Abstract
Background
Risk factors for metachronous colorectal cancer (mCRC) in Lynch Syndrome (LS) patients are essential for colorectal cancer (CRC) treatment strategy to perform not only a curative but also preventive surgery. The aim of this study was to evaluate the risk factors for mCRC development in LS patients to define the patient subset that may benefit an extended curative and preventive surgical resection.
Methods
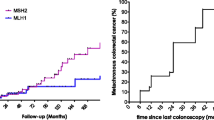
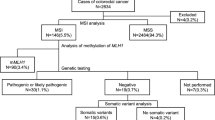
Patient’s clinical history, oncological, molecular and follow-up were collected retrospectively from the Hereditary Digestive Tumors Registry at the National Cancer Institute of Milan. The age-related cumulative risk of mCRC was calculated using the Kaplan–Meier method. Factors significantly associated with mCRC were analyzed with a Cox regression model. Overall and specific competitive risks were also calculated.
Results
In a total of 1346 CRC patients, 159 (11.8%) developed a mCRC after a mean follow-up of 138 months from the primary tumor. The independent risk factors reported by a multivariate analysis were: pathogenetic variants in MLH1 and MSH2 (HR 2.96 and 1.91, respectively) and history of colorectal adenomas (HR 1.54); whereas female sex and extended surgery were protective (HR 0.59 and 0.79, respectively).
Conclusions
Among a high-risk population for CRC, in particular LS, an extended surgery may be considered in CRC patients with specific risk factors (MLH1 or MSH2 germline pathogenic variants, history of colorectal adenomas) to reduce the risk of mCRC development.


Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Anele CC, Adegbola SO, Askari A et al (2017) Risk of metachronous colorectal cancer following colectomy in lynch syndrome: a systematic review and meta-analysis. Colorectal Dis 19(6):528–536. https://doi.org/10.1111/codi.13679
Renkonen-Sinisalo L, Seppala TT, Jarvinen HJ et al (2017) Subtotal colectomy for colon cancer reduces the need for subsequent surgery in lynch syndrome. Dis Colon Rectum 60(8):792–799. https://doi.org/10.1097/DCR.0000000000000802
Haanstra JF, de Vos Tot Nederveen Cappel WH, Gopie JP et al (2012) Quality of life after surgery for colon cancer in patients with lynch syndrome: partial versus subtotal colectomy. Dis Colon Rectum 55(6):653–659. https://doi.org/10.1097/DCR.0b013e31824f5392
Moertel CG, Bargen JA, Dockerty MB (1958) Multiple carcinomas of the large intestine: a review of the literature and a study of 261 cases. Gastroenterology 34(1):85–98
Bouvier AM, Latournerie M, Jooste V et al (2008) The lifelong risk of metachronous colorectal cancer justifies long-term colonoscopic follow-up. Eur J Cancer 44(4):522–527. https://doi.org/10.1016/j.ejca.2008.01.007
Kohlmann W, GS lynch syndrome. 2004 Feb 5 [Updated 2018 Apr 12]. In: Adam MP, Ardinger HH, Pagon RA et al (eds) GeneReviews® [Internet]. Seattle: University of Washington
Signoroni S, Tibiletti MG, Ricci MT et al (2019) Performance of tumor testing for Lynch syndrome identification in patients with colorectal cancer: a retrospective single-center study. Tumori 105(1):76–83. https://doi.org/10.1177/0300891618792460
Vasen HF, Moslein G, Alonso A et al (2010) Recommendations to improve identification of hereditary and familial colorectal cancer in Europe. Fam Cancer 9(2):109–115. https://doi.org/10.1007/s10689-009-9291-3
Lynch HT, Lanspa S, Smyrk T et al (1991) Hereditary nonpolyposis colorectal cancer (Lynch syndromes I & II). Genetics, pathology, natural history, and cancer control Part I. Cancer Genet Cytogenet 53(2):143–160
Provenzale D, Gupta S, Ahnen DJ et al (2018) NCCN guidelines insights: colorectal cancer screening, version 1.2018. J Natl Compr Canc Netw 16(8):939–949. https://doi.org/10.6004/jnccn.2018.0067
Bonadona V, Bonaiti B, Olschwang S et al (2011) Cancer risks associated with germline mutations in MLH1, MSH2, and MSH6 genes in Lynch syndrome. JAMA 305(22):2304–2310. https://doi.org/10.1001/jama.2011.743
Vasen HF, Blanco I, Aktan-Collan K et al (2013) Revised guidelines for the clinical management of Lynch syndrome (HNPCC): recommendations by a group of European experts. Gut 62(6):812–823. https://doi.org/10.1136/gutjnl-2012-304356
Syngal S, Brand RE, Church JM et al (2015) ACG clinical guideline: genetic testing and management of hereditary gastrointestinal cancer syndromes. Am J Gastroenterol 110(2):223–262. https://doi.org/10.1038/ajg.2014.435
Guillem JG, Wood WC, Moley JF et al (2006) ASCO/SSO review of current role of risk-reducing surgery in common hereditary cancer syndromes. Ann Surg Oncol 13(10):1296–1321. https://doi.org/10.1245/s10434-006-9036-6
Giardiello FM, Allen JI, Axilbund JE et al (2014) Guidelines on genetic evaluation and management of lynch syndrome: a consensus statement by the US multi-society task force on colorectal cancer. Am J Gastroenterol 109(8):1159–1179. https://doi.org/10.1038/ajg.2014.186
Heneghan HM, Martin ST, Winter DC (2015) Segmental vs extended colectomy in the management of hereditary nonpolyposis colorectal cancer: a systematic review and meta-analysis. Colorectal Dis 17(5):382–389. https://doi.org/10.1111/codi.12868
Malik SS, Lythgoe MP, McPhail M et al (2018) Metachronous colorectal cancer following segmental or extended colectomy in lynch syndrome: a systematic review and meta-analysis. Fam Cancer 17(4):557–564. https://doi.org/10.1007/s10689-017-0062-2
Umar A, Boland CR, Terdiman JP et al (2004) Revised Bethesda guidelines for hereditary nonpolyposis colorectal cancer (lynch syndrome) and microsatellite instability. J Natl Cancer Inst 96(4):261–268. https://doi.org/10.1093/jnci/djh034
Clark SK (2019) Management of genetically determined colorectal cancer. Surgeon 17(3):165–171. https://doi.org/10.1016/j.surge.2019.03.003
Kumarasinghe AP, de Boer B, Bateman AC et al (2010) DNA mismatch repair enzyme immunohistochemistry in colorectal cancer: a comparison of biopsy and resection material. Pathology 42(5):414–420. https://doi.org/10.3109/00313025.2010.493862
Shia JSZ, Weiser MR (2011) Immunohistochemical staining for DNA mismatch repair proteins in intestinal tract carcinoma: how reliable are biopsy samples? Am J Surg Pathol 35(3):447–454
Piozzi GN, Ricci MT, Signoroni S et al (2019) Ready, get set, go: fast preoperative genetic diagnosis is the present future in lynch syndrome surgical strategy. Dig Liver Dis. https://doi.org/10.1016/j.dld.2019.09.021
Moller P, Seppala T, Bernstein I et al (2017) Cancer incidence and survival in Lynch syndrome patients receiving colonoscopic and gynaecological surveillance: first report from the prospective lynch syndrome database. Gut 66(3):464–472. https://doi.org/10.1136/gutjnl-2015-309675
Kohlmann W, Gruber SB (1993) Lynch syndrome. In: Adam MP, Ardinger HH, Pagon RA et al. (eds) GeneReviews((R)). Seattle
Parry S, Win AK, Parry B et al (2011) Metachronous colorectal cancer risk for mismatch repair gene mutation carriers: the advantage of more extensive colon surgery. Gut 60(7):950–957. https://doi.org/10.1136/gut.2010.228056
Win AK, Parry S, Parry B et al (2013) Risk of metachronous colon cancer following surgery for rectal cancer in mismatch repair gene mutation carriers. Ann Surg Oncol 20(6):1829–1836. https://doi.org/10.1245/s10434-012-2858-5
Bogani G, Ricci MT, Vitellaro M et al (2019) Impact of gene-specific germline pathogenic variants on presentation of endometrial cancer in lynch syndrome. Int J Gynecol Cancer 29(4):705–710. https://doi.org/10.1136/ijgc-2019-000277
Jarvinen HJ, Aarnio M, Mustonen H et al (2000) Controlled 15-year trial on screening for colorectal cancer in families with hereditary nonpolyposis colorectal cancer. Gastroenterology 118(5):829–834
de Jong AE, Hendriks YM, Kleibeuker JH et al (2006) Decrease in mortality in lynch syndrome families because of surveillance. Gastroenterology 130(3):665–671. https://doi.org/10.1053/j.gastro.2005.11.032
Seppala TT, Ahadova A, Dominguez-Valentin M et al (2019) Lack of association between screening interval and cancer stage in lynch syndrome may be accounted for by over-diagnosis; a prospective lynch syndrome database report. Hered Cancer Clin Pract 17:8. https://doi.org/10.1186/s13053-019-0106-8
Engel C, Vasen HF, Seppala T et al (2018) No difference in colorectal cancer incidence or stage at detection by colonoscopy among 3 countries with different lynch syndrome surveillance policies. Gastroenterology 155(5):1400–1409. https://doi.org/10.1053/j.gastro.2018.07.030
Mecklin JP, Jarvinen HJ (1986) Clinical features of colorectal carcinoma in cancer family syndrome. Dis Colon Rectum 29(3):160–164
Jiang B, Ofshteyn A, Idrees JJ et al (2019) Total abdominal colectomy is cost-effective in treating colorectal cancer in patients with genetically diagnosed lynch syndrome. Am J Surg. https://doi.org/10.1016/j.amjsurg.2019.03.011
Ricci MT, Volorio S, Signoroni S et al (2019) Development, technical validation, and clinical application of a multigene panel for hereditary gastrointestinal cancer and polyposis. Tumori. https://doi.org/10.1177/0300891619847085
Dominguez-Valentin M, Sampson JR, Seppala TT et al (2019) Cancer risks by gene, age, and gender in 6350 carriers of pathogenic mismatch repair variants: findings from the prospective lynch syndrome database. Genet Med. https://doi.org/10.1038/s41436-019-0596-9
Acknowledgements
The authors wish to acknowledge and express sincere gratitude to Mariangela Di Ceglie and Ornella Galuppo from the Hereditary Digestive Tract Tumors Unit, for prospectively maintaining patient’s database.
Funding
No funding was received.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Alberto Morabito and Lucio Bertario are Retired from July 2014.
About this article
Cite this article
Signoroni, S., Piozzi, G.N., Ricci, M.T. et al. Risk factors for metachronous colorectal cancer in Lynch syndrome patients: a registry-based observational mono-institutional study cohort. Int J Clin Oncol 25, 1644–1652 (2020). https://doi.org/10.1007/s10147-020-01700-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-020-01700-2