Abstract
Background
The effectiveness of perioperative oral management in gastrointestinal surgery remains unclear. To elucidate the clinical significance of oral care, we investigated the relationship between the oral environment and postoperative infectious complications (POICs) in patients undergoing gastrointestinal surgery.
Methods
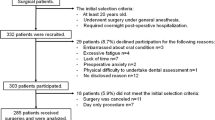
This was a single-institute and historical cohort study of 341 patients. The participants were isolated from consecutive patients undergoing planned radical resection for gastrointestinal carcinoma from January 2016 to June 2017. Dentists assessed the oral environment for periodontal disease, hygiene status, dry mouth, fur on tongue, and tooth stumps. All patients received scaling and tooth brushing instructions. A stepwise logistic regression analysis was conducted to identify risk factors for POICs among the different oral statuses.
Results
The surgical procedures performed were gastrectomy in 123 (36.1%), colorectal resection in 185 (54.2%), and pancreatoduodenectomy or others in 38 (11.1%). POICs occurred in 48 patients (14.1%), including deep organ space infection in 20, surgical site infection in 11, anastomotic leakage in 5, urinary tract infection in 4, pneumonia in 2, and others in 6. After adjusting for confounding factors, periodontal disease was isolated as an independent risk factor for POICs (odds ratio 2.091, p = 0.037, 95% confidence interval 1.045–4.183). Other variables of oral environment such as hygiene status, dry mouth, fur on tongue, and tooth stumps did not have a significant impact on POICs.
Conclusions
Periodontal disease is a risk factor for infectious complications after gastrointestinal surgery.
Similar content being viewed by others
References
Bergan EH, Tura BR, Lamas CC (2014) Impact of improvement in preoperative oral health on nosocomial pneumonia in a group of cardiac surgery patients: a single arm prospective intervention study. Intensive Care Med 40(1):23–31. https://doi.org/10.1007/s00134-013-3049-y
Spreadborough P, Lort S, Pasquali S et al (2016) A systematic review and meta-analysis of perioperative oral decontamination in patients undergoing major elective surgery. Perioperative medicine 5:6. https://doi.org/10.1186/s13741-016-0030-7
Sato J, Goto J, Harahashi A et al (2011) Oral health care reduces the risk of postoperative surgical site infection in inpatients with oral squamous cell carcinoma. Support Care Cancer 19(3):409–416. https://doi.org/10.1007/s00520-010-0853-6
Bebko SP, Green DM, Awad SS (2015) Effect of a preoperative decontamination protocol on surgical site infections in patients undergoing elective orthopedic surgery with hardware implantation. JAMA Surg 150(5):390–395. https://doi.org/10.1001/jamasurg.2014.3480
Wilson W, Taubert KA, Gewitz M et al (2007) Prevention of infective endocarditis: guidelines from the American Heart Association: a guideline from the American Heart Association Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee, Council on Cardiovascular Disease in the Young, and the Council on Clinical Cardiology, Council on Cardiovascular Surgery and Anesthesia, and the Quality of Care and Outcomes Research Interdisciplinary Working Group. Circulation 116(15):1736–1754. https://doi.org/10.1161/CIRCULATIONAHA.106.183095
Yoneyama T, Yoshida M, Matsui T et al (1999) Oral care and pneumonia. Oral Care Working Group. Lancet 354(9177):515
Wren SM, Martin M, Yoon JK et al (2010) Postoperative pneumonia-prevention program for the inpatient surgical ward. J Am Coll Surg 210(4):491–495. https://doi.org/10.1016/j.jamcollsurg.2010.01.009
Akutsu Y, Matsubara H, Shuto K et al (2010) Pre-operative dental brushing can reduce the risk of postoperative pneumonia in esophageal cancer patients. Surgery 147(4):497–502. https://doi.org/10.1016/j.surg.2009.10.048
Arimatsu K, Yamada H, Miyazawa H et al (2014) Oral pathobiont induces systemic inflammation and metabolic changes associated with alteration of gut microbiota. Sci Rep 4:4828. https://doi.org/10.1038/srep04828
Lockhart PB, Brennan MT, Thornhill M et al (2009) Poor oral hygiene as a risk factor for infective endocarditis-related bacteremia. J Am Dent Assoc 140(10):1238–1244
Nakatani S, Mitsutake K, Hozumi T et al (2003) Current characteristics of infective endocarditis in Japan: an analysis of 848 cases in 2000 and 2001. Circ J 67(11):901–905
Cotti E, Arrica M, Di Lenarda A et al (2017) The perioperative dental screening and management of patients undergoing cardiothoracic, vascular surgery and other cardiovascular invasive procedures: a systematic review. Eur J Prev Cardiol 24(4):409–425. https://doi.org/10.1177/2047487316682348
de Souza AF, Rocha AL, Castro WH (2016) Dental care before cardiac valve surgery: is it important to prevent infective endocarditis? Int J Cardiol Heart Vasc 12:57–62. https://doi.org/10.1016/j.ijcha.2016.07.001
Stansby G, Byrne MT, Hamilton G (1994) Dental infection in vascular surgical patients. Br J Surg 81(8):1119–1120
Silvestre FJ, Gil-Raga I, Martinez-Herrera M et al (2017) Prior oral conditions in patients undergoing heart valve surgery. J Clin Exp Dent 9(11):e1287–e1291. https://doi.org/10.4317/jced.53902
Salvi GE, Carollo-Bittel B, Lang NP (2008) Effects of diabetes mellitus on periodontal and peri-implant conditions: update on associations and risks. J Clin Periodontol 35(8 Suppl):398–409. https://doi.org/10.1111/j.1600-051X.2008.01282.x
Chavarry NG, Vettore MV, Sansone C et al (2009) The relationship between diabetes mellitus and destructive periodontal disease: a meta-analysis. Oral Health Prev Dent 7(2):107–127
Humphrey LL, Fu R, Buckley DI et al (2008) Periodontal disease and coronary heart disease incidence: a systematic review and meta-analysis. J Gen Intern Med 23(12):2079–2086. https://doi.org/10.1007/s11606-008-0787-6
Bahekar AA, Singh S, Saha S et al (2007) The prevalence and incidence of coronary heart disease is significantly increased in periodontitis: a meta-analysis. Am Heart J 154(5):830–837. https://doi.org/10.1016/j.ahj.2007.06.037
Yoneda M, Naka S, Nakano K et al (2012) Involvement of a periodontal pathogen, Porphyromonas gingivalis on the pathogenesis of non-alcoholic fatty liver disease. BMC Gastroenterol 12:16. https://doi.org/10.1186/1471-230X-12-16
Pischon N, Pischon T, Kroger J et al (2008) Association among rheumatoid arthritis, oral hygiene, and periodontitis. J Periodontol 79(6):979–986. https://doi.org/10.1902/jop.2008.070501
Page RC (1998) The pathobiology of periodontal diseases may affect systemic diseases: inversion of a paradigm. Ann Periodontol 3(1):108–120. https://doi.org/10.1902/annals.1998.3.1.108
Periodontology TJSo (2016) Clinical practice guideline for the periodontal treatment. 2015 The Japanese Society of Periodontology
Silness J, Loe H (1964) Periodontal disease in pregnancy. Ii. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand 22:121–135
Miyazaki H, Sakao S, Katoh Y et al (1995) Correlation between volatile sulphur compounds and certain oral health measurements in the general population. J Periodontol 66(8):679–684. https://doi.org/10.1902/jop.1995.66.8.679
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213
Oken MM, Creech RH, Tormey DC et al (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5(6):649–655
Sobin LH, Gospodarowicz MK, Wittekind C (2011) TNM Classification of Malignant Tumours, 7th edn. Wiley, New York
Organization WH (2008) WHO Report on the global tobacco epidemic 2008: the MPOWER Package. https://www.who.int/tobacco/mpower/mpower_report_full_2008.pdf. Accessed Aug 2017
Berrios-Torres SI, Umscheid CA, Bratzler DW et al (2017) Centers for disease control and prevention guideline for the prevention of surgical site infection. JAMA Surg 152(8):784–791. https://doi.org/10.1001/jamasurg.2017.0904
Tomas I, Diz P, Tobias A et al (2012) Periodontal health status and bacteraemia from daily oral activities: systematic review/meta-analysis. J Clin Periodontol 39(3):213–228. https://doi.org/10.1111/j.1600-051X.2011.01784.x
Lockhart PB, Brennan MT, Sasser HC et al (2008) Bacteremia associated with toothbrushing and dental extraction. Circulation 117(24):3118–3125. https://doi.org/10.1161/CIRCULATIONAHA.107.758524
Awano S, Ansai T, Takata Y et al (2008) Oral health and mortality risk from pneumonia in the elderly. J Dent Res 87(4):334–339. https://doi.org/10.1177/154405910808700418
Chiaki M, Kumiko K, Shouko K et al (2008) Preventive effects of postoperative pneumonia by thorough plaque control just before esophageal cancer operation. J Jpn Dent Hyg Assoc 2(2):43–47
Rickard AH, Gilbert P, High NJ et al (2003) Bacterial coaggregation: an integral process in the development of multi-species biofilms. Trends Microbiol 11(2):94–100
Ministry_of_Health_Labor_and_Welfare (2014). https://www.mhlw.go.jp/toukei/saikin/hw/kanja/14/dl/kanja-01.pdf. Accessed Aug 2017. Annal report of Patients' survey in Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No author has any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Nishikawa, M., Honda, M., Kimura, R. et al. Clinical impact of periodontal disease on postoperative complications in gastrointestinal cancer patients. Int J Clin Oncol 24, 1558–1564 (2019). https://doi.org/10.1007/s10147-019-01513-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-019-01513-y