Abstract
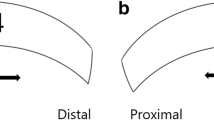
Moyamoya disease (MMD) and atherosclerotic cerebrovascular disease (ACVD) differ in angiographic appearance and probably hemodynamics. Pediatric MMD (PMMD) usually presents with cerebral ischemia, while intracranial hemorrhage is more common in adult MMD (AMMD), suggesting differences in cerebral hemodynamics. We analyzed the cortical flow velocity and direction of recipient arteries using micro-Doppler ultrasonography to evaluate the cortical circulation before and after anastomosis in MMD and ACVD. Twenty-eight patients with adult MMD (AMMD), 7 with pediatric MMD (PMMD), 16 with ACVD, and 12 control patients were studied. A micro-Doppler probe was applied on the cortical recipient artery (A4 or M4) before and after anastomosis. Systolic maximum flow velocity (V max) and blood flow direction were investigated at proximal and distal parts of anastomosed sites in recipient arteries. Pre- and postoperative regional cerebral blood flow was measured by cold xenon-computed tomography (Xe-CT). Before anastomosis, retrograde cortical flow was significantly more common in PMMD patients, and V max in cortical artery was significantly lower in AMMD patients. Bypass surgery changed the direction of blood flow from the anastomosis site to proximal and distal sites of the recipient artery in most patients, but pre-anastomosis flow direction was preserved more frequently in PMMD patients. The rate of V max increase after anastomosis was significantly higher in AMMD than in PMMD (11.6 ± 9.8 vs. 3.9 ± 1.8; P = 0.01). Micro-Doppler ultrasonography identified differences in cortical circulation among AMMD, PMMD, and ACVD. In AMMD, significantly low velocity in the cortical artery was observed before anastomosis, and bypass surgery reversed the flow and significantly increased flow velocity. The data of PMMD showed unique hemodynamics of the cortical artery before anastomosis, characterized by a higher frequency of retrograde flow and preserved velocity. The V max increase rate was significantly higher in patients with postoperative cerebral hyperperfusion on Xe-CT, and further study is warranted to validate the clinical use of intraoperative micro-Doppler monitoring to predict postoperative hyperperfusion.






Similar content being viewed by others

References
Akdemir H, Oktem S, Menkü A, Tucer B, Tuğcu B, Günaldi O (2007) Image-guided microneurosurgical management of small arteriovenous malformation: role of neuronavigation and intraoperative Doppler sonography. Minim Invasive Neurosurg 50:163–169
Awano T, Sakatani K, Yokose N, Kondo Y, Igarashi T, Hoshino T, Nakamura S, Fujiwara N, Murata Y, Katayama Y, Shikayama T, Miwa M (2010) Intraoperative EC-IC bypass blood flow assessment with indocyanine green angiography in moyamoya and non-moyamoya ischemic stroke. World Neurosurg 73:668–674
Bishop CCR, Powell S, Rutt D (1986) Transcranial Doppler measurement of middle cerebral artery blood flow velocity: a validation study. Stroke 17:913–915
Czabanka M, Peña-Tapia P, Schubert GA, Heppner FL, Martus P, Horn P, Schmiedek P, Vajkoczy P (2011) Proposal for a new grading of moyamoya disease in adult patients. Cerebrovasc Dis 32:41–50
Czabanka M, Peña-Tapia P, Schubert GA, Woitzik J, Vajkoczy P, Schmiedek P (2008) Characterization of cortical microvascularization in adult Moyamoya disease. Stroke 39:1703–1709
Fujimura M, Mugikura S, Kaneta T, Shimizu H, Tominaga T (2009) Incidence and risk factors for symptomatic cerebral hyperperfusion after superficial temporal artery–middle cerebral artery anastomosis in patients with moyamoya disease. Surg Neurol 71:442–447
Gesang DZ, Zhang D, Zhao JZ, Wang S, Zhao YL, Wang R, Sun JJ, Meng Z (2009) Laser Doppler flowmeter study on regional cerebral blood flow in early stage after standard superficial temporal artery–middle cerebral artery bypass surgery for moyamoya disease. Chin Med J 122:2412–2418
Houkin K, Yoshimoto T, Kuroda S, Ishikawa T, Takahashi A, Abe H (1996) Angiographic analysis of moyamoya disease—how does moyamoya disease progress? Neurol Med Chir (Tokyo) 36:783–788
Kapsalaki EZ, Lee GP, Robinson JS 3rd, Grigorian AA, Fountas KN (2008) The role of intraoperative micro-Doppler ultrasound in verifying proper clip placement in intracranial aneurysm surgery. J Clin Neurosci 15:153–157
Kawamata T, Kawashima A, Yamaguchi K, Hori T, Okada Y (2011) Usefulness of intraoperative laser Doppler flowmetry and thermography to predict a risk of postoperative hyperperfusion after superficial temporal artery–middle cerebral artery bypass for moyamoya disease. Neurosurg Rev 34:355–362
Kawamata T, Okada Y, Kawashima A, Yoneyama T, Yamaguchi K, Ono Y, Hori T (2009) Postcarotid endarterectomy cerebral hyperperfusion can be prevented by minimizing intraoperative cerebral ischemia and strict postoperative blood pressure control under continuous sedation. Neurosurgery 64:447–454
Kawashima A, Kawamata T, Yamaguchi K, Hori T, Okada Y (2010) Successful superficial temporal artery–anterior cerebral artery direct bypass using a long graft for moyamoya disease: technical note. Neurosurgery 67 (3 Suppl Operative):ons145–149
Kim SK, Seol HJ, Cho BK, Hwang YS, Lee DS, Wang KC (2004) Moyamoya disease among young patients: its aggressive clinical course and the role of active surgical treatment. Neurosurgery 54:840–846
Lee M, Guzman R, Bell-Stephens T, Steinberg GK (2011) Intraoperative blood flow analysis of direct revascularization procedures in patients with moyamoya disease. J Cereb Blood Flow Metab 31:262–274
Lee M, Zaharchuk G, Guzman R, Achrol A, Bell-Stephens T, Steinberg GK (2009) Quantitative hemodynamic studies in moyamoya disease: a review. Neurosurg Focus 26:E5
Mücke T, Wolff KD, Wagenpfeil S, Hölzle F, Scholz M (2010) Reliability of near-infrared angiography and micro-Doppler sonography for evaluating microvascular anastomoses. Plast Reconstr Surg 126:1506–1514
Nakagawa A, Fujimura M, Arafune T, Suzuki H, Sakuma I, Tominaga T (2008) Intraoperative infrared brain surface blood flow monitoring during superficial temporal artery–middle cerebral artery anastomosis in a patient with moyamoya disease: clinical implication of the gradation value in postoperative clinical course—a case report. Acta Neurochir Suppl 102:159–163
Nishimoto A, Takeuchi S (1968) Abnormal cerebral vascular network related to the internal carotid arteries. J Neurosurg 29:255–260
Obara K, Fukuuchi Y, Kobari M, Watanabe S, Dembo T (1997) Cerebral hemodynamics in patients with moyamoya disease and in patients with atherosclerotic occlusion of the major cerebral arterial trunks. Clin Neurol Neurosurg 99(Suppl 2):S86–S89
Ogasawara K, Ogawa A (2006) JET study (Japanese EC-IC Bypass Trial). Nippon Rinsho 64(Suppl 7):524–527
Okada Y, Kawamata T, Kawashima A, Hori T (2007) Intraoperative application of thermography in extracranial-intracranial bypass surgery. Neurosurgery 60(4 Suppl 2):362–365
Okada Y, Kawamata T, Kawashima A, Yamaguchi K, Ono Y, Hori T (2012) The efficacy of superficial temporal artery–middle cerebral artery anastomosis in patients with moyamoya disease complaining of severe headache. J Neurosurg 116:672–679
Okada Y, Shima T, Nishida M, Yamane K, Yamada T, Yamanaka C (1998) Effectiveness of superficial temporal artery–middle cerebral artery anastomosis in adult moyamoya disease: cerebral hemodynamics and clinical course in ischemic and hemorrhagic varieties. Stroke 29:625–630
Okada Y, Shima T, Yamane K, Yamanaka C, Kagawa R (1999) Cylindrical or T-shaped silicone rubber stents for microanastomosis—technical note. Neurol Med Chir (Tokyo) 39:55–58
Ruan LT, Duan YY, Cao TS, Zhuang L, Huang L (2006) Color and power Doppler sonography of extracranial and intracranial arteries in Moyamoya disease. J Clin Ultrasound 34:60–69
Suzuki J, Kodama N (1983) Moyamoya disease: a review. Stroke 14:104–109
Suzuki J, Takaku A (1969) Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol 20:288–299
Takanashi J (2011) Moyamoya disease in children. Brain Dev 33:229–234
Takase K, Kashihara M, Hashimoto T (1997) Transcranial Doppler ultrasonography in patients with moyamoya disease. Clin Neurol Neurosurg 99(Suppl 2):S101–S105
Yamaguchi K, Kawamata T, Kawashima A, Hori T, Okada Y (2010) Incidence and predictive factors of cerebral hyperperfusion after extracranial–intracranial bypass for occlusive cerebrovascular diseases. Neurosurgery 67:1548–1554
Acknowledgments
We thank the radiological technicians at the Departments of Neurosurgery and Radiology, Tokyo Women’s Medical University, Tokyo, Japan, for measurements of rCBF and CVR on cold Xe-CT. This study was supported by research funds of the Department of Neurosurgery, Tokyo Women’s Medical University.
Conflict of interest
All authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Yasuhiro Yonekawa, Zürich, Switzerland
Morisawa et al. are to be congratulated for delivering interesting information concerning the hemodynamics of cortical flow in three different cerebrovascular occlusive diseases, PMMD, AMMD, and ACVD, in comparison with a control group obtained at the time of aneurysm surgery. These examinations have been done with the aid of micro-Doppler sonography that we are using only to check vascular patency, especially after construction of an EC–IC bypass or in aneurysm surgery. Originally, the authors advocated the theory that the increase of the post-anastomotic V max could predict a hyperperfusion syndrome; however, they somewhat toned down, presumably due to an insufficient number of cases, stating that their finding may help in preventing this undesirable complication. To be honest, I miss some additional explanation or speculation about the mechanism responsible for such hemodynamic differences between patients with moyamoya disease, both pediatric and adult, or between moyamoya and atherosclerotic occlusive disease, even though some information regarding leptmeningeal anastomosis and rCVR has been given. Perhaps such an explanation could be possible with additional data obtained by measuring the intraarterial pressure or the local rCBF with the use of a thermocouple [1, 2]. Such measurements would also furnish evidence of changes in cortical flow direction after bypass surgery.
Table
V max: cortical flow | Retrograde flow | ∆V max | |
|---|---|---|---|
PMMD | ⇒ | +++ | + |
AMMD | ⇓ | ++ | +++ |
ACVD | ⇒ | + | ++ |
References
1 Yonekawa Y: Brain vascularization by extracranial–intracranial arterial bypass. In Sindou M (ed). Practical hand book of neurosurgery. Vol 1. Springer, Wien, 2009, pp 355-381
2 Ogata N, Fournier JY, Imhof HG, Yonekawa Y: Thermal diffusion blood flow monitoring during aneurysm surgery. Acta Neurochir (Wien) 138: 726-731, 1996
Kiyohiro Houkin, Sapporo, Japan
The authors clearly have demonstrated quantitative flow measurement in moyamoya disease using micro-Doppler ultrasonography. This work is praiseworthy for clinical application. They have also revealed that in pediatric moyamoya cases, the cortical flow shows retrograde flow and its V max (systolic maximum flow velocity) is higher than the adult moyamoya cases. This may mean that retrograde flow due to the pial anastomosis in pediatric cases is well established than in adult case.
As it is well-known, the collateral flow is dependent on the stages of this disease. In addition, the flow dynamics may depend on its location (area of craniotomy). We have to be careful to evaluate these quantitative data. I am confident that the intraoperative flow measurement using micro-Doppler ultrasonography is practical and convenient in intraoperative flow measurement based on my personal experience. Moreover, the hyperperfusion that is a serious issue after successful direct bypass to moyamoya disease can be predicted using this very convenient tool. More additional clinical experience with this tool is necessary and the establishment of a standard way of reliable evaluation using this weapon is expected.
Rights and permissions
About this article
Cite this article
Morisawa, H., Kawamata, T., Kawashima, A. et al. Hemodynamics and changes after STA–MCA anastomosis in moyamoya disease and atherosclerotic cerebrovascular disease measured by micro-Doppler ultrasonography. Neurosurg Rev 36, 411–419 (2013). https://doi.org/10.1007/s10143-012-0441-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-012-0441-y