Abstract
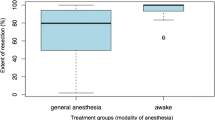
To assess feasibility and safety of function-based resection under awake conditions for solitary brain metastasis patients. Retrospective, observational, single-institution case-control study (2014-2019). Inclusion criteria are adult patients, solitary brain metastasis, supratentorial location within eloquent areas, and function-based awake resection. Case matching (1:1) criteria between metastasis group and control group (high-grade gliomas) are sex, tumor location, tumor volume, preoperative Karnofsky Performance Status score, age, and educational level. Twenty patients were included. Intraoperatively, all patients were cooperative; no obstacles precluded the procedure from being performed. A positive functional mapping was achieved at both cortical and subcortical levels, allowing for a function-based resection in all patients. The case-matched analysis showed that intraoperative and postoperative events were similar, except for a shorter duration of the surgery (p<0.001) and of the awake phase (p<0.001) in the metastasis group. A total resection was performed in 18 cases (90%, including 10 supramarginal resections), and a partial resection was performed in two cases (10%). At three months postoperative months, none of the patients had worsening of their neurological condition or uncontrolled seizures, three patients had an improvement in their seizure control, and seven patients had a Karnofsky Performance Status score increase ≥10 points. Function-based resection under awake conditions preserving the brain connectivity is feasible and safe in the specific population of solitary brain metastasis patients and allows for high resection rates within eloquent brain areas while preserving the overall and neurological condition of the patients. Awake craniotomy should be considered to optimize outcomes in brain metastases in eloquent areas.

Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
References
Arita H, Narita Y, Miyakita Y, Ohno M, Sumi M, Shibui S (2014) Risk factors for early death after surgery in patients with brain metastases: reevaluation of the indications for and role of surgery. J Neurooncol. 116:145–152. https://doi.org/10.1007/s11060-013-1273-5
Barbizet J, Duizabo P (1985) Abrégés de médecine. Neuropsychologie, 3ème éditi. Masson
Brown PD, Ballman KV, Cerhan JH, Anderson SK, Carrero XW, Whitton AC, Greenspoon J, Parney IF, Laack NNI, Ashman JB, Bahary JP, Hadjipanayis CG, Urbanic JJ, Barker FG II, Farace E, Khuntia D, Giannini C, Buckner JC, Galanis E, Roberge D (2017) Postoperative stereotactic radiosurgery compared with whole brain radiotherapy for resected metastatic brain disease (NCCTG N107C/CEC·3): a multicentre, randomised, controlled, phase 3 trial. Lancet Oncol 18(8):1049–1060
Chua TH, See AAQ, Ang BT, King NKK (2018) Awake craniotomy for resection of brain metastases: a systematic review. World Neurosurg 120:e1128–e1135
De Benedictis A, Moritz-Gasser S, Duffau H (2010) Awake mapping optimizes the extent of resection for low-grade gliomas in eloquent areas. Neurosurgery. 66:1074–1084. https://doi.org/10.1227/01.NEU.0000369514.74284.78
Duffau H (2018) Diffuse low-grade glioma, oncological outcome and quality of life: a surgical perspective. Curr Opin Oncol. 30:383–389. https://doi.org/10.1097/CCO.0000000000000483
Groshev A, Padalia D, Patel S, Garcia-Getting R, Sahebjam S, Forsyth PA, Vrionis FD, Etame AB (2017) Clinical outcomes from maximum-safe resection of primary and metastatic brain tumors using awake craniotomy. Clin Neurol Neurosurg 157:25–30
Herbet G, Rigaux-Viodé O, Moritz-Gasser S (2017) Peri- and intraoperative cognitive and language assessment for surgical resection in brain eloquent structures. Neurochirurgie. 63:135–141. https://doi.org/10.1016/j.neuchi.2016.10.011
Kamp MA, Dibué M, Niemann L, Reichelt DC, Felsberg J, Steiger H-J, Szelényi A, Rapp M, Sabel M (2012) Proof of principle: supramarginal resection of cerebral metastases in eloquent brain areas. Acta Neurochir (Wien) 154(11):1981–1986
Kamp MA, Rapp M, Slotty PJ, Turowski B, Sadat H, Smuga M, Dibué-Adjei M, Steiger H-J, Szelényi A, Sabel M (2015) Incidence of local in-brain progression after supramarginal resection of cerebral metastases. Acta Neurochir (Wien) 157(6):905–911
Metellus P, Pallud J, Ram Z, Watts C, Westphal M (2020) Surgery in brain metastasis management: therapeutic, diagnostic, and strategic considerations. In: Cent. Nerv. Syst. Metastases. Springer International Publishing, Cham, pp 183–190
Meyer FB, Bates LM, Goerss SJ, Friedman JA, Windschitl WL, Duffy JR, Perkins WJ, O’Neill BP (2001) Awake craniotomy for aggressive resection of primary gliomas located in eloquent brain. Mayo Clin Proc. 76:677–687. https://doi.org/10.4065/76.7.677
Mintz A, Perry J, Spithoff K, Chambers A, Laperriere N (2007) Management of single brain metastasis: a practice guideline. Curr Oncol. 14:131–143. https://doi.org/10.3747/co.2007.129
Muto J, Dezamis E, Rigaux-Viode O, Peeters S, Roux A, Zanello M, Mellerio C, Sauvageon X, Varlet P, Oppenheim C, Pallud J (2018) Functional-based resection does not worsen quality of life in patients with a diffuse low-grade glioma involving eloquent brain regions: a prospective cohort study. World Neurosurg. 113:e200–e212. https://doi.org/10.1016/j.wneu.2018.01.213
Neves S, Mazal PR, Wanschitz J, Rudnay AC, Drlicek M, Czech T, Wüstinger C, Budka H (2001) Pseudogliomatous growth pattern of anaplastic small cell carcinomas metastatic to the brain. Clin. Neuropathol.
Pallud J, Mandonnet E, Corns R, Dezamis E, Parraga E, Zanello M, Spena G (2017) Technical principles of direct bipolar electrostimulation for cortical and subcortical mapping in awake craniotomy. Neurochirurgie. 63:158–163. https://doi.org/10.1016/j.neuchi.2016.12.004
Pallud J, Rigaux-Viode O, Corns R, Muto J, Lopez Lopez C, Mellerio C, Sauvageon X, Dezamis E (2017) Direct electrical bipolar electrostimulation for functional cortical and subcortical cerebral mapping in awake craniotomy. Practical considerations. Neurochirurgie 63(3):164–174
Patchell RA, Tibbs PA, Walsh JW, Dempsey RJ, Maruyama Y, Kryscio RJ, Markesbery WR, Macdonald JS, Young B (1990) A randomized trial of surgery in the treatment of single metastases to the brain. N Engl J Med 322(8):494–500
Rossi M, Ambrogi F, Gay L et al (2019) Is supratotal resection achievable in low-grade gliomas? Feasibility, putative factors, safety, and functional outcome. J Neurosurg 132(June):1–14
Sanai N, Mirzadeh Z, Berger MS (2008) Functional outcome after language mapping for glioma resection. N Engl J Med 358(1):18–27
Sanmillan JL, Fernández-Coello A, Fernández-Conejero I, Plans G, Gabarrós A (2017) Functional approach using intraoperative brain mapping and neurophysiological monitoring for the surgical treatment of brain metastases in the central region. J Neurosurg 126(3):698–707
Sawaya R, Hammoud M, Schoppa D, Hess KR, Wu SZ, Shi W-M, WiIdrick DM (1998) Neurosurgical outcomes in a modern series of 400 craniotomies for treatment of parenchymal tumors. Neurosurgery 42(5):1044–1055
Schackert G, Lindner C, Petschke S, Leimert M, Kirsch M (2013) Retrospective study of 127 surgically treated patients with multiple brain metastases: Indication, prognostic factors, and outcome. Acta Neurochir (Wien). 155:379–387. https://doi.org/10.1007/s00701-012-1606-8
Soffietti R, Cornu P, Delattre JY, Grant R, Graus F, Grisold W, Heimans J, Hildebrand J, Hoskin P, Kalljo M, Krauseneck P, Marosi C, Siegal T, Vecht C (2006) EFNS Guidelines on diagnosis and treatment of brain metastases: report of an EFNS Task Force. Eur J Neurol. 13:674–681. https://doi.org/10.1111/j.1468-1331.2006.01506.x
Soffietti R, Abacioglu U, Baumert B, Combs SE, Kinhult S, Kros JM, Marosi C, Metellus P, Radbruch A, Villa Freixa SS, Brada M, Carapella CM, Preusser M, le Rhun E, Rudà R, Tonn JC, Weber DC, Weller M (2017) Diagnosis and treatment of brain metastases from solid tumors: guidelines from the European Association of neuro-oncology (EANO). Neuro Oncol 19(2):162–174
Telera S, Fabi A, Pace A, Vidiri A, Anelli V, Carapella CM, Marucci L, Crispo F, Sperduti I, Pompili A (2013) Radionecrosis induced by stereotactic radiosurgery of brain metastases: results of surgery and outcome of disease. J Neurooncol. 113:313–325. https://doi.org/10.1007/s11060-013-1120-8
Yoo H, Kim YZ, Nam BH, Shin SH, Yang HS, Lee JS, Zo JI, Lee SH (2009) Reduced local recurrence of a single brain metastasis through microscopic total resection: clinical article. J Neurosurg 110(4):730–736
Zanello M, Roux A, Zah-Bi G, Trancart B, Parraga E, Edjlali M, Tauziede-Espariat A, Sauvageon X, Sharshar T, Oppenheim C, Varlet P, Dezamis E, Pallud J (2020) Predictors of early postoperative epileptic seizures after awake surgery in supratentorial diffuse gliomas. J Neurosurg.:1–10. https://doi.org/10.3171/2020.1.jns192774
Acknowledgments
The authors gratefully acknowledge the following (in alphabetical order): the surgical neuro-oncology team, and particularly Alissia Basquin-Sanz, Odile Rigaux-Viodé, and Sylvie Sicot; the department of Neurosurgery; the department of Neuropathology, and particularly Pascale Varlet; the department of Neuroradiology, and particularly Joseph Benzakoun, Olivier Naggara, Catherine Oppenheim and Jean-François Meder; the department of Neurophysiology, and particularly Martine Gavaret and Angela Marchi; the department of neuro-anesthesia and neuro-intensive care, and particularly Abderrezak Akhrouf, Roland Benichou, Serge Biou, Mathieu Daniel, Hortense Dumontier, Aurélie Gruner, Aurélien Mazeraud, Alain Monpetit, Xavier Sauvageon, Caroline Schimpf, Alain Sermet, Tarek Sharshar, and Gilles Thouvenot; the neuro-oncology unit of the Gustave Roussy University Hospital, Villejuif, France, and particularly Sarah Dumont.
Author information
Authors and Affiliations
Contributions
JBP, AM, BT, ME, EL, ATE, ED, and JP did the data collection. JBP, AM, and JP did the data analysis. JBP, AM, MZ, AR, SP, BT, ME, EL, ATE, GZB, EP, FC, ED, FD, and JP did the data interpretation. JBP, AM, SP, and JP wrote the report. JBP, AM, MZ, AR, SP, BT, ME, EL, ATE, GZB, EP, FC, ED, FD, and JP reviewed and approved the paper.
Corresponding author
Ethics declarations
Ethics approval
This study received approval (IRB#1: 2020/10) from the institutional review board (IRB00011687).
Consent to participate
Due to the retrospective nature of the study no consent was obtained.
Consent for publication
Due to the retrospective nature of the study no consent was obtained.
Conflict of interest
The authors have no conflict of interest to disclose.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Pelletier, JB., Moiraghi, A., Zanello, M. et al. Is function-based resection using intraoperative awake brain mapping feasible and safe for solitary brain metastases within eloquent areas?. Neurosurg Rev 44, 3399–3410 (2021). https://doi.org/10.1007/s10143-021-01504-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-021-01504-6