Abstract
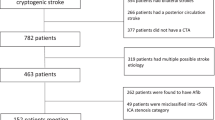
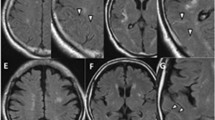
Mobile plaque is associated with increased risk of ischemic stroke, but definitions have remained unclear. We have previously reported that carotid ultrasonography can detect the mobile component of the carotid plaque surface, which rises and falls in a manner inconsistent with arterial pulsatile wall motion (Jellyfish sign). However, clinical and pathological features of Jellyfish sign remain unclear. The subjects comprised of 165 patients with carotid plaque and degree of area stenosis ≥50% on ultrasonography. Using magnetic resonance imaging, we quantified intraplaque hemorrhage (IPH) and defined ischemic stroke in each patient. Fifteen surgical specimens were obtained by carotid endarterectomy, and pathological features (area of fibrous cap and intraplaque atheromatous lesion) were compared with ultrasonographic plaque surface movement rate. Carotid plaques with IPH were seen in 78 cases, with Jellyfish sign in 31 cases. Jellyfish sign was not detected in patients without IPH. In these 15 patients, the fibrous cap covered the atheromatous lesion, and cap thickness correlated negatively with Jellyfish-positive plaque surface movement rate. Kaplan–Meier and Cox multiple regression analysis demonstrated that the most important predictor of ischemic stroke during follow-up is Jellyfish sign, not IPH. Stroke events in patients with Jellyfish sign repeated within a short interval after diagnosis. Jellyfish sign on ultrasonography is a sign of high-risk plaque vulnerability, suggesting rupture of the fibrous cap associated with the release of thrombogenic factors into the arterial lumen, and resulting in repeated ischemic stroke during a short interval after diagnosis.







Similar content being viewed by others
References
Altaf N, MacSweeney ST, Gladman J, Auer DP (2007) Carotid intraplaque hemorrhage predicts recurrent symptoms in patients with high-grade carotid stenosis. Stroke 38:1633–1635
Barnett HJM, Taylor DW, Eliasziw M, Fox AJ, Ferguson GG, Haynes RB, Rankin RN, Clagett GP, Hachinski VC, Sackett DL, Thorpe KE, Meldrum HE, Spence JD, for The North American Symptomatic Carotid Endarterectomy Trial Collaborators (1998) Benefit of carotid endarterectomy in patients with symptomatic moderate or severe stenosis. N Engl J Med 339:1415–1425
Carr S, Farb A, Pearce WH, Virmani R, Yao JS (1996) Atherosclerotic plaque rupture in symptomatic carotid artery stenosis. J Vasc Surg 23:755–765
Constantinides P (1966) Plaque fissures in human coronary thrombosis. J Atheroscler Res 6:1–17
Davies MJ, Thomas AC (1985) Plaque fissuring—the cause of acute myocardial infarction, sudden ischaemic death, and crescendo angina. Br Heart J 53:363–373
Devuyst G, Karapanayiotides T, Ruchat P, Pusztaszeri M, Lobrinus JA, Jonasson L, Cuisinaire O, Kalangos A, Despland PA, Thiran JP, Bogousslavsky J (2005) Ultrasound measurement of the fibrous cap in symptomatic and asymptomatic atheromatous carotid plaques. Circulation 111:2776–2782
Eliasziw M, Kennedy J, Hill MD, Buchan AM, Barnett HJM, for the North American Symptomatic Carotid Endarterectomy Trial (NASCET) Group (2004) Early risk of stroke after a transient ischemic attack in patients with internal carotid artery disease. CMAJ 170:1105–1109
European Carotid Surgery Trialists' Collaborative Group (1998) Randomised trial of endarterectomy for recently symptomatic carotid stenosis: final results of the MRC European Carotid Surgery Trial (ECST). Lancet 351:1379–1387
Grogan JK, Shaalan WE, Cheng H, Gewertz B, Desai T, Schwarze G, Glagov S, Lozanski L, Griffin A, Castilla M, Bassiouny HS (2005) B-mode ultrasonographic characterization of carotid atherosclerotic plaques in symptomatic and asymptomatic patients. J Vasc Surg 42:435–441
Hatsukami TS, Ross R, Polissar NL, Yuan C (2000) Visualization of fibrous cap thickness and rupture in human atherosclerotic carotid plaque in vivo with high-resolution magnetic resonance imaging. Circulation 102:959–964
Kobayashi M, Ogasawara K, Inoue T, Saito H, Komoribayashi N, Suga Y, Ogawa A (2007) Urgent endarterectomy using pretreatment with free radical scavenger, edaravone, and early clamping of the parent arteries for cervical carotid artery stenosis with crescendo transient ischemic attacks caused by mobile thrombus and hemodynamic cerebral ischemia. Case report. Neurol Med Chir (Tokyo) 47:121–125
Kume S, Hibino S, Kobayashi M, Kanazawa J, Mihara C, Yamane K, Toyota A, Onda H, Kurisu K (2007) Jellyfish sign: deformation of plaque in the carotid artery due to pulsatile blood flow. Neurosonology 20:21–24, Japanese
Li ZY, Howarth SP, Tang T, Gillard JH (2006) How critical is fibrous cap thickness to carotid plaque stability? A flow-plaque interaction model. Stroke 37:1195–1199
Lovett JK, Gallagher PJ, Hands LJ, Walton J, Rothwell PM (2004) Histological correlates of carotid plaque surface morphology on lumen contrast imaging. Circulation 110:2190–2197
Meairs S, Hennerici M (1999) Four-dimensional ultrasonographic characterization of plaque surface motion in patients with symptomatic and asymptomatic carotid artery stenosis. Stroke 30:1807–1813
Nighoghossian N, Derex L, Douek P (2005) The vulnerable carotid artery plaque: current imaging methods and new perspectives. Stroke 36:2764–2772
Redgrave JN, Gallagher P, Lovett JK, Rothwell PM (2008) Critical cap thickness and rupture in symptomatic carotid plaques: the oxford plaque study. Stroke 39:1722–1729
Redgrave JN, Lovett JK, Gallagher PJ, Rothwell PM (2006) Histological assessment of 526 symptomatic carotid plaques in relation to the nature and timing of ischemic symptoms: the Oxford plaque study. Circulation 113:2320–2328
Richardson PD (1992) Physical factors affecting the atherosclerotic plaque. In: Labs KH, Jäger KA, Fitzgerald DE, Neuerburg-Heusler D (eds) Diagnostic Vascular Ultrasound. Edward Arnold, London, pp 33–41
Rothwell PM, Eliasziw M, Gutnikov SA, Warlow CP, Barnett HJ (2004) Carotid Endarterectomy Trialists Collaboration. Endarterectomy for symptomatic carotid stenosis in relation to clinical subgroups and timing of surgery. Lancet 363:915–924
Rothwell PM, Gibson R, Warlow CP (2000) Interrelation between plaque surface morphology and degree of stenosis on carotid angiograms and the risk of ischemic stroke in patients with symptomatic carotid stenosis. On behalf of the European Carotid Surgery Trialists' Collaborative Group. Stroke 31:615–621
Spagnoli LG, Mauriello A, Sangiorgi G, Fratoni S, Bonanno E, Schwartz RS, Piepgras DG, Pistolese R, Ippoliti A, Holmes DR Jr (2004) Extracranial thrombotically active carotid plaque as a risk factor for ischemic stroke. JAMA 292:1845–1852
Takaya N, Yuan C, Chu B, Saam T, Underhill H, Cai J, Tran N, Polissar NL, Isaac C, Ferguson MS, Garden GA, Cramer SC, Maravilla KR, Hashimoto B, Hatsukami TS (2006) Association between carotid plaque characteristics and subsequent ischemic cerebrovascular events: a prospective assessment with MRI—initial results. Stroke 37:818–823
Virmani R, Kolodgie FD, Burke AP, Farb A, Schwartz SM (2000) Lessons from sudden coronary death: a comprehensive morphological classification scheme for atherosclerotic lesions. Arterioscler Thromb Vasc Biol 20:1262–1275
Yonemura K, Kimura K, Yasaka M, Minematsu K (2003) Disappearance of an oscillating intraluminal thrombus in the carotid artery demonstrated by ultrasonography. Intern Med 42:746–749
Yuan C, Zhang SX, Polissar NL, Echelard D, Ortiz G, Davis JW, Ellington E, Ferguson MS, Hatsukami TS (2002) Identification of fibrous cap rupture with magnetic resonance imaging is highly associated with recent transient ischemic attack or stroke. Circulation 105:181–185
Acknowledgements
The authors thank Masuki Kobayashi, M.D., Junichi Kanazawa, M.D., Seiichirou Hibino, M.D., Chie Mihara, M.D. (Hibino Hospital), and Akihiro Toyota, M.D. (Chugoku Rosai Hospital), for the collection of follow-up data and helpful comments.
Financial Disclosure
None
Grant Information
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Dorothea Miller, Ulrich Sure, Essen, Germany
Kume and colleagues demonstrated in this article how ultrasonography might help in predicting the risk of ischemic stroke in patients with carotid stenosis.
Ultrasound was performed to determine plaque morphology in cases of carotid stenosis. Ultrasound features with focus on plaque surface movement (Jellyfish sign) were compared with pathological features in 15 surgical specimens. Moreover, MRI was used to quantify intraplaque hemorrhage, as well as ischemic stroke.
The authors could show that Jellyfish sign was only detected in cases with intraplaque hemorrhage on MRI. Jellyfish sign was negatively correlated to fibrous cap thickness in surgical specimens. Statistical analysis revealed Jellyfish sign as the most important predictor of ischemic stroke during follow-up.
The idea that unstable or ruptured atheromatous plaques bear an increased risk of stroke is not new. However, little has been published on ultrasound diagnostics of unstable plaques, as well as its predictive value for ischemic stroke. Carotid ultrasonography is an inexpensive and widely available diagnostic tool. Thus, the study presented by the authors is highly relevant for clinical practice.
However, there are some limitations of the study. The authors do not correlate signs of plaque rupture directly on ultrasound and MRI. Correlations with pathological specimens could only be performed in a small number of cases.
Thus, the ultrasound feature termed “Jellyfish sign” by the authors could be an important predictive sign in patients at risk of stroke, although further validation of the methodology will still be necessary.
Kazunori Arita, Kagoshima, Japan
The development of ultrasonographic scanning of the carotid artery has provided valuable information on the pathophysiologic nature of atheromatous plaques of the cervical carotid arteries. Ultrasonographically identified floating plaques are a well-known risk factor for ischemic stroke. The authors describe the rise and fall motion of the carotid plaque surface that is inconsistent with arterial pulsatile wall motion. This, a finding different from floating plaque, they name the “Jellyfish sign”. They found that this movement predicts the early recurrence of stroke and postulate that the Jellyfish sign is a result of plaque rupture associated with the continuous release of thrombogenic factors into the arterial lumen. Their findings may contribute significantly to the proper management of carotid artery stenosis. They also suggest that the early surgical treatment of plaques exhibiting the Jellyfish sign is justified, especially in patients with recurrent ischemic stroke during a short period of time.
As the authors indicate, their current findings must be confirmed in large cohorts that include patients with less than 50% stenosis. Changes in the Jellyfish sign in the long run and the response to medical treatment with, for example, statins, may be the next study targets.
Electronic supplementary materials
Below is the link to the electronic supplementary material.
Digital video of plaque surface motion of Jellyfish sign in Case 1. Arrow shows the Jellyfish sign-positive part. CCA common carotid artery, ICA internal carotid artery. (MPG 1307 kb)
Digital video of plaque surface motion of Jellyfish sign in Case 2. Arrow shows the Jellyfish sign-positive part. CCA common carotid artery, ICA internal carotid artery. (MPG 546 kb)
Rights and permissions
About this article
Cite this article
Kume, S., Hama, S., Yamane, K. et al. Vulnerable carotid arterial plaque causing repeated ischemic stroke can be detected with B-mode ultrasonography as a mobile component: Jellyfish sign. Neurosurg Rev 33, 419–430 (2010). https://doi.org/10.1007/s10143-010-0270-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-010-0270-9