2222
Hannaway CD, Hull TL (2008) Current considerations in the management of rectovaginal fistula from Crohn’s disease. Colorectal Dis 10:747–756
Shelton AA, Welton ML (2006) Transperineal repair of persistent rectovaginal fistulas using an acellular cadaveric dermal graft (AlloDerm). Dis Colon Rectum 49:1454–1457
Moore RD, Miklos JR, Kohli N (2004) Rectovaginal fistula repair using a porcine dermal graft. Obstet Gynecol 104:1165–1167
van Koperen PJ, Bemelman WA, Bossuyt PM et al (2008) The anal fistula plug versus the mucosal advancement flap for the treatment of anorectal fistula (PLUG trial). BMC Surg 8:11
Walfisch A, Zilberstein T, Walfisch S (2004) Rectovaginal septal repair: case presentations and introduction of a modified reconstruction technique. Tech Coloproctol 8:192–194
Fürst A, Schmidbauer C, Swol-Ben J et al (2008) Gracilis transposition for repair of recurrent anovaginal and rectovaginal fistulas in Crohn’s disease. Int J Colorectal Dis 23:349–353
Ruiz D, Bashankaev B, Speranaza J et al (2008) Graciloplasty for rectourethral, rectovaginal and rectovesical fistulas: technique overview, pitfalls and complications. Tech Coloproctol 12:277–281
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schwandner, O., Fuerst, A., Kunstreich, K. et al. Innovative technique for the closure of rectovaginal fistula using Surgisis™ mesh. Tech Coloproctol 13, 135–140 (2009). https://doi.org/10.1007/s10151-009-0470-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-009-0470-x