Abstract
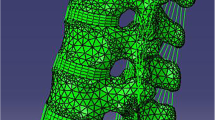
Previous finite element studies of thoracolumbar fractures were mostly based on simulation analysis of one single object, which was difficult to objectively evaluate the differences between conventional pedicle screws and Schanz pedicle screws. The aim of this study was to evaluate the stress of screw and injured vertebrae displacement using the finite element model of conventional pedicle screw and Schanz pedicle screw instrumentation for the treatment of lumbar 1 fractures. Data of eight healthy volunteers were used to simulate the finite element model. The instrumentation models were divided into four groups: moderate fracture conventional (MC), moderate fracture Schanz (MS), unstable/severe fracture conventional (UC), and unstable/severe fracture Schanz (US) pedicle screw groups. The maximum screw stress and lumbar 1 displacement/micro-motion in each group increased with the increase of torque and/or load. Under the same fracture, maximum von Mises stress of conventional pedicle screw (MC/UC) was larger than Schanz pedicle screw (MS/US) (P < 0.05) and lumbar 1 displacement/micro-motion of Schanz pedicle screw (MS/US) was larger than conventional pedicle screw (MC/UC) (P < 0.05). Under the same screws, the maximum von Mises stress and displacement/micro-motion of unstable fracture (UC/US) were larger than moderate fracture (MC/MS) (P < 0.05). Posterior short-segment instrumentation with Schanz pedicle screws were recommended for unstable fractures. The compression displacement/micro-motion of bony defect during flexion may lead to the postoperative re-collapse of injured vertebrae.








Similar content being viewed by others
References
Aono H, Tobimatsu H, Ariga K, Kuroda M, Nagamoto Y, Takenaka S, Furuya M, Iwasaki M (2016) Surgical outcomes of temporary short-segment instrumentation without augmentation for thoracolumbar burst fractures. Injury 47:1337–1344. https://doi.org/10.1016/j.injury.2016.03.003
Mi J, Sun XJ, Zhang K, Zhao CQ, Zhao J (2018) Prediction of MRI findings including disc injury and posterior ligamentous complex injury in neurologically intact thoracolumbar burst fractures by the parameters of vertebral body damage on CT scan. Injury 49:272–278. https://doi.org/10.1016/j.injury.2017.12.011
Aono H, Ishii K, Tobimatsu H, Nagamoto Y, Takenaka S, Furuya M, Chiaki H, Iwasaki M (2017) Temporary short-segment pedicle screw fixation for thoracolumbar burst fractures: comparative study with or without vertebroplasty. Spine J: Off J North Am Spine Soc17:1113–1119. doi:https://doi.org/10.1016/j.spinee.2017.03.022
Xu GJ, Li ZJ, Ma JX, Zhang T, Fu X, Ma XL (2013) Anterior versus posterior approach for treatment of thoracolumbar burst fractures: a meta-analysis. Eur Spine J : Off Publ Eur Spine Soc, Eur Spinal Deform Soc Eur Sect Cervical Spine Res Soc 22:2176–2183. https://doi.org/10.1007/s00586-013-2987-y
McCormack T, Karaikovic E, Gaines RW (1994) The load sharing classification of spine fractures. Spine 19:1741–1744
Pneumaticos SG, Triantafyllopoulos GK, Giannoudis PV (2013) Advances made in the treatment of thoracolumbar fractures: current trends and future directions. Injury 44:703–712. https://doi.org/10.1016/j.injury.2012.12.005
Ozdemir B, Kanat A, Erturk C, Batcik OE, Balik MS, Yazar U, Celiker FB, Metin Y, Inecikli MF, Guvercin AR (2017) Restoration of anterior vertebral height by short-segment pedicle screw fixation with screwing of fractured vertebra for the treatment of unstable thoracolumbar fractures. World Neuros 99:409–417. https://doi.org/10.1016/j.wneu.2016.11.133
Kanna RM, Shetty AP, Rajasekaran S (2015) Posterior fixation including the fractured vertebra for severe unstable thoracolumbar fractures. Spine J: Off J N Am Spine Soc 15:256–264. https://doi.org/10.1016/j.spinee.2014.09.004
Pellise F, Barastegui D, Hernandez-Fernandez A, Barrera-Ochoa S, Bago J, Issa-Benitez D, Caceres E, Villanueva C (2015) Viability and long-term survival of short-segment posterior fixation in thoracolumbar burst fractures. Spine J: Off J N Am Spine Soc 15:1796–1803. https://doi.org/10.1016/j.spinee.2014.03.012
Yang S, Shang DP, Lu JM, Liu JF, Fu DP, Zhou F, Cong Y, Lv ZZ (2018) Modified posterior short-segment pedicle screw instrumentation for lumbar burst fractures with incomplete neurological deficit. World Neurosurg 119:e977–e985. https://doi.org/10.1016/j.wneu.2018.08.014
Jang HD, Bang C, Lee JC, Soh JW, Choi SW, Cho HK, Shin BJ (2018) Risk factor analysis for predicting vertebral body re-collapse after posterior instrumented fusion in thoracolumbar burst fracture. Spine J : Off J N Am Spine Soc18:285–293. doi:https://doi.org/10.1016/j.spinee.2017.07.168
Liu J, Yang S, Lu J, Fu D, Liu X, Shang D (2018) Biomechanical effects of USS fixation with different screw insertion depths on the vertebrae stiffness and screw stress for the treatment of the L1 fracture. J Back Musculoskel Rehab 31:285–297. https://doi.org/10.3233/bmr-169692
Xu G, Fu X, Du C, Ma J, Li Z, Tian P, Zhang T, Ma X (2014) Biomechanical comparison of mono-segment transpedicular fixation with short-segment fixation for treatment of thoracolumbar fractures: a finite element analysis. Proc Inst Mech Eng H J Eng Med 228:1005–1013. https://doi.org/10.1177/0954411914552308
Kubosch D, Kubosch EJ, Gueorguiev B, Zderic I, Windolf M, Izadpanah K, Sudkamp NP, Strohm PC (2016) Biomechanical investigation of a minimally invasive posterior spine stabilization system in comparison to the Universal Spinal System (USS). BMC Musculoskelet Disord 17:134. https://doi.org/10.1186/s12891-016-0983-1
Liao JC, Chen WP, Wang H (2017) Treatment of thoracolumbar burst fractures by short-segment pedicle screw fixation using a combination of two additional pedicle screws and vertebroplasty at the level of the fracture: a finite element analysis. BMC Musculoskelet Disord 18:262. https://doi.org/10.1186/s12891-017-1623-0
Alizadeh M, Kadir MR, Fadhli MM, Fallahiarezoodar A, Azmi B, Murali MR, Kamarul T (2013) The use of X-shaped cross-link in posterior spinal constructs improves stability in thoracolumbar burst fracture: a finite element analysis. J Orthop Res : Off Publ Orthop Res Soc 31:1447–1454. https://doi.org/10.1002/jor.22376
Chen SH, Chiang MC, Lin JF, Lin SC, Hung CH (2013) Biomechanical comparison of three stand-alone lumbar cages--a three-dimensional finite element analysis. BMC Musculoskelet Disord 14:281. https://doi.org/10.1186/1471-2474-14-281
Li C, Zhou Y, Wang H, Liu J, Xiang L (2014) Treatment of unstable thoracolumbar fractures through short segment pedicle screw fixation techniques using pedicle fixation at the level of the fracture: a finite element analysis. PLoS One 9:e99156. https://doi.org/10.1371/journal.pone.0099156
Naserkhaki S, El-Rich M (2017) Sensitivity of lumbar spine response to follower load and flexion moment: finite element study. Computer methods in biomechanics and biomedical engineering 20:550–557. https://doi.org/10.1080/10255842.2016.1257707
Rohlmann A, Neller S, Claes L, Bergmann G, Wilke HJ (2001) Influence of a follower load on intradiscal pressure and intersegmental rotation of the lumbar spine. Spine 26:E557–E561
Vaccaro AR, Oner C, Kepler CK, Dvorak M, Schnake K, Bellabarba C, Reinhold M, Aarabi B, Kandziora F, Chapman J, Shanmuganathan R, Fehlings M, Vialle L (2013) AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine 38:2028–2037. https://doi.org/10.1097/BRS.0b013e3182a8a381
Wang H, Zhao Y, Mo Z, Han J, Chen Y, Yu H, Wang Q, Liu J, Li C, Zhou Y, Xiang L (2017) Comparison of short-segment monoaxial and polyaxial pedicle screw fixation combined with intermediate screws in traumatic thoracolumbar fractures: a finite element study and clinical radiographic review. Clinics (Sao Paulo, Brazil) 72:609–617. https://doi.org/10.6061/clinics/2017(10)04
Panjabi MM, Oxland TR, Lin RM, McGowen TW (1994) Thoracolumbar burst fracture. A biomechanical investigation of its multidirectional flexibility. Spine 19:578–585
Yamamoto I, Panjabi MM, Crisco T, Oxland T (1989) Three-dimensional movements of the whole lumbar spine and lumbosacral joint. Spine 14:1256–1260
Brown SA (2006) Chapter 2–synthetic biomaterials for spinal applications. Spine Technology Handbook:11–33
Bu BX, Wang MJ, Liu WF, Wang YS, Tan HL (2015) Short-segment posterior instrumentation combined with calcium sulfate cement vertebroplasty for thoracolumbar compression fractures: radiographic outcomes including nonunion and other complications. Orthopaedics & traumatology, surgery & research : OTSR 101:227–233. https://doi.org/10.1016/j.otsr.2014.11.019
Elmasry SS, Asfour SS, Travascio F (2018) Finite element study to evaluate the biomechanical performance of the spine after augmenting percutaneous pedicle screw fixation with kyphoplasty in the treatment of burst fractures. J Biomech Eng 140:061005. https://doi.org/10.1115/1.4039174
Wilke HJ, Rohlmann A, Neller S, Graichen F, Claes L, Bergmann G (2003) ISSLS prize winner: a novel approach to determine trunk muscle forces during flexion and extension: a comparison of data from an in vitro experiment and in vivo measurements. Spine 28:2585–2593. https://doi.org/10.1097/01.brs.0000096673.16363.c7
Lakshmanan P, Jones A, Mehta J, Ahuja S, Davies PR, Howes JP (2009) Recurrence of kyphosis and its functional implications after surgical stabilization of dorsolumbar unstable burst fractures. Spine J : Off J N Am Spine Soc 9:1003–1009. doi:https://doi.org/10.1016/j.spinee.2009.08.457
Funding
This work was supported by the National Natural Science Foundation of China (grant 30870647) and Dalian Medical Scientific Research Project (grant 1811110).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
This study was approved by the Ethics Committee of Affiliated Zhongshan Hospital of Dalian University.
Informed consent
All participants provided written informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhou, F., Yang, S., Liu, J. et al. Finite element analysis comparing short-segment instrumentation with conventional pedicle screws and the Schanz pedicle screw in lumbar 1 fractures. Neurosurg Rev 43, 301–312 (2020). https://doi.org/10.1007/s10143-019-01146-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-019-01146-9