Abstract
Combined scalp and skull deficiency due to malignant scalp tumors or sequelae of intracranial surgery present challenging entities for both neurosurgeons and reconstructive treatment. In complex cases, an interdisciplinary approach is needed between neurosurgeons and cranio-maxillofacial surgeons. We present a considerably large series for which we identify typical complications and pitfalls and provide evidence for the importance of an interdisciplinary algorithm for chronic wound healing complications and malignomas of the scalp and skull. We retrospectively reviewed all patients treated by the department of neurosurgery and cranio-maxillofacial surgery at our hospital for complex scalp deficiencies and malignant scalp tumors affecting the skull between 2006 and 2019, and extracted data on demographics, surgical technique, and perioperative complications. Thirty-seven patients were treated. Most cases were operated simultaneously (n: 32) and 6 cases in a staged procedure. Nineteen patients obtained a free flap for scalp reconstruction, 15 were treated with local axial flaps, and 3 patients underwent full thickness skin graft treatment. Complications occurred in 62% of cases, mostly related to cerebrospinal fluid (CSF) circulation disorders. New cerebrospinal fluid (CSF) disturbances occurred in 8 patients undergoing free flaps and shunt dysfunction occurred in 5 patients undergoing local axial flaps. Four patients died shortly after the surgical procedure (perioperative mortality 10.8%). Combined scalp and skull deficiency present a challenging task. An interdisciplinary treatment helps to prevent severe and specialty-specific complications, such as hydrocephalus. We therefore recommend a close neurological observation after reconstructive treatment with focus on symptoms of CSF disturbances.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Large skin defects due to chronic wound healing disorders and scalp deficiency, as well as scalp and skull malignancies such as spinalioma and metastases, present a challenge for health care providers [4, 26]. In some cases, patients need to undergo multiple surgeries, and an interdisciplinary approach is needed to provide a sufficient and esthetically satisfying scalp and skin reconstruction [21, 22].
In cases of large scalp defects, different methods can be applied to overcome scalp deficiency. First, local flaps can be used to cover small scalp defects [28], then, microvascular free flaps [15] such as the latissimus dorsi flap, vastus lateralis flap [11], or (para-) scapular flap, are used for reconstruction. In cases of the mentioned microvascular free flaps, donor sites are closed by primary wound closure. Free flaps for scalp reconstruction are considered a safe and successful procedure in complex and challenging cases of scalp and calvarial defects [12]. In terms of skull defects, such as in patients with chronic wound healing disorders and infected or osteolytic calvarial bone, a cranioplasty with alloplastic material is planned to restore cosmesis [1, 13, 25].
The literature focusing on scalp reconstruction is mainly determined by cases and techniques reported by craniofacial surgeons, despite the patient population being neurosurgical cases with initial diagnoses treated in neurosurgical departments.
In our study, we aim to analyze cases treated in an interdisciplinary way, including the neurosurgical and cranio-maxillofacial surgery department, to identify potential risk factors in patients with complicated scalp and skull defects.
Material and methods
Patients
All patients treated in an interdisciplinary way between 2006 and 2019 by the neurosurgical and cranio-maxillofacial surgery departments at our clinic were retrospectively screened for procedures performed due to large chronic wound healing disturbances or malignomas with the need for local or free flap reconstruction of the scalp and skull (inclusion criteria: data on operative therapy available, explicit diagnosis stated, follow-up data complete).
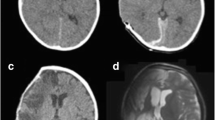
Information on a patient’s demographics, as well as detailed data on the surgical performance and technique, duration of surgery, perioperative complications and management, as well as length of hospital stay were retrieved from our archives and compared depending on the surgical procedures performed in terms of surgical and neurological outcome (Fig. 1).
Ethics
The present study is in accordance with ethical standards outlined in the Declaration of Helsinki; the ethics approval was obtained on the 28th of May 2018 and is listed under document number 218/18 S.
Statistics
Statistical analyses were performed using the Excel spreadsheet statistics software with data analysis package (Microsoft) and SPSS (IBM Corporation Version 26). The statistical hypothesis test was run by a two-sided t test following the Student’s t distribution for paired samples. A p value < 0.05 was considered significant. We performed bivariate and multivariate analysis to analyze possible influencing factors. Multivariate variance analysis was performed with ANOVA.
Results
Patients
In total, 37 patients matched our previously defined inclusion criteria. Fifty-one percent of the patients were female (19/37) and 49% were male (18/37). Median age at time of surgery was 56 years (range 26–86 years). Eighty-four percent of the patients were treated in an interdisciplinary way in a simultaneous operative procedure (neurosurgical intervention and reconstructive surgery, 31 cases), and in 16% of the cases (6/37), a staged procedure was preferred with a delay of 1 to 45 days (mean 17 days).
In total, 11 patients (29.7%) underwent a surgical treatment for hydrocephalus or cerebrospinal fluid (CSF) circulation disorder (ventriculo-peritoneal VP shunt) prior to the scalp and skull reconstruction.
Medical history
The main initial diagnoses leading to the first operative neurosurgical treatment were recurrent high-grade astrocytoma and traumatic brain injury, followed by recurrent meningioma. The numbers are given in Table 1. In 3 cases, skin tumors of the scalp and the skull were surgically removed (1 basalioma, 2 spinalioma) (Table 1).
On average, patients with chronic wound healing disorders underwent a median of 4 surgeries (range 2 to 12) before the interdisciplinary scalp reconstruction was performed; patients with recurrent or primary tumor lesions underwent a median of 3 surgeries (range 0 to 5). The average duration between the initial cranial operative treatment and the need for interdisciplinary wound treatment was 224 days (range 0 to 41.6 years).
General procedure
Thirty-seven patients were treated in total. In 31 patients, the surgical therapy was performed in an interdisciplinary way simultaneously with both neurosurgical and craniofacial expertise in one operative step. In 6 patients, the surgical procedure was staged, with a neurosurgical intervention performed prior to the flap transfer and wound closure (with a time interval of 31 days prior to 45 days after reconstructive therapy).
Neurosurgical procedure
Neurosurgical performances included the treatment of former cranioplasties, either the implantation with computer-aided design (CAD) titanium implants (5/37) or autologous bone graft (2/37) or the removal of the affected cranioplasty (7/37), indicating the need for reconstructive treatment of the osseous compartment and/or dura. In 5 patients, a previously implanted shunt was replaced/transferred to another location (5/37). Ten patients underwent tumor resection and 2 patients were operated for a hematoma. Four patients had their autologous bone graft reduced and 2 patients underwent wound debridement with subdural inspection.
Mean duration of the interdisciplinary surgery was 232 min (range 25 to 672 min).
Scalp reconstruction
Different approaches were applied to patients presenting with scalp deficiencies. Only complex composite defects were included; local wound revisions were excluded due to their missing complexity and interdisciplinary treatment. Local transposition flaps were applied in 15 out of 37 cases and free flaps in 19 complex scalp defects, including the transfer of a latissimus dorsi muscle flap, scapular and parascapular muscle flaps, radial forearm, and the anterolateral thigh (ALT) flap. In one patient, a tissue expander was implanted prior to the reconstruction (Table 2).
In total, in 29 patients (74%) postoperative intravenous antibiotics were administered.
Outcome and complications
Complications occurred in 62% of the cases (22/37). Minor complications included CSF leaks (n: 1) or urinary tract infections with the need of intravenous antibiotic treatment (13/37) (Table 3).
Wound healing problems continued to occur in 5 patients (12.8%) with a need for further operative treatment (in 3 cases a new flap was transferred, 2 cases were treated with local wound adaptations).
In 40.5% of the cases (15/37), patients suffered from a postoperative CSF circulation disorder and 4 underwent surgery for VP shunting after scalp reconstruction after a median of 6 days (range 1 to 607 days). The type of CSF complication was related to the type of flap reconstruction used. Out of 8 patients with preoperative history of a VP-Shunt undergoing local axial flap reconstruction, 5 patients suffered from shunt dysfunctions or shunt infections after the local axial flap reconstruction (62.5% of the shunt patients and 33% of all patients treated with axial local flaps). In the patient group undergoing free flap transfer, 8 patients developed new CSF disturbances which were not present before the operative treatment (42.1%); patients were treated for hydrocephalus via VP Shunt (n: 3), Omaya reservoir (n: 1), external ventricular drain (EVD, n: 3), or lumbar drain (n: 1). Ten patients suffered from ventriculitis (27%). The 3 patients obtaining the EVD were planned for VP Shunt, but died before their operative treatment of the hydrocephalus. Correlation between the occurrence of CSF infection and CSF disturbance with the need for VP Shunt placement or revision did not reach statistical significance (r: 0.278, p = 0.096). Sex and age did not influence the onset of CSF disturbances (p = 0.527 and p = 237). The presence of a previously implanted VP shunt significantly increased the risk for a CSF infection (r: 0.536, p = 0.001) but not CSF disturbances (r: 0.102, p = 0.540).
Four patients died shortly after the scalp reconstruction due to postoperative intracranial hemorrhage, acute hydrocephalus, pulmonary artery embolism, or persistent ventriculitis (Table 3).
Mean length of hospital stay was 37 days (range 3 to 120 days).
Discussion
General aspects
Complex cranial composite defects present challenging complications for routine neurosurgical procedures. In cases of scalp and skull deficiency, different approaches can be used to perform a scalp reconstruction. In our department, patients are treated by an interdisciplinary team to provide a favorable neurological outcome from the neurosurgical point of view and wound closure and reconstruction from the aspect of reconstructive surgery. As previously described in the results section, postoperative complications did not only include wound-healing difficulties but also neurological complications such as hydrocephalus with the need of VP shunting. Depending on the complexity of the scalp and scull defect, different approaches with varying extent of surgery duration and size are used to achieve skin coverage, and to assure its integrity during adjuvant treatment [9]. We presented a large case series with complex composite defects and focus not only on the reconstructive aspect of the treatment, as most publications do [3, 8, 20, 23], but point out neurosurgical complications influencing the overall outcome. We therefore aim to emphasize the importance of the interdisciplinary setting and draw specific attention to the necessity of neurological monitoring after reconstructive surgery (Table 4).
Study limitations
Complications
Due to the complexity of simultaneous surgical treatment, the complication rate is high compared to standard flap reconstruction in non-neurosurgical patients. Complication rates usually rise to 15% [19], but do not focus on neurosurgical patients with skull defects and include patients with local skin tumors without intracranial involvement. Scalp deficiencies occurring postoperatively in neurosurgical patients reported higher complication rates than patients treated for local scalp deficiencies [18]. Scalp deficiencies occurring postoperatively in neurosurgical patients present a unique entity. Difficulties, such as infections due to plates and screws after cranioplasty [14], CSF circulation, wound infections due to dead space [16], and radiation therapy before or after the reconstructive surgery [1, 24] have been described.
The published literature mostly includes small case series with few patients treated via a distinct reconstructive approach [6, 7]. The outcome reported in current literature aims to describe satisfying microvascular free flap reconstructive success rates, but neurological complications are rarely described. Large case series focusing on the interdisciplinary approach and neurosurgical complications are underrepresented in the current literature.
The risk of treatment failure, focusing on neurosurgical complications such as CSF disturbances with influence on microvascular free flap acceptance has been reported previously in one case report in 2017 [10]. Here, the negative pressure gradients cause substantial flap sinking or melting. Flap failure was indeed observed in our cohort in 5 cases, but not directly related to CSF disturbances. To our knowledge, complications related to CSF circulation disorders have otherwise not been reported yet.
In total, 8 patients developed a hydrocephalus after scalp and skull reconstruction with free flap transfer, while patients with local axial flaps had complications with preexisting shunts such as clotting or sudden changes in pressure gradients but did not develop a new hydrocephalus. Patients undergoing reconstructive surgery for complex composite defects are indeed at an increased risk of deep postoperative infection and CSF leaks [21], but the new onset of CSF disturbances with the need of surgical treatment and VP-shunting have not been described so far. Long-term outcomes and neurosurgical pathologies are often underreported in studies on reconstructive techniques, and recurrent CSF leaks may be correlated to undetected hydrocephalus, but we lack detailed information in current literature.
Unfortunately, long-term results including the neurological outcome and ventricle width are often understated in publications, and studies report only on flap loss or wound revisions [27]. After an extensive search, we did not find any literature on CSF disturbances and reconstructive techniques in skull and scalp deficiencies, or information on the placement and need of external ventricular drains. Also, information on the occurrence of ventriculitis with antibiotic administration is not mentioned in manuscripts focusing on the success of scalp and skull reconstruction.
Unfortunately, we did not identify the underlying cause of a new hydrocephalus onset in patients undergoing skull reconstruction. Several authors discussed possible etiologies leading to CSF resorption problems. A suggested cause could be an impairment of the glymphatic system, ventricular squeezing, or reduced arterial pulsations due to arachnoiditis or arteriopathy [2, 5, 17]. Unfortunately, we did not perform specific MRI imaging or metabolic analysis to test for the described hypothesis.
Limitations
Our study was conducted retrospectively; therefore, the causality of complications and their underlying causes can be described, but not proven. We observed many CSF disturbances after reconstructive free flap transfers, pre-existing symptoms of hydrocephalus were not described in the medical data, and preoperative imaging did reveal any signs of CSF disturbances. We presume patients did not suffer from hydrocephalic symptoms, but can retrospectively not exclude it. Chronic wound healing disorders may be caused by pre-existing occult CSF disturbances unapparent on preoperative imaging. The causality between CSF disturbance and reconstructive free flap transfer and which is preceding the other may be different than suspected. As cause and effect cannot be defined retrospectively, we hereby only aim to point out the existence of CSF disturbances after reconstructive surgery, with focus on neurological observation after surgery.
Patients underwent different types of reconstructive surgery, depending on size and complexity of the composite defect. All patients were treated in an interdisciplinary way, with preoperative consultation of both disciplines. In our department, patients remain under the observation of neurosurgeons on a neurosurgical ward focusing on neurosurgical symptoms. Therefore, the detection rate and suspicion of CSF disturbances may be higher than in departments with patients treated for reconstructive surgery without neurosurgical participation. As patients are treated interdisciplinary, the surgical reconstructive treatment and neurosurgical complications can be observed during the same hospital stay. In hospitals with strictly separated departments, the detection of neurological symptoms may be delayed or even missed.
Conclusion
Neurosurgical complications such as CSF leaks or circulation disorders are common in patients undergoing cranial reconstructive therapy. Especially in patients undergoing free flap reconstruction, CSF disturbances occurred in many cases and must be considered and controlled postoperatively. In order to prevent postoperative complications to assure the optimal neurosurgical and reconstructive outcome, an interdisciplinary treatment needs to be provided for patients with large composite scalp and skull defects.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Afifi A, Djohan RS, Hammert W, Papay FA, Barnett AE, Zins JE (2010) Lessons learned reconstructing complex scalp defects using free flaps and a cranioplasty in one stage. J Craniofac Surg 21:1205–1209. https://doi.org/10.1097/SCS.0b013e3181e17c1e
Akins PT, Guppy KH (2019) Are Hygromas and hydrocephalus after decompressive craniectomy caused by impaired brain Pulsatility, cerebrospinal fluid hydrodynamics, and glymphatic drainage? Literature overview and illustrative cases. World Neurosurg 130:e941–e952. https://doi.org/10.1016/j.wneu.2019.07.041
Desai SC, Sand JP, Sharon JD, Branham G, Nussenbaum B (2015) Scalp reconstruction: an algorithmic approach and systematic review. JAMA facial plastic surgery 17:56–66. https://doi.org/10.1001/jamafacial.2014.889
Di Rienzo A, Pangrazi PP, Riccio M, Colasanti R, Ghetti I, Iacoangeli M (2016) Skin flap complications after decompressive craniectomy and cranioplasty: proposal of classification and treatment options. Surg Neurol Int 7:S737–S745. https://doi.org/10.4103/2152-7806.193724
Greitz D, Greitz T, Hindmarsh T (1997) A new view on the CSF-circulation with the potential for pharmacological treatment of childhood hydrocephalus. Acta Paediatr 86:125–132. https://doi.org/10.1111/j.1651-2227.1997.tb08850.x
Han DH, Park MC, Park DH, Song H, Lee IJ (2013) Role of muscle free flap in the salvage of complicated scalp wounds and infected prosthetic dura. Arch Plast Surg 40:735–741. https://doi.org/10.5999/aps.2013.40.6.735
Heron A, Michot A, Menez T, Jecko V, Penchet G, Casoli V (2019) Secondary reconstruction of calvarial defects by using free flap: report of consecutive cases and analysis of strategy. J Craniofac Surg 30:e151–e155. https://doi.org/10.1097/SCS.0000000000005099
Hierner R, van Loon J, Goffin J, van Calenbergh F (2007) Free latissimus dorsi flap transfer for subtotal scalp and cranium defect reconstruction: report of 7 cases. Microsurgery 27:425–428. https://doi.org/10.1002/micr.20386
Hussussian CJ, Reece GP (2002) Microsurgical scalp reconstruction in the patient with cancer. Plast Reconstr Surg 109:1828–1834. https://doi.org/10.1097/00006534-200205000-00008
Joo JD, Jang JU, Kim H, Yoon ES, Kang DH (2017) Cranial defect overlying a Ventriculoperitoneal shunt: pressure gradient leading to free flap deterioration? Arch Craniofac Surg 18:186–190. https://doi.org/10.7181/acfs.2017.18.3.186
Kwee MM, Rozen WM, Ting JW, Mirkazemi M, Leong J, Baillieu C (2012) Total scalp reconstruction with bilateral anterolateral thigh flaps. Microsurgery 32:393–396. https://doi.org/10.1002/micr.21954
Lessard L, Tahiri Y (2013) Complex scalp, skull, and dural defect reconstruction using a turnover "tournedos" myocutaneous free flap. J Craniofac Surg 24:62–65. https://doi.org/10.1097/SCS.0b013e318272db28
Murdoch A (1976) Titanium cranioplasty in the repair of skull defects. Nurs Times 72:1426–1429
Nagasao T, Horiguchi T, Miyamoto J, Kishi K (2011) Reconstruction of the scalp with a calvarial defect. Surg Today 41:189–196. https://doi.org/10.1007/s00595-009-4262-8
Oh SJ, Lee J, Cha J, Jeon MK, Koh SH, Chung CH (2011) Free-flap reconstruction of the scalp: donor selection and outcome. J Craniofac Surg 22:974–977. https://doi.org/10.1097/SCS.0b013e31820fe354
Ozaki M, Narita K, Kurita M, Iwashina Y, Takushima A, Harii K (2017) Implantation of thickened artificial bone for reduction of dead space and prevention of infection between implant and dura in secondary reconstruction of the skull. J Craniofac Surg 28:888–891. https://doi.org/10.1097/SCS.0000000000003507
Rasmussen MK, Mestre H, Nedergaard M (2018) The glymphatic pathway in neurological disorders. Lancet Neurol 17:1016–1024. https://doi.org/10.1016/S1474-4422(18)30318-1
Shimada K, Ishikura N, Heshiki T, Kawakami S (2007) Treatment for chronic abscess after cranioplasty: reconstruction of dura maters using the anterolateral thigh flap with fascia lata. J Craniofac Surg 18:1305–1308. https://doi.org/10.1097/scs.0b013e31811ec238
Shonka DC, Potash AE, Jameson MJ, Funk GF (2011) Successful reconstruction of scalp and skull defects: lessons learned from a large series. Laryngoscope 121:2305–2312. https://doi.org/10.1002/lary.22191
Simunovic F, Eisenhardt SU, Penna V, Thiele JR, Stark GB, Bannasch H (2016) Microsurgical reconstruction of oncological scalp defects in the elderly. Journal of plastic, reconstructive & aesthetic surgery : JPRAS 69:912–919. https://doi.org/10.1016/j.bjps.2016.03.021
Steiner D, Horch RE, Eyüpoglu I, Buchfelder M, Arkudas A, Schmitz M, Ludolph I, Beier JP, Boos AM (2018) Reconstruction of composite defects of the scalp and neurocranium-a treatment algorithm from local flaps to combined AV loop free flap reconstruction. World J Surg Oncol 16:217. https://doi.org/10.1186/s12957-018-1517-0
Steiner D, Hubertus A, Arkudas A, Taeger CD, Ludolph I, Boos AM, Schmitz M, Horch RE, Beier JP (2017) Scalp reconstruction: a 10-year retrospective study. J Craniomaxillofac Surg 45:319–324. https://doi.org/10.1016/j.jcms.2016.11.023
Uzun H, Bitik O, Ersoy US, Bilginer B, Aksu AE (2018) Comparison of musculocutaneous and fasciocutaneous free flaps for the reconstruction of the extensive composite scalp and cranium defects. The Journal of craniofacial surgery 29:1947–1951. https://doi.org/10.1097/SCS.0000000000005052
Wang HT, Erdmann D, Olbrich KC, Friedman AH, Levin LS, Zenn MR (2007) Free flap reconstruction of the scalp and calvaria of major neurosurgical resections in cancer patients: lessons learned closing large, difficult wounds of the dura and skull. Plast Reconstr Surg 119:865–872. https://doi.org/10.1097/01.prs.0000240830.19716.c2
Winkler PA, Stummer W, Linke R, Krishnan KG, Tatsch K (2000) Influence of cranioplasty on postural blood flow regulation, cerebrovascular reserve capacity, and cerebral glucose metabolism. J Neurosurg 93:53–61. https://doi.org/10.3171/jns.2000.93.1.0053
Wolff AY, Santiago GF, Belzberg M, Manson PN, Huang J, Brem H, Gordon CR (2019) Full-thickness skin grafting for local defect coverage following scalp adjacent tissue transfer in the setting of cranioplasty. J Craniofac Surg 30:115–119. https://doi.org/10.1097/SCS.0000000000004872
Yoshioka N (2017) Versatility of the Latissimus Dorsi free flap during the treatment of complex postcraniotomy surgical site infections. Plast Reconstr Surg Glob Open 5:e1355. https://doi.org/10.1097/GOX.0000000000001355
Zayakova Y, Stanev A, Mihailov H, Pashaliev N (2013) Application of local axial flaps to scalp reconstruction. Arch Plast Surg 40:564–569. https://doi.org/10.5999/aps.2013.40.5.564
Funding
Open Access funding provided by Projekt DEAL. This work was financed by the Department of Neurosurgery at the Klinikum rechts der Isar (Technical University Munich).
Author information
Authors and Affiliations
Contributions
V. Butenschoen (VB) and S. Krieg (SK) made substantial contributions to study conception and design, acquisition of data, analysis and interpretation of data; SK and VB have been involved in drafting the manuscript and revising it critically for important intellectual content; JW, LR, SK, and BM gave final approval of the version to be published. VB and SK agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Consent for publication
Informed consent for publication was obtained.
Ethics
The present study is in accordance with ethical standards outlined in the Declaration of Helsinki; the ethics approval was obtained on the 28th of May 2018 and is listed under document number 218/18 S.
Competing interests
SK is a consultant for Spineart Deutschland GmbH (Frankfurt, Germany) and Nexstim Plc (Helsinki, Finland) and received honoraria from Medtronic (Meerbusch, Germany) and Carl Zeiss Meditec (Oberkochen, Germany). SK and BM received research grants from and are consultants for Brainlab AG (Munich, Germany). BM received honoraria, consulting fees, and research grants from Medtronic (Meerbusch, Germany), icotec ag (Altstätten, Switzerland), and Relievant Medsystemy Inc. (Sunnyvale, CA, USA); honoraria and research grants from Ulrich Medical (Ulm, Germany); honoraria and consulting fees from Spineart Deutschland GmbH (Frankfurt, Germany) and DePuy Synthes (West Chester, PA, USA); and royalties from Spineart Deutschland GmbH (Frankfurt, Germany). All authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this publication.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Butenschoen, V.M., Weitz, J., Ritschl, L.M. et al. CSF disturbances and other neurosurgical complications after interdisciplinary reconstructions of large combined scalp and skull deficiencies. Neurosurg Rev 44, 1583–1589 (2021). https://doi.org/10.1007/s10143-020-01347-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-020-01347-7