Abstract
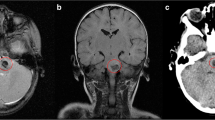
Hemorrhages of brainstem cavernomas may cause severe neurological deficits. Surgical strategies are frequently described, and advanced neuromonitoring with intraoperative imaging can help neurosurgeons to achieve good results. However, patients are often confronted with significant therapeutic risks by the primary doctor before talking to an experienced brainstem neurosurgeon. On the other hand, lethal progression with repeated hemorrhages is rarely described, although many would agree on this possibility by experience or assumption. Our reported case represents the natural development of a patient with repeated hemorrhages of a brainstem cavernoma and consequently increasing neurological deterioration, which led to a fatal ending. After two recurrent hemorrhages, the patient and his family declined twice the offered surgical procedures to evacuate the hematoma of the pons. The patient died after three noticed hemorrhages of the same brainstem cavernoma and their consecutive consequences. This case report represents one possible clinical scenario for consultation for brainstem cavernoma procedures.




Similar content being viewed by others
References
Aiba T, Tanaka R, Koike T et al (1995) Natural history of intracranial cavernous malformations. J Neurosurg 83:56–59
Bertalanffy H, Benes L, Miyazawa T et al (2002) Cerebral cavernous in the adult. Review of the literature and analysis of 72 surgically treated patients. Neurosurg Rev 25:1–53
Curling OD, Kelly DL, Elster AD, Craven TE (1991) An analysis of the natural history of cavernous angiomas. J Neurosurg 75:702–705
Fahlbusch R, Strauss C, Huk W et al (1990) Surgical removal of pontomesencephalic cavernous hemangiomas. Neurosurgery 26:449–457
Ferroli P, Sinisi M, Franzini A, Giombini S, Solero CL, Broggi G (2005) Brainstem cavernomas: long-term results of microsurgical resection in 52 patients. Neurosurgery 56(6):1203–1212, Jun
Giombini S, Morello G (1978) Cavernous angiomas of the brain; account of 14 personal cases and review of the literature. Acta Neurochir 40:61–82
Houtteville JP (1997) Brain cavernoma; a dynamic lesion. Surg Neurol 48:610–614
Porter RW, Detwiler PW, Spetzler RF, Lawton MT, Baskin JJ, Derksen PT, Zabramski JM (1999) Cavernous malformations of the brainstem: experience with 100 patients. J Neurosurg 90(1):50–58, Jan
Robinson JR, Awad IA, Little JR (1991) Natural history of the cavernous angioma. J Neurosurg 75:709–714
Sakay N, Yamada H, Tanigawara T et al (1991) Surgical treatment of cavernous angioma involving the brainstem and review of the literature. Acta Neurchir 113:138–143
Samii M, Eghbal A, Carvalo A, Matthies C (2001) Surgical management of brain stem cavernomas. J Neurosurg 95:825–832
Author information
Authors and Affiliations
Corresponding author
Additional information
Comments
Siddharth Kharkar, Daniele Rigamonti, Baltimore, MD, USA
The authors present the tragic case of a patient with multiple brain cavernomas, including one in the brainstem. The patient refused surgical removal of the cavernoma because of the perceived risks of such a procedure. Three documented hemorrhages severely disabled the patient, ultimately causing his death.
This is a well-written and balanced report. The authors are to be congratulated for highlighting the paucity of data reflecting different management strategies for these lesions.
It is a complex task to choose the appropriate management strategy for brainstem cavernomas. On one hand, their surgical resection is challenging, and on the other, the consequences of a bleed in this location can be catastrophic. Hence, we completely agree with the author’s assertion that the neurosurgeon’s experience should play a major role in determining the treatment strategy.
However, even if the neurosurgeon is comfortable operating on these lesions, what information does he/she have to choose the best management strategy? As the authors note, there is very little or no information on conservative/radiosurgical management of brainstem cavernomas, both symptomatic and asymptomatic. Without doubt, there is a serious publication bias in this field. We believe that the selective publication of surgically managed patients with severe symptoms creates a significant bias in the neurosurgeon’s mind about management of the individual patient.
The tragic case presented by the authors needs to be interpreted in this light. Although failure to resect the cavernoma resulted in catastrophic consequences in this patient, it would be a giant leap to generalize results from one patient to the entire population of patients with brainstem cavernomas.
What are the long-term effects of conservatively managing accidentally discovered, completely asymptomatic brainstem cavernomas? At what point does surgical resection become imperative? In an individual patient, are there factors (such as the presence or type of CCM mutation) that can dependably predict the course of the cavernoma and hence help in customizing treatment?
Definitive answers to these questions are sorely lacking.
Ulrich Sure, Marburg, Germany
The case reported by Ciurea et al. is a highly interesting contribution to the literature on cerebral and in particular on brain stem cavernomas. The vast majority of publications on this topic describe the various treatment strategies, their clinical course and outcome after treatment, and, to a lesser extent, their biological capabilities [1–5]. Although we have learned that cavernomas are not static and inherited but rather active and acquired lesions that may develop spontaneously or after prior irradiation [3, 4], we must state that their clinical danger cannot be derived from their biological ability but must attributed to their potential to cause hemorrhages that are responsible for severe morbidity, and, as in the present case, mortality [1, 2, 5].
The surgical indication for intrinsic brain stem surgery is very difficult to be set and should only be made by an experienced microsurgeon. Within the group of pathologies that can affect the brain stem, cavernomas are the most promising lesions with respect to the clinical outcome of a larger series [1, 2, 5]. The risk for surgical morbidity, however, still remains high also for brain stem cavernomas [1, 2, 5]. Therefore, the present fatal case after conservative treatment (that could be treated mircosurgically, for example, by a subtemporal transtentorial approach) might help to increase a surgeon´s confidence for treatment in difficult cases, because it clearly shows what might happen without surgical treatment. In myopinion, this publication demonstrates that a brain stem cavernoma patient should not be pre-informed and influenced by a referring colleague but should rather be introduced to the situation and advised by an experienced brain stem surgeon who, optimally, would be able to report on her/his positive personal experience. In our experience, this strategy was beneficial for all patients (>100) that were examined at our institution.
References
1. Bertalanffy H, Benes L, Miyazawa T, Alberti O, Siegel AM, Sure U (2002) Cerebral cavernomas in the adult. Review of the literature and analysis of 72 surgically treated patients. Neurosurg Rev 25(1–2):1–53
2. Fritschi JA, Reulen HJ, Spetzler RF, Zabramski JM (1994) Cavernous malformations of the brain stem. A review of 139 cases. Acta Neurochir (Wien) 130(1–4):35–46
3. Kilic T, Pamir MN, Kullu S, Eren F, Ozek MM, Black PM (2000) Expression of structural proteins and angiogenic factors in cerebrovascular anomalies. Neurosurgery 46(5):1179–1191
4. Sure U, Freman S, Bozinov O, Benes L, Siegel AM, Bertalanffy H (2005) Biological activity of adult cavernous malformations: a study of 56 patients. J Neurosurg 102(2):342–347.
5. Wang CC, Liu A, Zhang JT, Sun B, Zhao YL (2003) Surgical management of brain-stem cavernous malformations: report of 137 cases. Surg Neurol 59(6):444–454
Rights and permissions
About this article
Cite this article
Ciurea, A.V., Nastase, C., Tascu, A. et al. Lethal recurrent hemorrhages of a brainstem cavernoma. Neurosurg Rev 30, 259–262 (2007). https://doi.org/10.1007/s10143-007-0075-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10143-007-0075-7