Abstract
Objective
Intracranial haemorrhage (ICH) is associated with permanent neurological disability resulting in deterioration of the quality of life (QoL). Our study assesses QoL in patients with ruptured arteriovenous malformation (AVM) in long-term follow-up at least five years after ICH and compares their QoL with the QoL of patient with non-ruptured AVM.
Methods
Using the Quality of Life Scale (QOLS), the Patient Health Questionnaire (PHQ-9) for depressive symptoms, and the socioeconomic status (SES), a prospective assessment was performed. The modified Rankin Scale (mRS) was assessed for outcome.
Results
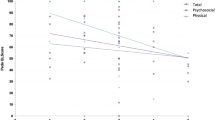
Of 73 patients, 42 (57.5%) had ruptured (group 1) and 31 (42.5%) a non-ruptured AVM (group 2). Mean follow-up time was 8.6 ± 3.9 years (8.5 ± 4.2 years in group 1 and 8.9 ± 3.7 years in group 2). Favourable outcome (mRS 0–1) was assessed in 60 (83.3%) and unfavourable in 12 (16.7%) patients. Thirty-one of 42 patients (73.8%) in group 1 and 29 of 30 patients in group 2 (96.7%) had favourable outcomes. Mean QOLS was 85.6 ± 14.1 (group 1 86.1 ± 15.9, group 2 84.9 ± 11.4). Patients in group 1 did not show a significant difference in QoL compared to patients in group 2 (p = 0.23). Additional analyses in group 2 (rho = − 0.73; p < 0.01) and in untreated AVM patients (rho = − 0.81; p < 0.01) showed a strong correlation between QOLS and PHQ-9.
Conclusion
Long-term follow-up showed no difference in the QoL between patients with and without ICH caused by brain AVM. Outcome- and QoL-scores were high in both groups. Further studies are necessary to evaluate depression and anxiety symptoms in patients with AVM.


Similar content being viewed by others
Availability of data and materials
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Ahlsiö B, Britton M, Murray V, Theorell T (1984) Disablement and quality of life after stroke. Stroke 15(5):886–890. https://doi.org/10.1161/01.STR.15.5.886
Al-Shahi R, Warlow C (2001) A systematic review of the frequency and prognosis of arteriovenous malformations of the brain in adults. Brain 124(Pt 10):1900–1926. https://doi.org/10.1093/brain/124.10.1900
Angermeyer MC, Holzinger A, Matschinger H, Stengler-Wenzke K (2002) Depression and quality of life: results of a follow-up study. Int J Soc Psychiatry 48(3):189–99. https://doi.org/10.1177/002076402128783235
Bielderman A, de Greef MHG, Krijnen WP, van der Schans CP (2015) Relationship between socioeconomic status and quality of life in older adults: a path analysis. Qual Life Res 24(7):1697–1705. https://doi.org/10.1007/s11136-014-0898-y
Burckhardt CS, Anderson KL (2003) The Quality of Life Scale (QOLS): reliability, validity, and utilization. Health Qual Life Outcomes 23(1):60. https://doi.org/10.1186/1477-7525-1-60
Carod-Artal FJ, Egido JA (2009) Quality of life after stroke: the importance of a good recovery. Cerebrovasc Dis 27 Suppl 1:204–214. https://doi.org/10.1159/000200461
Cenzato M, Boccardi E, Beghi E, Vajkoczy P, Szikora I, Motti E, Morgan MK (2017) European consensus conference on unruptured brain AVMs treatment (supported by EANS, ESMINT, EGKS, and SINCH). Acta Neurochir 159(6):1059–1064. https://doi.org/10.1007/s00701-017-3154-8
Chen CJ, Ding D, Derdeyn CP, Lanzino G, Friedlander RM, Southerland AM, Sheehan JP et al (2020) Brain arteriovenous malformations: a review of natural history, pathobiology, and interventions. Neurology 95(20):917–927. https://doi.org/10.1212/WNL.0000000000010968
Choi JH, Mast H, Sciacca RR, Hartmann A, Khaw AV, Mohr JP et al (2006) Clinical outcome after first and recurrent hemorrhage in patients with untreated brain arteriovenous malformation. Stroke 37(5):1243–1247. https://doi.org/10.1161/01.STR.0000217970.18319.7d
Dalton A, Dobson G, Prasad M, Mukerji N (2018) De novo intracerebral arteriovenous malformations and a review of the theories of their formation. Br J Neurosurg 32(3):305–311. https://doi.org/10.1080/02688697.2018.1478060
Dinc N, Platz J, Tritt S, Quick-Weller J, Eibach M, Wolff R et al (2018) Posterior fossa AVMs: increased risk of bleeding and worse outcome compared to supratentorial AVMs. J Clin Neurosci 53:171–176. https://doi.org/10.3171/2009.2.FOCUS0914
Dinc N, Won S-Y, Brawanski N, Eibach M, Quick-Weller J, Konczalla J et al (2019) Differences in bleeding patterns and outcome after intracerebral hemorrhage due to vascular malformations. PLoS ONE 14(5):e0217017. https://doi.org/10.1371/journal.pone.0217017
Dinc N, Won S-Y, Eibach M, Gessler F, Konczalla J, Quick-Weller J et al (2019) The extent of neurologic improvement and social life in young patients with ruptured and unruptured brain AVM: a long-term follow-up. World Neurosurg 127:e503–e508. https://doi.org/10.1016/j.wneu.2019.03.187
Dinc N, Won S-Y, Quick-Weller J, Berkefeld J, Seifert V, Marquardt G (2019) Prognostic variables and outcome in relation to different bleeding patterns in arteriovenous malformations. Neurosurg Rev 42(3):731–736. https://doi.org/10.1007/s10143-019-01091-7
Haraldstad K, Wahl A, Andenæs R, Andersen JR, Andersen MH, Beisland E et al (2019) A systematic review of quality of life research in medicine and health sciences. Qual Life Res 28(10):2641–2650. https://doi.org/10.1007/s11136-019-02214-9
JieAnNaMu, Xu X, You H, Gu H, Gu J, Li X et al (2020) Inequalities in health-related quality of life and the contribution from socioeconomic status: evidence from Tibet, China. BMC Public Health 20(1):630. https://doi.org/10.1186/s12889-020-08790-7
Jonkman EJ, de Weerd AW, Vrijens NL (1998) Quality of life after a first ischemic stroke. Long-term developments and correlations with changes in neurological deficit, mood and cognitive impairment. Acta Neurol Scand 98(3):169–75. https://doi.org/10.1111/j.1600-0404.1998.tb07289.x
King RB (1996) Quality of life after stroke. Stroke 27(9):1467–72. https://doi.org/10.1161/01.STR.27.9.1467
Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16(9):606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Kwa VI, Limburg M, de Haan RJ (1996) The role of cognitive impairment in the quality of life after ischaemic stroke. J Neurol 243(8):599–604. https://doi.org/10.1007/BF00900948
Lai EHP, Lun SLC (2002) Impact on the quality of life of patients with arteriovenous malformations during the latent interval between gamma knife radiosurgery and lesion obliteration. J Neurosurg 97(5 Suppl):471–473. https://doi.org/10.3171/jns.2002.97.supplement_5.0471
Lampert T, Kroll LE, Müters S, Stolzenberg H (2012) Messung des sozioökonomischen Status in der Studie „Gesundheit in Deutschland aktuell“ (GEDA). [cited 2021 Jun 6]; Available from: https://edoc.rki.de/handle/176904/1750
Lampert T, Kroll LE, von der Lippe E, Müters S, Stolzenberg H (2013) Sozioökonomischer Status und Gesundheit: Ergebnisse der Studie zur Gesundheit Erwachsener in Deutschland (DEGS1). Bundesgesundheitsbl 56(5–6):814–821
Lo Buono V, Bonanno L, Corallo F, Sidoti A, Bramanti P, Marino S (2016) Evaluation of qualitative outcomes after surgical intervention on patients affected by arteriovenous malformations. J Stroke Cerebrovasc Dis 25(12):2947–2952. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.08.010
Lo Buono V, Corallo F, Bramanti P, Marino S (2017) Coping strategies and health-related quality of life after stroke. J Health Psychol 22(1):16–28. https://doi.org/10.1177/1359105315595117
Lombardo L, Shaw R, Sayles K, Altschul D (2020) Anxiety and depression in patients who undergo a cerebrovascular procedure. BMC Neurol 20(1):1–6. https://doi.org/10.1186/s12883-020-01674-8
Manea L, Gilbody S, McMillan D (2015) A diagnostic meta-analysis of the Patient Health Questionnaire-9 (PHQ-9) algorithm scoring method as a screen for depression. Gen Hosp Psychiatry 37(1):67–75. https://doi.org/10.1016/j.genhosppsych.2014.09.009
Mast H, Young WL, Koennecke HC, Sciacca RR, Osipov A, Pile-Spellman J et al (1997) Risk of spontaneous haemorrhage after diagnosis of cerebral arteriovenous malformation. Lancet 350(9084):1065–8. https://doi.org/10.1016/S0140-6736(97)05390-7
Nikolaev SI, Vetiska S, Bonilla X, Boudreau E, Jauhiainen S, Rezai Jahrom B, Radovanovic I et al (2018) Somatic activating KRAS mutations in arteriovenous malformations of the brain. N Engl J Med 378(3):250–261. https://doi.org/10.1056/NEJMoa1709449
Noble AJ, Baisch S, Mendelow AD, Allen L, Kane P, Schenk T (2008) Posttraumatic stress disorder explains reduced quality of life in subarachnoid hemorrhage patients in both the short and long term. Neurosurgery 63(6):1095–104; discussion 1004-1005. https://doi.org/10.1227/01.NEU.0000327580.91345.78
Noble AJ, Schenk T (2010) Which variables help explain the poor health-related quality of life after subarachnoid hemorrhage? A meta-analysis. Neurosurgery 66(4):772–783. https://doi.org/10.1227/01.NEU.0000367548.63164.B2
Offenbächer M, Sauer S, Kohls N, Waltz M, Schoeps P (2012) Quality of life in patients with fibromyalgia: validation and psychometric properties of the German Quality of Life Scale (QOLS-G). Rheumatol Int 32(10):3243–3252. https://doi.org/10.1007/s00296-011-2184-4
Orosz P, Vadász Á, Veres DS, Berentei Z, Gubucz I, Nardai S et al (2021) Living with a brain AVM: a quality of life assessment. Acta Neurochir Suppl 132:71–76. https://doi.org/10.1007/978-3-030-63453-7_10
Pohjola A, Oulasvirta E, Roine R, Sintonen HP, Hafez A, Koroknay-Pál P, Laakso A (2021) Comparing health-related quality of life in modified Rankin Scale grades: 15D results from 323 patients with brain arteriovenous malformation and population controls. Acta Neurochir 163(7):2037–2046. https://doi.org/10.1007/s00701-021-04847-7
Pohjola A, Oulasvirta E, Roine RP, Sintonen HP, Hafez A, Koroknay-Pál P et al (2019) Long-term health-related quality of life in 262 patients with brain arteriovenous malformation. Neurology 93(14):e1374-84. https://doi.org/10.1212/WNL.0000000000008196
Ramos-Lima MJM, Brasileiro I de C, de Lima TL, Braga-Neto P (2018) Quality of life after stroke: impact of clinical and sociodemographic factors. Clinics (Sao Paulo) 73:e418. https://doi.org/10.6061/clinics/2017/e418
Rohn B, Haenggi D, Etminan N, Kunz M, Turowski B, Steiger HJ (2014) Epilepsy, headache, and quality of life after resection of cerebral arteriovenous malformations. J Neurol Surg A Cent Eur Neurosurg 75(4):282–288
Rohn B, Hänggi D, Etminan N, Turowski B, Steiger HJ (2017) Relief of epilepsy and headache and quality of life after microsurgical treatment of unruptured brain AVM-audit of a single-center series and comprehensive review of the literature. Neurosurg Rev 40(1):59–65. https://doi.org/10.1007/s10143-016-0750-7
Spetzler RF, Martin NA (1986) A proposed grading system for arteriovenous malformations. J Neurosurg 65(4):476–483. https://doi.org/10.3171/jns.1986.65.4.0476
Spetzler RF, Ponce FA (2011) A 3-tier classification of cerebral arteriovenous malformations. J Neurosurg 114(3):842–849. https://doi.org/10.3171/2010.8.JNS10663
Tatemichi TK, Desmond DW, Stern Y, Paik M, Sano M, Bagiella E (1994) Cognitive impairment after stroke: frequency, patterns, and relationship to functional abilities. J Neurol Neurosurg Psychiatry 57(2):202–207. https://doi.org/10.1136/jnnp.57.2.202
van Beijnum J, Lovelock CE, Cordonnier C, Rothwell PM, Klijn CJM, Al-Shahi Salman R et al (2009) Outcome after spontaneous and arteriovenous malformation-related intracerebral haemorrhage: population-based studies. Brain 132(Pt 2):537–543. https://doi.org/10.1093/brain/awn318
Van den Bussche, Berger K, Kemper C et al (2010) Inzidenz, Rezidiv, Pflegebedürftigkeit und Mortalität von Schlaganfall. Aktuelle Neurol 37(03):131–135
van der Schaaf IC, Brilstra EH, Rinkel GJE, Bossuyt PM, van Gijn J (2002) Quality of life, anxiety, and depression in patients with an untreated intracranial aneurysm or arteriovenous malformation. Stroke 33(2):440–443. https://doi.org/10.1161/hs0202.102335
von Vogelsang A-C, Thelin EP, Hakim R, Svensson M (2017) Health-related quality of life dynamics 2 years following aneurysmal subarachnoid hemorrhage: a prospective cohort study using EQ-5D. Neurosurgery 81(4):650–8. https://doi.org/10.1227/NEU.0b013e3182804686
Yang SY, Paek SH, Kim DG, Chung HT (2012) Quality of life after radiosurgery for cerebral arteriovenous malformation patients who present with seizure. Eur J Neurol 19(7):984–991. https://doi.org/10.1111/j.1468-1331.2012.03664.x
Acknowledgements
The authors thank Marina Heibel for her support during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Lina Benhassine. The first draft of the manuscript was written by Lina Benhassine, and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
LB — concept development, data collection, provided and cared for study patients, data interpretation as well as the below-listed contributions.
ND — concept development and substantial involvement in the development of the draft manuscript.
SYW, NF, GM, ÜB — contributed important intellectual content, served as scientific advisers.
GM, VS, MK, SYW, CS, MC, MAK — critical review of the study proposal and final approval.
All the authors agreed to be accountable for all aspects of the work for accuracy and are committed to the integrity of the final product.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were following the ethical standards of the institutional committee (University Hospital Frankfurt am Main) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study protocol was reviewed and approved by the ethics committee at University Hospital Frankfurt am Main, approval number 136/19.
Consent to participate
Written informed consent for participation was obtained from all study participants before their inclusion in the study.
Consent for publication
Written informed consent for publication was obtained from all study participants before their inclusion in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The study was registered prospectively on 7 July 2019, trial registration number: DRKS00017409.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Benhassine, L., Won, SY., Filmann, N. et al. Long-term follow-up in patients with brain arteriovenous malformation based on the Quality of Life Scale and socioeconomic status. Neurosurg Rev 45, 3281–3290 (2022). https://doi.org/10.1007/s10143-022-01847-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-022-01847-8