Abstract
Purpose
We prospectively evaluated the 90-day postoperative mortality and morbidity of open radical cystectomy by using a standardized reporting methodology. Additionally, we assessed the preoperative characteristics to determine risk factors for major complications.
Methods
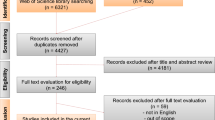
This multicenter prospective study included 185 consecutive patients undergoing open radical cystectomy from October 2010 through March 2014. Postoperative complications within 90 days were recorded and graded according to the modified Clavien–Dindo classification.
Results
Totally, 328 postoperative complications were observed in 149 patients (80.5%). Of these events, 73 (22.2%) were high grade (≥ Grade III), and developed in 46 patients (24.9%). Three patients (1.6%) died postoperatively. Urinary tract infection, wound complications, and paralytic ileus were common complications that occurred in 55 (29.7%), 42 (22.7%) and 41 (22.2%) patients, respectively. Ureteroenteric stricture was diagnosed in 13 of the 151 patients (8.6%) undergoing intestinal urinary diversion. Emergency room visits were required for 13 patients (7.0%) and readmission after discharge was needed for 36 (19.5%). A body mass index ≥ 25 kg/m2, smoking history and Charlson Comorbidity Index ≥ 2 were independent risk factors for high-grade complications, and their odds ratios (95% confidence intervals) were 2.357 (1.123–4.948), 2.843 (1.225–6.596) and 3.025 (1.390–6.596), respectively.
Conclusions
Open radical cystectomy is associated with a high incidence of postoperative complications. Most, however, are of low grade. Our results suggest that obesity, a smoking history, and increasing comorbidity are risk factors for major complications.
Similar content being viewed by others
Introduction
Radical cystectomy (RC) with lymph node dissection and urinary diversion (UD) is the gold standard treatment for patients with muscle-invasive bladder cancer or high-risk non-muscle invasive bladder cancer. With recent improvements of surgical procedures and perioperative care, the treatment-related morbidity and mortality rates have decreased during the last two decades [1]. However, RC remains one of the most invasive urological procedures in spite of these improvements.
Many studies have reported the postoperative morbidity and mortality rates of patients who undergo RC with UD [2,3,4,5,6,7,8,9,10]. The mortality and morbidity rates ranged from 0 to 9.0% and 30 to 70%, respectively, and varied widely among these reports. In a retrospective study using a care pathway in a cohort of 304 patients, the mortality rate was 0.3%, and overall major and minor complication rates were 4.9 and 30.9%, respectively [2]. Another large study including 1142 patients reported that the mortality and overall early complication rates were 2.7 and 67%, respectively [3]. This discrepancy may be explained by lack of standardized definitions of perioperative mortality and postoperative complications. In fact, there were differences in the definition of perioperative death among the reports, whether death due to cancer was included or not, and various follow-up periods such as 30 and 90 days were employed. Furthermore, most of these studies were done in a retrospective manner and might have underreported preoperative comorbidity and minor postoperative complications.
The demand for studies using standard definitions of complications, standard follow-up, and prospectively collected data is growing [11]. These are necessary for accumulation of evidence to create guidelines for postoperative management, better comparisons of different surgical techniques and counseling patients. Among various classifications of complications, the Clavien–Dindo classification (CDC) is applicable to most procedures for comprehensive surgical outcome assessment. To improve the quality of reporting on surgical complications, Martin et al. [12] proposed 10 criteria of ideal standard methods for reporting surgical complications, including methods of accruing data, the duration of follow-up, and outpatient information, as well as definitions of complications, mortality and morbidity, procedure-specific complications, severity grade, hospital stay and risk factors.
In this study, we prospectively evaluated the 90-day postoperative mortality and morbidity of open RC by using a standardized reporting methodology. Additionally, we assessed the preoperative characteristics to determine risk factors for major complications.
Materials and methods
Patient selection and assessment of data
From October 2010 through March 2014, 185 consecutive patients underwent open RC at Sapporo Medical University Hospital and 9 affiliate institutions participating in the Sapporo Medical University Urologic Oncology Consortium project. Patients who had received prior external beam radiotherapy were excluded from this study. Preoperative characteristics of the patients such as age, sex, BMI, ECOG-PS, the ASA score, Charlson Comorbidity Index (CCI) [13], smoking history, presence of hydronephrosis, serum creatinine and neoadjuvant chemotherapy were recorded prior to RC. BMI was calculated preoperatively according to the WHO guidelines, and divided into the following subgroups. The clinical stage and surgical parameters such as the operating time, intraoperative blood loss and transfusion requirement were recorded immediately after surgery. Pathological examination was performed by experienced pathologists at each institution according to the 2009 TNM classification. The postoperative complications were updated appropriately in a timely manner during the hospital stay. After discharge, the patients were told to come to the hospital where they had undergone surgery if they felt any change of their health status. Thus, complete information about complications was collected within a period of 90 days after surgery. This study was approved by the institutional review board of Sapporo Medical University (#20-84).
Preoperative and postoperative procedures
The standard procedure of RC including standard lymphadenectomy was performed for all patients. Lymphadenectomy included bilateral pelvic and at least bilateral common iliac lymph nodes. Urinary diversion types included ileal conduit, orthotopic neobladder and ureterocutaneostomy and percutaneous nephrostomy. Orthotopic neobladder substitution was performed by modified Studer methods with Nesbit anastomosis or the Le Duc-Camey anti-reflux method. Urethrectomy was indicated for male patients with high risk for urethral involvement or recurrence. In female patients, the uterus and ovaries were removed depending on age.
We adopted shared guidelines for preoperative and postoperative care including intravenous administration of antibiotic agents and parenteral nutrition. Briefly, only mechanical bowel preparation was performed the day before surgery. As prophylaxis for infection, antibiotics were intravenously administrated every 3 h and continued postoperatively for up to 2 days at the physicians’ discretion. A nasogastric tube was placed intraoperatively and removed immediately after surgery. Continuous lower thoracic epidural analgesia with local anesthetics was used for postoperative pain control if possible. Early postoperative feeding of semiliquid food was started on postoperative day 2, and then solid food was gradually introduced until resumption of a regular diet.
Definitions of complications
Postoperative mortality was defined as death from any cause occurring within 90 days after surgery. Postoperative complications within the same period were recorded and graded according to the modified CDC. We further grouped all complications into 11 categories as reported by the Memorial-Sloan Kettering Cancer Center [3]. Some common complications were defined in detail, including paralytic ileus, wound complications and urinary tract infection. Prolonged oral intake, the need for total parenteral nutrition and insertion of an ileus tube or a nasogastric tube again were considered to be paralytic ileus of Grade I, II and IIIa, respectively. Wound complications (surgical site infection and wound dehiscence) for which intravenous administration of antibiotics or an increase in the length of the hospital stay was needed were defined as Grade II. Wound dehiscence that needed resuture under local or general anesthesia and emergency operations for prolapse of visceral organs were defined as Grade III and IV, respectively. Most urinary tract infections requiring antibiotic chemotherapy were usually classified into Grade II, whereas complicated UTI associated with hydronephrosis needing nephrostomy or stenting, and sepsis were defined as Grade III and IV.
Statistical analysis
Univariate and multivariate logistic regression analyses were done to identify predictive factors of patients developing high-grade complications within 90 days after surgery. The following perioperative variables were categorized as risk factors: age, sex, BMI, a history of smoking, prior abdominal surgery, ECOG-PS, the ASA score, CCI, clinical T stage and neoadjuvant chemotherapy. A P value < 0.05 was considered statistically significant, and statistical analyses were performed using commercial software (SPSS version 16; IBM, Chicago, IL, USA).
Results
The patients’ clinical characteristics and perioperative outcomes are shown in Table 1. The median age was 72 years and the male-to-female ratio was approximately 4:1. The series included a few patients with impaired physical status such as a CCI ≥ 3 or ASA score ≥ 3. More than half of the patients had organ-confined disease. For three patients who had distant metastases at the time of operation, cystectomy was performed for the purpose of relieving severe symptoms such as continuing bleeding and bladder irritability. The regimen most often employed for neoadjuvant chemotherapy was gemcitabine plus cisplatin, which was carried out for approximately 20% of the patients. Ileal conduit was adopted for a large number of patients, whereas only a small number of patients underwent neobladder substitution as urinary diversion. The decision on the type of urinary diversion was affected by physicians’ and patients’ preferences in addition to medical contraindications for neobladder substitution such as positive cancer in the prostatic urethra.
Tables 2 and 3 show all of the postoperative complications observed within 90 days after surgery in this study according to category. A total of 328 postoperative complications of any CDC grade were observed in 149 patients (80.5%). The mean number of complications per patient was 1.8 and high-grade (Grade III or more) complications developed in 46 patients (24.9%). Urinary tract infection was the most common complication, and affected 55 patients (29.7%), followed by wound complications in 42 (22.7%) and paralytic ileus in 41 (22.2%). Ureteroenteric stricture was diagnosed in 13 of the 151 patients (8.6%) who underwent intestinal urinary diversion. Constipation, increased serum creatinine and delirium were observed in 21 (11.4%), 20 (10.8%) and 15 (8.1%) patients, respectively, almost all of which were Grade II or less. Emergency room visits were required for 13 patients (7.0%) and readmission after discharge was needed for 36 patients (19.5%).
The results of univariate and multivariate logistic regression analyses to determine the preoperative risk factors for high-grade intra- and postoperative complications are shown in Table 4. In univariate analysis, BMI ≥ 25 kg/m2, a smoking history and CCI ≥ 2 were significant risk factors. All of them were independent risk factors for high-grade complications associated with RC. The remaining variables, age, sex, the ASA score, tumor stage and neoadjuvant chemotherapy, had no significant association with the incidence of high-grade complications. There is no significant difference in morbidity and mortality rate between continent and incontinent UD groups. The overall mortality rate within 90 days after surgery was 1.6%. The details of the patients who died within 90 days after RC are shown in Table 5. One patient died of tumor progression and liver insufficiency within 30 days of surgery. Palliative radical cystectomy was originally planned for her with the purpose of controlling bladder bleeding and severe anemia. Another patient died of pulmonary embolism on postoperative day 7. Before that, he developed wound dehiscence (Grade IIIb) and underwent an emergency operation for wound closure on postoperative day 3. The other patient developed paralytic ileus, sepsis, renal insufficiency, delirium and wound complications, and died of heart failure at 2 months after surgery. He was only 61 years old and preoperatively had no sign of heart disease.
Discussion
RC is a representative general surgical procedure in urology associated with high invasiveness that may contribute to relatively high mortality and morbidity. A European group conducted a multicenter prospective observational study of 679 patients who underwent RC. In their study, the mortality rate within 90 days was 9.0% [8]. They found that clinically node-positive disease and distant metastatic disease were independent risk factors for perioperative mortality, which suggests that they included a significant number of cancer-related deaths. This may account for their higher mortality rate. On the other hand, although the rate of major complications was similar, our series had a much higher overall complication rate than their study [14]. Not only a difference in races, but also differences in hospital volume (median 49 cystectomies per year) and perioperative management might have affected the different incidences of minor complications.
Several studies have reported the impact of comorbidities on postoperative complications after RC. A population-based study by Abdollah et al. showed that the CCI was a statistically significant predictor of postoperative mortality [7]. Furthermore, Mayr et al. assessed the impacts of four comorbidity indices, the ASA score, ACE-27, CCI and ECOG PS, on perioperative mortality within 90 days after RC, all of which were shown to be independent predictors [5]. In a retrospective study using the ACE-27 as a comorbidity instrument, Fairey et al. [15] concluded that increasing comorbidity was independently associated with an increased risk of 90-day mortality and postoperative complications after RC. Furthermore, in a study by Roghmann et al. using a standardized methodology, both the CCI and BMI were significant risk factors for high-grade complications [9].
The BMI and a history of smoking were also independent risk factors for postoperative complications in the current study. Several investigators have reported the negative impacts of the BMI on operative and postoperative courses. Lee et al. [16] observed that the BMI was correlated with the perioperative complication rate, estimated blood loss and operative time. In our series, particularly, ileus and wound trouble accounted for a large number of postoperative complications. Several reports showed that the rate of postoperative ileus was associated with the BMI [17, 18]. Associations between the BMI and wound trouble such as surgical site infection and wound dehiscence in abdominal surgery are well reported [19, 20]. Furthermore, smoking is also a well-known risk factor for surgical site infection. On the other hand, ureteric anastomotic stenosis has not been reported to be directly associated with the BMI or smoking. It may be associated with other factors such as the type of anastomosis and urinary tract infection [21]. Interestingly, however, Richards et al. reported that the incidence of grade III or higher postoperative complications within 30 days after RC was an independent risk factor for ureteric anastomotic stenosis [22]. As discussed in other reports, patients with high BMIs tend to have more postoperative complications, suggesting a potential association between a high BMI and the incidence of ureteric anastomotic stenosis. Moreover, ureteral anastomotic leakage was the other reported risk factor for ureteric anastomotic stenosis [22]. It is well known that smoking induces tissue ischemia, leading to anastomotic leakage in gastrointestinal tract surgery, suggesting that smoking also potentially induces ureteral anastomotic leakage, which can lead to anastomotic stenosis [23, 24].
Current guidelines recommend that a continent UD should be offered to all patients without specific contraindications. There are controversies whether the type of UD influences postoperative morbidity and mortality after RC. In general, continent diversion (such as ileal neobladder) might include higher morbidity rates due to its complicated procedure. However, in the present study, no significant difference in morbidity and mortality rate between continent and incontinent UD groups was observed. This result is supported by other studies. In a prospective large study from a European tertiary center, the risk of postoperative complications did not vary according to UD type. Abe et al. [25] reported that there was no significant difference in the overall morbidity rate, although the patients with ileal neobladder had more infectious complications. A matched pair analysis in Korean series also showed no difference in 30- and 90-day morbidity and mortality [26].
The median postoperative hospital stay in our series was longer than in a cohort in the USA, but similar to that of large series in Japan [6] and that of one in Italy [27]. However, the length of hospital stay is strongly influenced by the healthcare system of each country and the individual hospital policy.
There has been a growing acceptance of minimally invasive surgery such as laparoscopic (LRC) and robot-assisted laparoscopic radical cystectomy (RARC). However, a recent systematic review concluded that RARC had a lower 90-day rate of complications of any grade, whereas the high-grade complication and mortality rates were similar to those of open RC, although RARC can be performed safely [28]. Some prospective studies showed that there were no significant differences in 90-day postoperative complication rates between open RC and RARC, although RARC provided possible benefits such as reducing intraoperative blood loss, inpatient narcotic requirements and time to regular diet [29, 30]. Furthermore, a recent randomized controlled trial from an experienced high-volume cancer center failed to identify a definite advantage of RARC over open RC and reported similar complication rates, lengths of hospital stay and short-term QOL outcomes in the two groups, although RARC had a significantly lower intraoperative blood loss [31]. To clarify the possible advantages of LRC/RARC with regard to postoperative complications, further studies with larger sample sizes and standardized assessment of complications are needed. LRC/RARC is already widespread due to its potential lesser invasiveness and many surgeons are trying to improve the technique. Therefore another randomized controlled study to compare the outcomes of open RC and LRC/RAPC might be infeasible in the present circumstances and the outcomes of LRC/RAPC should be verified by comparison with reported results of open RC as a control. However, most studies about open RC do not meet the criteria for reports of surgical complications [32] because they do not report the definitions of complications, the grade/severity, outpatient data, comorbidities and the duration of the reporting period, which are essential to improve the quality of surgical complication reporting. In addition, Lawrentschuk et al. [11] found that standard definitions of complications, standard follow-up, and prospectively collected data were needed to create evidence-based guidelines and improve postoperative outcomes of RC. The present study may have significant value because of its use of a standardized reporting methodology advocated by Martin et al. [12] and prospective assessment.
Our study has some limitations. First, although data were collected prospectively, the number of patients was small. This may have resulted in the failure to identify some potential risk factors predicting complications. Second, despite the application of the CDC, the complication grading had potential interobserver biases. Nevertheless, our study has the special strength of prospective collection of data, where the categories and severities of postoperative complications were defined in advance of surgery and complications were reported immediately after their incidence.
In conclusion, although open RC is associated with significant morbidity, most of the complications are minor. Because obesity, increasing comorbidity and a history of smoking might be associated with high-grade complications, we should be aware of these risk factors and inform patients of them before surgery.
References
Rosario DJ, Becker M, Anderson JB (2000) The changing pattern of mortality and morbidity from radical cystectomy. BJU Int 85:427–430
Chang SS, Cookson MS, Baumgartner RG et al (2002) Analysis of early complications after radical cystectomy: results of a collaborative care pathway. J Urol 167:2012–2016
Shabsigh A, Korets R, Vora KC et al (2009) Defining early morbidity of radical cystectomy for patients with bladder cancer using a standardized reporting methodology. Eur Urol 55:164–176
Svatek RS, Fisher MB, Matin SF et al (2010) Risk factor analysis in a contemporary cystectomy cohort using standardized reporting methodology and adverse event criteria. J Urol 183:929–934
Mayr R, May M, Martini T et al (2012) Predictive capacity of four comorbidity indices estimating perioperative mortality after radical cystectomy for urothelial carcinoma of the bladder. BJU Int 110:E222–E227
Takada N, Abe T, Shinohara N et al (2012) Peri-operative morbidity and mortality related to radical cystectomy: a multi-institutional retrospective study in Japan. BJU Int 110:E756–E764
Abdollah F, Sun M, Schmitges J et al (2012) Development and validation of a reference table for prediction of postoperative mortality rate in patients treated with radical cystectomy: a population-based study. Ann Surg Oncol 19:309–317
Aziz A, May M, Burger M et al (2014) Prediction of 90-day mortality after radical cystectomy for bladder cancer in a prospective European multicenter cohort. Eur Urol 66:156–163
Roghmann F, Trinh QD, Braun K et al (2014) Standardized assessment of complications in a contemporary series of European patients undergoing radical cystectomy. Int J Urol 21:143–149
Novotny V, Froehner M, Koch R et al (2016) Age, American Society of Anesthesiologists physical status classification and Charlson score are independent predictors of 90-day mortality after radical cystectomy. World J Urol 34:11231129
Lawrentschuk N, Colombo R, Hakenberg OW et al (2010) Prevention and management of complications following radical cystectomy for bladder cancer. Eur Urol 57:983–1001
Martin RCG, Brennan MF, Jaques DP (2002) Quality of complication reporting in the surgical literature. Ann Surg 235:803–813
Charlson ME, Pompei P, Ales KL et al (1987) A new method of classifying prognostic co-morbidity in longitudinal-studies—development and validation. J Chronic Dis 40:373–383
Schmid M, Rink M, Traumann M et al (2015) Evidence from the ‘PROspective MulticEnTer RadIcal Cystectomy Series 2011 (PROMETRICS 2011)’ Study: how are preoperative patient characteristics associated with urinary diversion type after radical cystectomy for bladder cancer? Ann Surg Oncol 22:1032–1042
Fairey A, Chetner M, Metcalfe J et al (2008) Associations among age, comorbidity and clinical outocomes after radical cystectomy; results from the Alberta Urology Institute Radical Cystectomy Database. J Urol 180:128–134
Lee CT, Dunn RL, Chen BT et al (2004) Impact of body mass index on radical cystectomy. J Urol 172:1281–1285
Svatek RS, Fisher MB, Williams MB et al (2010) Age and body mass index are independent risk factors for the development of postoperative paralytic ileus after radical cystectomy. Urology 76:1419–1424
Ramirez JA, McIntosh AG, Strehlow R et al (2013) Definition, incidence, risk factors, and prevention of paralytic ileus following radical cystectomy: a systematic review. Eur Urol 64:588–597
Mullen JT, Davenport DL, Hutter MM et al (2008) Impact of body mass index on perioperative outcomes in patients undergoing major intra-abdominal cancer surgery. Ann Surg Oncol 15:2164–2172
de Blacam C, Ogunleye AA, Momoh AO et al (2012) High body mass index and smoking predict morbidity in breast cancer surgery a multivariate analysis of 26,988 patients from the national surgical quality improvement program database. Ann Surg 255:551–555
Large MC, Cohn JA, Kiriluk KJ et al (2013) The impact of running versus interrupted anastomosis on ureterointestinal stricture rate after radical cystectomy. J Urol 190:923–927
Richards KA, Cohn JA, Large MC et al (2015) The effect of length of ureteral resection on benign ureterointestinal stricture rate in ileal conduit or ileal neobladder urinary diversion following radical cystectomy. Urol Oncol 33(65):e1–e8
Fawcett A, Shembekar M, Church JS et al (1996) Smoking, hypertension, and colonic anastomotic healing; a combined clinical and histopathological study. Gut 38:714–718
Sorensen LT, Jorgensen T, Kirkeby LT et al (1999) Smoking and alcohol abuse are major risk factors for anastomotic leakage in colorectal surgery. Br J Surg 86:927–931
Abe T, Takada N, Shinohara N et al (2014) Comparison of 90-day complications between ileal conduit and neobladder reconstruction after radical cystectomy: a retrospective multi-institutional study in Japan. Int J Urol 21:554–559
Kim SH, Yu A, Jung JH et al (2014) Incidence and risk factors of 30-day early and 90-day late morbidity and mortality of radical cystectomy during a 13-year follow-up: a comparative propensity-score matched analysis of complications between neobladder and ileal conduit. Jpn J Clin Oncol 44:677–685
Novara G, De Marco V, Aragona M et al (2009) Complications and mortality after radical cystectomy for bladder transitional cell cancer. J Urol 182:914–921
Novara G, Catto JWF, Wilson T et al (2015) Systematic review and cumulative analysis of perioperative outcomes and complications after robot-assisted radical cystectomy. Eur Urol 67:376–401
Khan MS, Gan C, Ahmed K et al (2016) A single-centre early phase randomised controlled three-arm trial of open, robotic, and laparoscopic radical cystectomy (CORAL). Eur Urol 69:613–621
Nix J, Smith A, Kurpad R et al (2010) Prospective randomized controlled trial of robotic versus open radical cystectomy for bladder cancer: perioperative and pathologic results. Eur Urol 57:196–201
Bochner BH, Dalbagni G, Sjoberg DD et al (2015) Comparing open radical cystectomy and robot-assisted laparoscopic radical cystectomy: a randomized clinical trial. Eur Urol 67:1042–1050
Donat SM (2007) Standards for surgical complication reporting in urologic oncology: time for a change. Urology 69:221–225
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
About this article
Cite this article
Hirobe, M., Tanaka, T., Shindo, T. et al. Complications within 90 days after radical cystectomy for bladder cancer: results of a multicenter prospective study in Japan. Int J Clin Oncol 23, 734–741 (2018). https://doi.org/10.1007/s10147-018-1245-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-018-1245-z