Abstract
Ruptured intracranial aneurysms, as the leading cause of spontaneous subarachnoid hemorrhage (aSAH), represents an emergency with high morbi-mortality. The comprehension of the underlying pathology that involves inflammatory and immune responses, through the neutrophil-to-lymphocyte ratio (NLR), could help to predict complications such as delayed cerebral ischemia (DCI) or rebleeding and the functional outcome. Systematic review of English-based literature through PubMed and Biblioteca Vitural em Saúde (BVS) to find papers discussing the use of NLR in the aSAH setting. Area-under-curve (AUC) of receiver operating characteristics (ROC), cutoff value, sensitivity, and specificity were retrieved. From 53 articles included, 4 papers were evaluated after exclusion criteria. Rebleeding could be predicted with a NLR cutoff value of 9.88 (sensitivity 72.3%, specificity 63.3%). The mean cutoff value for DCI was 12.85, with sensitivity 66.3% and specificity 75.8%. Finally, a worse 3-month functional outcome could be predicted with a mean sensitivity of 73.3% and a mean specificity of 54%. NLR is a new issue in scientific community, especially neurosurgery. The current understanding points to a multifactorial process after aSAH that emerges as alterations on the NLR. As a measurement readily available and cost-effect after admission of the patient, its use signals that patients that need expedite surgical treatment or more aggressive treatment for vasospasm. As other medical subspecialties already use this ratio to predict outcomes, the literature reviewed by this paper constitute the earliest clues that higher NLR predicts re-bleeding, DCI, and functional outcome.

Similar content being viewed by others
Data availability
Not applicable
References
Dumont AS, Dumont RJ, Chow MM, Lin C, Calisaneller T, Ley KF, Kassell NF, Lee KS (2003) Cerebral vasospasm after subarachnoid hemorrhage: putative role of inflammation. Neurosurgery 53:123–135. https://doi.org/10.1227/01.NEU.0000068863.37133.9E
Suarez JI, Tarr RW, Selman WR (2006) Aneurysmal subarachnoid hemorrhage. N Engl J Med 354:387–396
Kassell NF, Sasaki T, Colohan AR, Nazar G (1985) Cerebral vasospasm following aneurysmal subarachnoid hemorrhage. Stroke 16:562–572. https://doi.org/10.1161/01.STR.16.4.562
Weir B, Macdonald RL, Stoodley M (1999) Etiology of cerebral vasospasm. Acta Neurochir Suppl 1999:27–46. https://doi.org/10.1007/978-3-7091-6377-1_3
Feigin VL, Rinkel GJE, Lawes CMM, Algra A, Bennett DA, van Gijn J, Anderson CS (2005) Risk factors for subarachnoid hemorrhage: an updated systematic review of epidemiological studies. Stroke 36:2773–2780
Rosenørn J, Eskesen V, Schmidt K, Espersen JO, Haase J, Harmsen A, Hein O, Knudsen V, Midholm S, Marcussen E, Rasmussen P, Rønde F, Voldby B, Hansen L (1987) Clinical features and outcome in 1076 patients with ruptured intracranial saccular aneurysms: A prospective consecutive study. Br J Neurosurg 1:33–45. https://doi.org/10.3109/02688698709034339
Suzuki S, Iwabuchi T, Tanaka T, Kanayama S, Ottomo M, Hatanaka M, Aihara H (1985) Prevention of cerebral vasospasm with OKY-046 an imidazole derivative and a thromboxane synthetase inhibitor. A preliminary co-operative clinical study. Acta Neurochir 77:133–141. https://doi.org/10.1007/BF01476216
Cataudella E, Giraffa CM, di Marca S, Pulvirenti A, Alaimo S, Pisano M, Terranova V, Corriere T, Ronsisvalle ML, di Quattro R, Stancanelli B, Giordano M, Vancheri C, Malatino L (2017) Neutrophil-to-lymphocyte ratio: an emerging marker predicting prognosis in elderly adults with community-acquired pneumonia. J Am Geriatr Soc 65:1796–1801. https://doi.org/10.1111/jgs.14894
Dong CH, Wang ZM, Chen SY (2018) Neutrophil to lymphocyte ratio predict mortality and major adverse cardiac events in acute coronary syndrome: A systematic review and meta-analysis. Clin Biochem 52:131–136. https://doi.org/10.1016/j.clinbiochem.2017.11.008
Zheng J, Cai J, Li H, Zeng K, He L, Fu H, Zhang J, Chen L, Yao J, Zhang Y, Yang Y (2017) Neutrophil to lymphocyte ratio and platelet to lymphocyte ratio as prognostic predictors for hepatocellular carcinoma patients with various treatments: a meta-analysis and systematic review. Cell Physiol Biochem 44:967–981. https://doi.org/10.1159/000485396
Mitsuya K, Nakasu Y, Kurakane T, Hayashi N, Harada H, Nozaki K (2017) Elevated preoperative neutrophil-to-lymphocyte ratio as a predictor of worse survival after resection in patients with brain metastasis. J Neurosurg 127:433–437. https://doi.org/10.3171/2016.8.JNS16899
Tao C, Hu X, Wang J, Ma J, Li H, You C (2017) Admission neutrophil count and neutrophil to lymphocyte ratio predict 90-day outcome in intracerebral hemorrhage. Biomark Med 11:33–42. https://doi.org/10.2217/bmm-2016-0187
Weng W, Chen X, Gong S, Guo L, Zhang X (2018) Preoperative neutrophil–lymphocyte ratio correlated with glioma grading and glioblastoma survival. Neurol Res 40:917–922. https://doi.org/10.1080/01616412.2018.1497271
Moher D, Liberati A, Tetzlaff J, Altman DG, Altman D, Antes G, Atkins D, Barbour V, Barrowman N, Berlin JA, Clark J, Clarke M, Cook D, D’Amico R, Deeks JJ, Devereaux PJ, Dickersin K, Egger M, Ernst E, Gøtzsche PC, Grimshaw J, Guyatt G, Higgins J, Ioannidis JPA, Kleijnen J, Lang T, Magrini N, McNamee D, Moja L, Mulrow C, Napoli M, Oxman A, Pham B, Rennie D, Sampson M, Schulz KF, Shekelle PG, Tovey D, Tugwell P (2009) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 6:6. https://doi.org/10.1371/journal.pmed.1000097
Wang J-Y, Zhang X-T, Wang J-Q, Wang C-Y, Zheng W-L, Pan Z-M, Xu Z-B, Li X-Y, Zhang Y-B (2020) Admission neutrophil-lymphocyte ratio predicts rebleeding following aneurismal subarachnoid hemorrhage. World Neurosurg 138:e317–e322. https://doi.org/10.1016/j.wneu.2020.02.112
Wu Y, He Q, Wei Y, Zhu J, He Z, Zhang X, Guo Z, Xu R, Cheng C, Huang Z, Sun X (2019) The association of neutrophil-to-lymphocyte ratio and delayed cerebral ischemia in patients with aneurysmal subarachnoid hemorrhage: possible involvement of cerebral blood perfusion. Neuropsychiatr Dis Treat 15:1001–1007. https://doi.org/10.2147/NDT.S190477
Tao C, Wang J, Hu X, Ma J, Li H, You C (2017) Clinical value of neutrophil to lymphocyte and platelet to lymphocyte ratio after aneurysmal subarachnoid hemorrhage. Neurocrit Care 26:393–401. https://doi.org/10.1007/s12028-016-0332-0
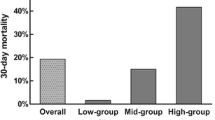
Giede-Jeppe A, Reichl J, Sprügel MI, Lücking H, Hoelter P, Eyüpoglu IY, Kuramatsu JB, Huttner HB, Gerner ST (2019) Neutrophil-to-lymphocyte ratio as an independent predictor for unfavorable functional outcome in aneurysmal subarachnoid hemorrhage. J Neurosurg 132:400–407. https://doi.org/10.3171/2018.9.JNS181975
Celikbilek A, Ismailogullari S, Zararsiz G (2014) Neutrophil to lymphocyte ratio predicts poor prognosis in ischemic cerebrovascular disease. J Clin Lab Anal 28:27–31. https://doi.org/10.1002/jcla.21639
Fang YN, Tong MS, Sung PH, Chen YL, Chen CH, Tsai NW, Huang CJ, Chang YT, Chen SF, Chang WN, Lu CH, Yip HK (2017) Higher neutrophil counts and neutrophil-to-lymphocyte ratio predict prognostic outcomes in patients after non-atrial fibrillation-caused ischemic stroke. Biom J 40:154–162. https://doi.org/10.1016/j.bj.2017.03.002
Tokgoz S, Keskin S, Kayrak M, Seyithanoglu A, Ogmegul A (2014) Is neutrophil/lymphocyte ratio predict to short-term mortality in acute cerebral infarct independently from infarct volume? J Stroke Cerebrovasc Dis 23:2163–2168. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.04.007
Jamali SA, Turnbull MT, Kanekiyo T, Vishnu P, Zubair AC, Raper CC, Tawk RG, Freeman WD (2020) Elevated neutrophil-lymphocyte ratio is predictive of poor outcomes following aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis 29:104631. https://doi.org/10.1016/j.jstrokecerebrovasdis.2019.104631
Lattanzi S, Cagnetti C, Provinciali L, Silvestrini M (2016) Neutrophil-to-lymphocyte ratio predicts the outcome of acute intracerebral hemorrhage. Stroke. 47:1654–1657. https://doi.org/10.1161/STROKEAHA.116.013627
Xue J, Huang W, Chen X, Li Q, Cai Z, Yu T, Shao B (2017) Neutrophil-to-lymphocyte ratio is a prognostic marker in acute ischemic stroke. J Stroke Cerebrovasc Dis 26:650–657. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.11.010
Chalouhi N, Ali MS, Jabbour PM, Tjoumakaris SI, Gonzalez LF, Rosenwasser RH, Koch WJ, Dumont AS (2012) Biology of intracranial aneurysms: role of inflammation. J Cereb Blood Flow Metab 32:1659–1676
Fennell VS, Kalani MYS, Atwal G, Martirosyan NL, Spetzler RF (2016) Biology of saccular cerebral aneurysms: a review of current understanding and future directions. Front Surg 3:25
Sawyer DM, Amenta PS, Medel R, Dumont AS (2015) Inflammatory mediators in vascular disease: identifying promising targets for intracranial aneurysm research. Mediat Inflamm 2015:896283–896210. https://doi.org/10.1155/2015/896283
Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, Fang MC, Fisher M, Furie KL, Heck DV, Johnston SC, Kasner SE, Kittner SJ, Mitchell PH, Rich MW, Richardson D, Schwamm LH, Wilson JA (2014) Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 45:2160–2236. https://doi.org/10.1161/STR.0000000000000024
Bhat T, Teli S, Rijal J, Bhat H, Raza M, Khoueiry G, Meghani M, Akhtar M, Costantino T (2013) Neutrophil to lymphocyte ratio and cardiovascular diseases: A review. Expert Rev Cardiovasc Ther 11:55–59
Melo MCA, Garcia RF, de Araújo CFC, Abreu RLC, de Bruin PFC, de Bruin VMS (2019) Clinical significance of neutrophil-lymphocyte and platelet-lymphocyte ratios in bipolar patients: an 18-month prospective study. Psychiatry Res 271:8–14. https://doi.org/10.1016/j.psychres.2018.10.077
Tanık VO, Çınar T, Velibey Y, Öz A, Kalenderoğlu K, Gümüşdağ A, Aruğaslan E, Keskin M, Eren M (2019) Neutrophil-to-lymphocyte ratio predicts contrast-induced acute kidney injury in patients with st-elevation myocardial infarction treated with primary percutaneous coronary intervention. J Tehran Heart Cent 14:59–66
Jabbarli R, Gläsker S, Weber J, Taschner C, Olschewski M, van Velthoven V (2013) Predictors of severity of cerebral vasospasm caused by aneurysmal subarachnoid hemorrhage. J Stroke Cerebrovasc Dis 22:1332–1339. https://doi.org/10.1016/j.jstrokecerebrovasdis.2013.01.006
Azab B, Bhatt VR, Phookan J, Murukutla S, Kohn N, Terjanian T, Widmann WD (2012) Usefulness of the neutrophil-to-lymphocyte ratio in predicting short- and long-term mortality in breast cancer patients. Ann Surg Oncol 19:217–224. https://doi.org/10.1245/s10434-011-1814-0
Uthamalingam S, Patvardhan EA, Subramanian S, Ahmed W, Martin W, Daley M, Capodilupo R (2011) Utility of the neutrophil to lymphocyte ratio in predicting long-term outcomes in acute decompensated heart failure. Am J Cardiol 107:433–438. https://doi.org/10.1016/j.amjcard.2010.09.039
Ying HQ, Deng QW, He BS, Pan YQ, Wang F, Sun HL, Chen J, Liu X, Wang SK (2014) The prognostic value of preoperative NLR, d-NLR, PLR and LMR for predicting clinical outcome in surgical colorectal cancer patients. Med Oncol 31:1–8. https://doi.org/10.1007/s12032-014-0305-0
Code availability
Not applicable
Funding
Not applicable
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data analysis were performed by Artur Nobrega Lima Rodrigues de Morais. Data collection was performed by Artur Nobrega Lima Rodrigues de Morais and Victor Matheus Ribeiro Baylão. The first draft of the manuscript was written by Artur Nobrega Lima Rodrigues de Morais, Adilson JM. de Oliveira, and Victor Matheus Ribeiro Baylão. Artur Nobrega Lima Rodrigues de Morais, Victor Matheus Ribeiro Baylão, Alexandra Gomes dos Santos, Mayara Azevedo, Tamires Martins, and Adilson JM. de Oliveira critically revised the work. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Conflicts of interest
The authors read and approved the final manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nóbrega Lima Rodrigues de Morais, A., Ribeiro Baylão, V.M., Martins Silva, T. et al. Is neutrophil-lymphocyte ratio a useful tool for predicting outcome in subarachnoid hemorrhage? A systematic review. Neurosurg Rev 44, 3023–3028 (2021). https://doi.org/10.1007/s10143-021-01484-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-021-01484-7