Abstract
Background
It is important to recognize regional and racial differences in drug efficacy and safety when performing multi-regional clinical trials (MRCTs). To understand regional differences, we compared the efficacy results in Japanese patients and the overall population in the MRCTs of anticancer drugs.
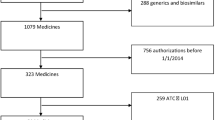
Methods
All new approvals of oncology drugs in Japan from January 2009 to December 2018 were searched using the Pharmaceuticals and Medical Devices Agency web site to find phase 3 MRCTs for the analysis. As the supporting data source, a literature search was performed in PubMed and Google Scholar. Linear regression analysis was performed and Pearson correlation coefficients (r) were calculated to compare the overall survival (OS), progression-free survival (PFS), and objective response rate (ORR) between Japanese patients and the overall population.
Results
Seventy MRCTs were identified. The correlation of hazard ratios (HRs) for OS between Japanese patients and the overall population was moderate (r = 0.45), and OS was 1.31 times longer in Japanese patients than in the overall population, although the correlation of median OS was strong (r = 0.91). The HRs for PFS were moderately correlated (r = 0.70) and the correlation of median PFS was strong (r = 0.90). The correlation of ORR was very strong (r = 0.96).
Conclusion
The PFS and ORR were consistent between Japanese patients and the overall population. A longer median OS was observed in Japanese patients. Our results would be a useful reference when planning and conducting MRCTs that include Japan for global simultaneous drug development.




Similar content being viewed by others
References
Hsiehchen D, Espinoza M, Hsieh A (2015) The cooperative landscape of multinational clinical trials. PLoS ONE. https://doi.org/10.1371/journal.pone.0130930
Hasegawa Y, Kawaguchi T, Kubo A et al (2011) Ethnic difference in hematological toxicity in patients with non-small cell lung cancer treated with chemotherapy a pooled analysis on Asian versus non-Asian in phase II and III. Thorac Oncol 11:1881–1888
Wang Z, Zhang N, Zhang C et al (2019) Effect of region on the outcome of patients receiving PD-1/PD-L1 inhibitors for advanced cancer. Int Immunopharmacol 74:105709
The International Council for Harmonization of Technical Requirements for Pharmaceuticals for Human Use (2016) General principles for planning and design of multi-regional clinical trials E17. Retrieved from https://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E17/E17_Step2.pdf. Accessed 05 Sept 2016
Pharmaceuticals and Medical Devices Agency (2007) Basic principles on global clinical trials (PMDA Notification No.0928010) Retrieved from https://www.pmda.go.jp/files/000157900.pdf
Saijo N, Fukuoka M, Thongpraser S et al (2010) Lung cancer working group report. Jpn J Clin Oncol 40(Suppl 1):i7–i12
Takashima A, Iizumi S, Boku N (2017) Survival after failure of first-line chemotherapy in advanced gastric cancer patients: differences between japan and the rest of the world. Jpn J Clin Oncol 47(7):583–589
Fukagai T, Namiki TS, Carlile RG et al (2006) Comparison of the clinical outcome after hormonal therapy for prostate cancer between Japanese and Caucasian men. BJU Int 97:1190–1193
PMDA website: https://www.pmda.go.jp/english/index.html
US National Library of Medicine (2018) Clinicaltrials.gov. Retrieved from https://www.clinicaltrials.gov
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458
Zhu AX, Park JO, Ryoo BY et al (2015) Ramucirumab versus placebo as second-line treatment in patients with advanced hepatocellular carcinoma following first-line therapy with sorafenib (REACH): a randomised, double-blind, multicentre, phase 3 trial. Lancet Oncol 16:859–870
Kudo M, Hatano E, Ohkawa S et al (2017) Ramucirumab as second-line treatment in patients with advanced hepatocellular carcinoma: Japanese subgroup analysis of the REACH trial. J Gastroenterol 52:494–503
Cainap C, Qin S, Huang WT et al (2015) Linifanib versus sorafenib in patients with advanced hepatocellular carcinoma: results of a randomized phase III trial. J Clin Oncol 33(2):172–179
Ioka T, Okusaka T, Ohkawa S et al (2015) Efficacy and safety of axitinib in combination with gemcitabine in advanced pancreatic cancer: subgroup analyses by region, including Japan, from the global randomized phase III trial. Jpn J Clin Oncol 45(5):439–448
Ohtsu A, Ajani JA, Bai YX et al (2013) Everolimus for previously treated advanced gastric cancer: results of the randomized, double-blind, phase III GRANITE-1 study. J Clin Oncol 31(31):3935–3943
Kimura G, Yonese J, Fukagai T et al (2016) Enzalutamide in Japanese patients with chemotherapy-naive, metastatic Castration-resistant prostate cancer: a post-hoc analysis of the placebo-controlled PREVAIL trial. Int J Urol 23:395–403
Xu RH, Muro K, Morita S et al (2018) Modified XELIRI (capecitabine plus irinotecan) versus FOLFIRI (leucovorin, fluorouracil, and irinotecan), both either with or without Bevacizumab, as second-line therapy for metastatic colorectal cancer (AXEPT): a multicentre, open-label, randomised, non-inferiority, phase 3 trial. Lancet Oncol 19:660–671
Kato T, Kagawa Y, Ota M et al (2018) Global phase III trial of comparing Mxeliri+BV Vs FOLFIRI+Bmab for 2nd line Mcrc (AXEPT) Japanese population analysis. Ann Oncol 29(Suppl 7):751–765
Shitara K, Doi T, Dvorkin M et al (2018) Trifluridine/tipiracil versus placebo in patients with heavily pretreated metastatic gastric cancer (TAGS): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol 19:1437–1448
Koizumi W, Kim YH, Fujii M et al (2014) Addition of docetaxel to S-1 without platinum prolongs survival of patients with advanced gastric cancer: a randomized study (START). J Cancer Res Clin Oncol 140:319–328
Tabernero J, Hoff PM, Shen L et al (2018) Pertuzumab plus trastuzumab and chemotherapy for HER2-positive metastatic gastric or gastro-oesophageal junction cancer (JACOB): final analysis of a double-blind, randomised, placebo-controlled phase 3 study. Lancet Oncol 19:1372–1384
Shaw AT, Kim TM, Crinò L et al (2017) Ceritinib versus chemotherapy in patients with ALK-rearranged non-small-cell lung cancer previously given chemotherapy and crizotinib (ASCEND-5): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol 18:874–886
Kiura K, Imamura F, Kagamu H et al (2018) Phase 3 study of ceritinib vs chemotherapy in ALK-rearranged NSCLC patients previously treated with chemotherapy and crizotinib (ASCEND-5): Japanese subset. Jpn J Clin Oncol 48(4):367–375
Kudo M, Han G, Finn RS et al (2014) Brivanib as adjuvant therapy to transarterial chemoembolization in patients with hepatocellular carcinoma: a randomized phase III trial. Hepatology 60(5):1697–1707
Katakami N, Felip E, Spigel DR et al (2017) A randomized, open-label, multicenter, phase 3 study to compare the efficacy and safety of Eribulin to treatment of physician’s choice in patients with advanced non-small cell lung cancer. Ann Oncol 28:2241–2247
Miles D, Cameron D, Bondarenko I et al (2017) Bevacizumab plus paclitaxel versus placebo plus paclitaxel as first-line therapy for HER2-negative metastatic breast cancer (Meridian): a double-blind placebo-controlled randomised phase III trial with prospective biomarker evaluation. Eur J Cancer 70:146–155
Masuda N, Takahashi M, Nakagami K et al (2017) First-line bevacizumab plus paclitaxel in Japanese patients with Her2-negative metastatic breast cancer: subgroup results from the randomized phase III meridian trial. Jpn J Clin Oncol 47(5):385–392
Kudo M, Cheng AL, Park JW et al (2018) Orantinib versus placebo combined with transcatheter arterial chemoembolisation in patients with unresectable hepatocellular carcinoma (ORIENTAL): a randomised, double-blind, placebo-controlled, multicentre, phase 3 study. Lancet Gastroenterol Hepatol 3:37–46
Gandara DR, Kawaguchi T, Crowley J et al (2009) Japanese-US common-arm analysis of paclitaxel plus carboplatin in advanced non-small-cell lung cancer: a model for assessing population-related pharmacogenomics. J Clin Oncol 27(21):3540–3546
Shigematsu H, Gazdar AF (2006) Somatic mutations of epidermal growth factor receptor signaling pathway in lung cancers. Int J Cancer 118:257–262
Soo RA, Loh M, Mok TS et al (2011) Ethnic differences in survival outcome in patients with advanced stage non-small cell lung cancer results of a meta-analysis of randomized controlled trials. J Thorac Oncol 6:1030–1038
Imai H, Kaira K, Minato K (2017) Clinical significance of post-progression survival in lung cancer. Thorac Cancer 8:379–386
Shimokawa M, Kogawa T, Shimada T et al (2018) Overall survival and post-progression survival are potent endpoint in phase III trials of second/third-line chemotherapy for advanced or recurrent epithelial ovarian cancer. J Cancer 9(5):872–879
Terashima T, Yamashita T, Toyama T et al (2019) Surrogacy of time to progression for overall survival in advanced hepatocellular carcinoma treated with systemic therapy: a systematic review and meta-analysis of randomized controlled trials. Liver Cancer 8:130–139
Kiyota N, Hasegawa Y, Takahashi S et al (2017) A randomized, open-label, phase III clinical trial of nivolumab vs. therapy of investigator’s choice in recurrent squamous cell carcinoma of the head and neck: a subanalysis of asian patients versus the global population in checkmate 141. Oral Oncol 73:138–146
Acknowledgements
We would like to thank Editage (https://www.editage.com) for English editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Toshiyuki Tamai is an employee of Eisai Co., Ltd.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Tamai, T., Kaneko, M. & Narukawa, M. Comparison of efficacy outcomes of anticancer drugs between Japanese patients and the overall population. Int J Clin Oncol 26, 296–304 (2021). https://doi.org/10.1007/s10147-020-01804-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-020-01804-9



