Abstract
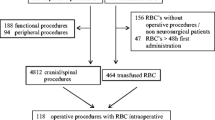
We assessed the impact of intra- and postoperative RBC transfusion on postoperative morbidity and mortality in cranial surgery. A total of 8924 adult patients who underwent cranial surgery were identified in the 2006–2011 American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) database. Patients undergoing a biopsy, radiosurgery, or outpatient surgery were excluded. Propensity scores were calculated according to demographic variables, comorbidities, and preoperative laboratory values. Patients who had received RBC transfusion were matched to those who did not, by propensity score, preoperative hematocrit level, and by length of surgery, as an indirect measure of potential intraoperative blood loss. Logistic regression was used to predict adverse postoperative outcomes. A total of 625 (7%) patients were transfused with one or more units of packed RBCs. Upon matching, preoperative hematocrit, length of surgery, and emergency status were no longer different between transfused and non-transfused patients. RBC transfusion was associated with prolonged length of hospitalization (OR 1.6, 95% CI 1.2–2.2), postoperative complications (OR 2.8, 95% CI 2.0–3.8), 30-day return to operation room (OR 2.0, 95% CI 1.3–3.2), and 30-day mortality (OR 4.3, 95% CI 2.4–7.6). RBC transfusion is associated with substantive postoperative morbidity and mortality in patients undergoing both elective and emergency cranial surgery. These results suggest judicious use of transfusion in cranial surgery, consideration of alternative means of blood conservation, or pre-operative restorative strategies in patients undergoing elective surgery, when possible.

Similar content being viewed by others
References
American College of Surgeons National Surgical Quality Improvement Project (2012) User guide for the 2011 participant use data file. American College of Surgeons, Chicago
Andrews NB (2009) Neurosurgical procedures in Jehovah’s witnesses: the Tema experience. West Afr J Med 28(3):148–150
Bergstralh E, Kosanke J (1995) Computerized matching of cases to controls. Technical report serial no. 56. Mayo Clinic Section of Biostatistics, Minnesota
Beris P, Muñoz M, García-Erce JA, Thomas D, Maniatis A, Van der Linden P (2008) Perioperative anaemia management: consensus statement on the role of intravenous iron. Br J Anaesth 100(5):599–604
Carlson AP, Schermer CR, Lu SW (2006) Retrospective evaluation of anemia and transfusion in traumatic brain injury. J Trauma 61(3):567–571
Carson JL, Terrin ML, Noveck H, Sanders DW, Chaitman BR, Rhoads GG et al (2011) FOCUS investigators. Liberal or restrictive transfusion in high-risk patients after hip surgery. N Engl J Med 365(26):2453–2462
Dhar R, Zazulia AR, Videen TO, Zipfel GJ, Derdeyn CP, Diringer MN (2009) Red blood cell transfusion increases cerebral oxygen delivery in anemic patients with subarachnoid hemorrhage. Stroke 40(9):3039–3044
Engoren MC, Habib RH, Zacharias A, Schwann TA, Riordan CJ, Durham SJ (2002) Effect of blood transfusion on long-term survival after cardiac operation. Ann Thorac Surg 74(4):1180–1186
Feagan BG, Wong CJ, Kirkley A, Johnston DW, Smith FC, Whitsitt P et al (2000) Erythropoietin with iron supplementation to prevent allogeneic blood transfusion in total hip joint arthroplasty. A randomized, controlled trial. Ann Intern Med 133(11):845–854
George ME, Skarda DE, Watts CR, Pham HD, Beilman GJ (2008) Aggressive red blood cell transfusion: no association with improved outcomes for victims of isolated traumatic brain injury. Neurocrit Care 8(3):337–343
Glance LG, Dick AW, Mukamel DB, Fleming FJ, Zollo RA, Wissler R et al (2011) Association between intraoperative blood transfusion and mortality and morbidity in patients undergoing noncardiac surgery. Anesthesiology 114(2):283–292
Hébert PC, Wells G, Blajchman MA, Marshall J, Martin C, Pagliarello G et al (1999) A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. Transfusion requirements in critical care investigators, Canadian critical care trials group. N Engl J Med 340(6):409–417
Heddle NM, Cook RJ, Arnodl DM, Lui Y, Barty R, Crowther MA et al (2016) Effect of short-term vs. long-term blood storage on mortality after transfusion. N Engl J Med 375(20):1937–1945
Hendrickson JE, Hillyer CD (2009) Noninfectious serious hazards of transfusion. Anesth Analg 108(3):759–769
Hu SS (2004) Blood loss in adult spinal surgery. Eur Spine J 13(Suppl 1):S3–S5
Koch CG, Khandwala F, Li L, Estafanous FG, Loop FD, Blackstone EH (2006) Persistent effect of red cell transfusion on health-related quality of life after cardiac surgery. Ann Thorac Surg 82(1):13–20
Koch CG, Li L, Duncan AI, Mihaljevic T, Cosgrove DM, Loop FD et al (2006) Morbidity and mortality risk associated with red blood cell and blood-component transfusion in isolated coronary artery bypass grafting. Crit Care Med 34(6):1608–1616
Koch CG, Li L, Sessler DI, Figueroa P, Hoeltge GA, Mihaljevic T, Blackstone EH (2008) Duration of red-cell storage and complications after cardiac surgery. N Engl J Med 358(12):1229–1239
Khuri SF, Henderson WG, Daley J, Jonasson O, Jones RS, Campbell DA et al (2007) The patient safety in surgery study: background, study design, and patient populations. J Am Coll Surg 204:1089–1102
Kramer AH, Le Roux P (2012) Red blood cell transfusion and transfusion alternatives in traumatic brain injury. Curr Treat Options Neurol. doi:10.1007/s11940-012-0167-8
Kumar A (2009) Perioperative management of anemia: limits of blood transfusion and alternatives to it. Cleve Clin J Med 76(Suppl 4):S112–S118
Kumar MA, Boland TA, Baiou M, Moussouttas M, Herman JH, Bell RD et al (2013) Red blood cell transfusion increases the risk of thrombotic events in patients with subarachnoid hemorrhage. Neurocrit Care 20(1):84–90
Naidech AM, Shaibani A, Garg RK, Duran IM, Liebling SM, Bassin SL et al (2010) Prospective, randomized trial of higher goal hemoglobin after subarachnoid hemorrhage. Neurocrit Care 13(3):313–320
Okuyama M, Ikeda K, Shibata T, Tsukahara Y, Kitada M, Shimano T (2005) Preoperative iron supplementation and intraoperative transfusion during colorectal cancer surgery. Surg Today 35(1):36–40
Rosenbaum PR, Rubin D (1983) The central role of the propensity score in observational studies for causal effects. Biometrika 70:41–55
Seicean A, Seicean S, Alan N, Schiltz NK, Rosenbaum BP, Jones PK et al (2013) Pre-operative anemia and peri-operative outcomes in patients who undergo elective spine surgery. Spine 38(15):1331–1341
Shander A, Hofmann A, Ozawa S, Theusinger OM, Gombotz H, Spahn DR (2010) Activity-based costs of blood transfusions in surgical patients at four hospitals. Transfusion 50(4):753–765
Smith MJ, Le Roux PD, Elliott JP, Winn HR (2004) Blood transfusion and increased risk for vasospasm and poor outcome after subarachnoid hemorrhage. J Neurosurg 101(1):1–7
Suess S, Suess O, Brock M (2001) Neurosurgical procedures in Jehovah's witnesses: an increased risk? Neurosurgery 49(2):266–272
Theusinger OM, Leyvraz PF, Schanz U, Seifert B, Spahn DR (2007) Treatment of iron deficiency anemia in orthopedic surgery with intravenous iron: efficacy and limits: a prospective study. Anesthesiology 107(6):923–927
Villanueva C, Colomo A, Bosch A, Concepción M, Hernandez-Gea V, Aracil C et al (2013) Transfusion strategies for acute upper gastrointestinal bleeding. N Engl J Med 368(1):11–21
Warner MA, O'Keeffe T, Bhavsar P, Shringer R, Moore C, Harper C et al (2010) Transfusions and long-term functional outcomes in traumatic brain injury. J Neurosurg 113(3):539–546
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interests
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with animals performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Cohen, J.A., Alan, N., Seicean, A. et al. Risk associated with perioperative red blood cell transfusion in cranial surgery. Neurosurg Rev 40, 633–642 (2017). https://doi.org/10.1007/s10143-017-0819-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-017-0819-y