Abstract
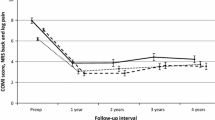
The authors determined current health status of patients who had been included in a long-term survivorship analysis of a lumbar dynamic stabilizer. Among 133 living patients, 107 (average age at surgery, 44.2 ± 9.9 years) completed health questionnaires. All patients had initially been scheduled for decompression and fusion for canal stenosis, herniated disc, or both. In 20 patients, the implant was removed, and fusion was performed. The other 87 still had the dynamic stabilizer. Satisfaction, Oswestry disability index, visual analog scales for back and leg pain, short-form (SF-36) quality-of-life physical composite score, physical function, and social function were significantly better (p ≤ 0.05) in the patients who still had the dynamic stabilization device. SF-36 scores of the fused subgroup were no worse than those reported elsewhere in patients who had primary pedicle-screw enhanced lumbar fusion. This anatomy-sparing device provided a good 13-year clinical outcome and obviated arthrodesis in 80% of patients.



Similar content being viewed by others
References
Ala-Kokko L (2002) Genetic risk factors for lumbar disc disease. Ann Med 34:42–47
Borenstein DG, O’Mara JW Jr, Boden SD et al (2001) The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects: a seven-year follow-up study. J Bone Joint Surg Am 83-A:1306–1311
Calmels P, Bethoux F, Condemine A et al (2005) Low back pain disability assessment tools. Ann Readapt Med Phys 48:288–297
David T (2007) Long-term results of one-level lumbar arthroplasty: minimum 10-year follow-up of the CHARITE artificial disc in 106 patients. Spine 32:661–666
Elfering A, Semmer N, Birkhofer D et al (2002) Risk factors for lumbar disc degeneration: a 5-year prospective MRI study in asymptomatic individuals. Spine 27:125–134
Etminan M, Girardi FP, Khan SN et al (2002) Revision strategies for lumbar pseudarthrosis. Orthop Clin North Am 33:381–392
Ghiselli G, Wang JC, Bhatia NN et al (2004) Adjacent segment degeneration in the lumbar spine. J Bone Joint Surg Am 86-A:1497–1503
Glaser J, Stanley M, Sayre H et al (2003) A 10-year follow-up evaluation of lumbar spine fusion with pedicle screw fixation. Spine 28:1390–1395
Guehring T, Omlor GW, Lorenz H et al (2006) Disc distraction shows evidence of regenerative potential in degenerated intervertebral discs as evaluated by protein expression, magnetic resonance imaging, and messenger ribonucleic acid expression analysis. Spine 31:1658–1665
Guigui P, Wodecki P, Bizot P et al (2000) [Long-term influence of associated arthrodesis on adjacent segments in the treatment of lumbar stenosis: a series of 127 cases with 9-year follow-up]. Rev Chir Orthop Reparatrice Appar Mot 86:546–557
Hartigan C, Rainville J, Sobel JB et al (2000) Long-term exercise adherence after intensive rehabilitation for chronic low back pain. Med Sci Sports Exerc 32:551–557
Katz JN, Lipson SJ, Chang LC et al (1996) Seven- to 10-year outcome of decompressive surgery for degenerative lumbar spinal stenosis. Spine 21:92–98
Kawaguchi Y, Ishihara H, Kanamori M et al (2007) Adjacent segment disease following expansive lumbar laminoplasty. Spine J 7:273–279
Keller SD, Ware JE Jr, Bentler PM et al (1998) Use of structural equation modeling to test the construct validity of the SF-36 health survey in ten countries: results from the IQOLA project. International quality of life assessment. J Clin Epidemiol 51:1179–1188
Khoueir P, Kim KA, Wang MY (2007) Classification of posterior dynamic stabilization devices. Neurosurg Focus 22:E3
Kroeber M, Unglaub F, Guehring T et al (2005) Effects of controlled dynamic disc distraction on degenerated intervertebral discs: an in vivo study on the rabbit lumbar spine model. Spine 30:181–187
Lemaire JP, Carrier H, Sariali el H et al (2005) Clinical and radiological outcomes with the Charite artificial disc: a 10-year minimum follow-up. J Spinal Disord Tech 18:353–359
Leplege A, Ecosse E, Verdier A et al (1998) The French SF-36 health survey: translation, cultural adaptation and preliminary psychometric evaluation. J Clin Epidemiol 51:1013–1023
Martin BI, Mirza SK, Comstock BA et al (2007) Are lumbar spine reoperation rates falling with greater use of fusion surgery and new surgical technology? Spine 32:2119–2126
Okuda S, Miyauchi A, Oda T et al (2006) Surgical complications of posterior lumbar interbody fusion with total facetectomy in 251 patients. J Neurosurg Spine 4:304–309
Pellise F, Hernandez A, Vidal X et al (2007) Radiologic assessment of all unfused lumbar segments 7.5 years after instrumented posterior spinal fusion. Spine 32:574–579
Rohlmann A, Neller S, Bergmann G et al (2001) Effect of an internal fixator and a bone graft on intersegmental spinal motion and intradiscal pressure in the adjacent regions. Eur Spine J 10:301–308
Senegas J (1991) Surgery of the intervertebral ligaments, alternative to arthrodesis in the treatment of degenerative instabilities. Acta Orthop Belg 57(Suppl 1):221–226
Senegas J (2002) Mechanical supplementation by non-rigid fixation in degenerative intervertebral lumbar segments: the Wallis system. Eur Spine J 11(Suppl 2):S164–S169
Senegas J, Vital JM, Pointillart V et al (2007) Long-term actuarial survivorship analysis of an interspinous stabilization system. Eur Spine J 16:1279–1287
Shono Y, Kaneda K, Abumi K et al (1998) Stability of posterior spinal instrumentation and its effects on adjacent motion segments in the lumbosacral spine. Spine 23:1550–1558
Videman T, Battie MC, Ripatti S et al (2006) Determinants of the progression in lumbar degeneration: a 5-year follow-up study of adult male monozygotic twins. Spine 31:671–678
Wilke H-J, Drumm J, Haeussler K, et al (2007) Biomechanical comparison of the segmental stability and intradiscal pressure achieved with different interspinous implants. In: 53rd annual meeting of the Orthopaedic Research Society. Orthopaedic Research Society, San Diego, CA, p 88
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Luciano Mastronardi, Roma, Italy
This is a very interesting article on a large series of patients with various type of lumbar instabilities treated with the interspinous device Wallis. I think any spine surgeon would find the data analysis complete, the follow-up adequate, and the results promising.
Even if I am not completely convinced that the interspinous device Wallis, which I use time by time, can avoid a lumbar fusion in a very high percentage of cases, I think that the readers will enjoy this experience. A multicenter, randomized study comparing the results of standard fixation and interspinous techniques would be very useful for the future.
Hatem Sabry, Jack Jallo, Philadelphia, USA
The authors of this article have conducted a retrospective study aimed at evaluating the health status of the patients who underwent a lumbar dynamic stabilization procedure. This is a well-written article covering a relatively large number of patients treated with the Wallis dynamic stabilizer and with a long-term follow-up of 13 years.
The authors concluded that the patients had excellent clinical results in terms of pain, disability, and quality of life. The question that comes to mind of course after reading this article is how these patients would compare to others managed conservatively. The answer to this would ideally be provided by a randomized, controlled study.
Yet, we cannot ignore that this study brings to light an important, less invasive, and somewhat underestimated alternative to traditional decompression and fusion of the spinal canal.
Li-Yang Dai, Shanghai, China
Senegas et al. provided a relatively large series of patients treated with interspinous process spacers for degenerative disorders of the lumbar spine. Their results of long-term follow-up are interesting and show success in the patients with implants survived. This clinical report suggests that satisfactory long-term results could be achieved when these devices are applied in appropriately selected patients. I congratulate the authors on adding to our knowledge in lumbar spine surgery.
As the authors pointed out, this study might be limited in its retrospective nature. It is difficult to determine whether the improvement of the clinical symptoms is the result of decompression or dynamic stabilization, or both of them. Therefore, a randomized, controlled study should be required for comparing the results between interspinous device insertion and fusion, although the authors found that better clinical outcome was noted at follow-up in the patients who still had the dynamic stabilizer than the patients who received subsequent fusion.
Another limitation of this study might be the heterogeneity of enrolled patients with regard to surgical indications. As generally believed, the interspinous process spacers are indicated for the patients with neurogenic claudication resulting from lumbar spinal stenosis. Our previous study showed that the capacity of the spinal canal is influenced by flexion-extension motion of the lumbar spine with a significant increase from extension to flexion (1). The advantage of using interspinous process spacers may lie in the enlargement of the spinal canal and decrease in painful motion by restricting the extension or increasing the flexion of lumbar spine. So far, as we know, there are no studies showing that interspinous process spacer insertion would be more advantageous than simple discectomy in the treatment of disc herniation. In fact, recurrence of disc herniation after the use of interspinous process devices in the primary discectomy has been reported (2). Concern remains regarding the role of the interspinous process spacers in the treatment of disc herniation.
References
1. Dai LY, Xu YK, Zhang WM, Zhou ZH (1989) The effect of flexion-extension motion of the lumbar spine on the capacity of the spinal canal: an experimental study. Spine 14:523–525
2. Floman Y, Millgram MA, Smorgick Y, Rand N, Ashkenazi E (2007) Failure of the Wallis interspinous implant to lower the incidence of recurrent lumbar disc herniations in patients undergoing primary disc excision. J Spinal Disord Tech 20:337–341
All index operations were performed in the Unité de Pathologie Rachidienne, Centre Hospitalier Pellegrin, Bordeaux.
Rights and permissions
About this article
Cite this article
Sénégas, J., Vital, JM., Pointillart, V. et al. Clinical evaluation of a lumbar interspinous dynamic stabilization device (the Wallis system) with a 13-year mean follow-up. Neurosurg Rev 32, 335–342 (2009). https://doi.org/10.1007/s10143-009-0199-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-009-0199-z