Abstract
Purpose
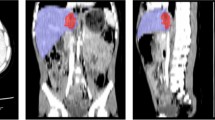
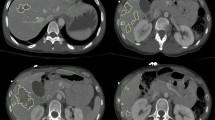
We employ nnU-Net, a state-of-the-art self-configuring deep learning-based semantic segmentation method for quantitative visualization of hemothorax (HTX) in trauma patients, and assess performance using a combination of overlap and volume-based metrics. The accuracy of hemothorax volumes for predicting a composite of hemorrhage-related outcomes — massive transfusion (MT) and in-hospital mortality (IHM) not related to traumatic brain injury — is assessed and compared to subjective expert consensus grading by an experienced chest and emergency radiologist.
Materials and methods
The study included manually labeled admission chest CTs from 77 consecutive adult patients with non-negligible (≥ 50 mL) traumatic HTX between 2016 and 2018 from one trauma center. DL results of ensembled nnU-Net were determined from fivefold cross-validation and compared to individual 2D, 3D, and cascaded 3D nnU-Net results using the Dice similarity coefficient (DSC) and volume similarity index. Pearson’s r, intraclass correlation coefficient (ICC), and mean bias were also determined for the best performing model. Manual and automated hemothorax volumes and subjective hemothorax volume grades were analyzed as predictors of MT and IHM using AUC comparison. Volume cut-offs yielding sensitivity or specificity ≥ 90% were determined from ROC analysis.
Results
Ensembled nnU-Net achieved a mean DSC of 0.75 (SD: ± 0.12), and mean volume similarity of 0.91 (SD: ± 0.10), Pearson r of 0.93, and ICC of 0.92. Mean overmeasurement bias was only 1.7 mL despite a range of manual HTX volumes from 35 to 1503 mL (median: 178 mL). AUC of automated volumes for the composite outcome was 0.74 (95%CI: 0.58–0.91), compared to 0.76 (95%CI: 0.58–0.93) for manual volumes, and 0.76 (95%CI: 0.62–0.90) for consensus expert grading (p = 0.93). Automated volume cut-offs of 77 mL and 334 mL predicted the outcome with 93% sensitivity and 90% specificity respectively.
Conclusion
Automated HTX volumetry had high method validity, yielded interpretable visual results, and had similar performance for the hemorrhage-related outcomes assessed compared to manual volumes and expert consensus grading. The results suggest promising avenues for automated HTX volumetry in research and clinical care.

Similar content being viewed by others
Data availability
Labeled dataset has not been made available at this time.
Code availability
Code can be made available on github.
References
Mowery NT, Gunter OL, Collier BR, Jose’J D Jr, Haut E, Hildreth A, Holevar M, Mayberry J, Streib E (2011) Practice management guidelines for management of hemothorax and occult pneumothorax. J Trauma Acute Care Surg 70(2):510–518
Sangster GP, González-Beicos A, Carbo AI, Heldmann MG, Ibrahim H, Carrascosa P, Nazar M, D’Agostino HB (2007) Blunt traumatic injuries of the lung parenchyma, pleura, thoracic wall, and intrathoracic airways: multidetector computer tomography imaging findings. Emerg Radiol 14(5):297–310
Mahmood I, Abdelrahman H, Al-Hassani A, Nabir S, Sebastian M, Maull K (2011) Clinical management of occult hemothorax: a prospective study of 81 patients. Am J Surg 201(6):766–769
Dreizin D, Munera F (2012) Blunt polytrauma: evaluation with 64-section whole-body CT angiography. Radiographics 32(3):609–631
Bilello JF, Davis JW, Lemaster DM (2005) Occult traumatic hemothorax: when can sleeping dogs lie? Am J Surg 190(6):844–848
Dreizin D, Munera F (2015) Multidetector CT for penetrating torso trauma: state of the art. Radiology 277(2):338–355
Demetri L, Aguilar MMM, Bohnen JD, Whitesell R, Yeh DD, King D, de Moya M (2018) Is observation for traumatic hemothorax safe? J Trauma Acute Care Surg 84(3):454–458
Stafford RE, Linn J, Washington L (2006) Incidence and management of occult hemothoraces. Am J Surg 192(6):722–726
Marts B, Durham R, Shapiro M, Mazuski JE, Zuckerman D, Sundaram M, Luchtefeld WB (1994) Computed tomography in the diagnosis of blunt thoracic injury. Am J Surg 168(6):688–692
Dreizin D, Bodanapally UK, Neerchal N, Tirada N, Patlas M, Herskovits E (2016) Volumetric analysis of pelvic hematomas after blunt trauma using semi-automated seeded region growing segmentation: a method validation study. Abdom Radiol 41(11):2203–2208
Battey TW, Dreizin D, Bodanapally UK, Wnorowski A, Issa G, Iacco A, Chiu W (2019) A comparison of segmented abdominopelvic fluid volumes with conventional CT signs of abdominal compartment syndrome in a trauma population. Abdom Radiol 44(7):2648–2655
Moy MP, Levsky JM, Berko NS, Godelman A, Jain VR, Haramati LB (2013) A new, simple method for estimating pleural effusion size on CT scans. Chest 143(4):1054–1059
Meyer DM (2007) Hemothorax related to trauma. Thorac Cardiovasc Surg 17(1):47–55
Huang J-F, Hsu C-P, Fu C-Y, Yang C-HO, Cheng C-T, Liao C-H, Kuo I-M, Hsieh C-H (2021) Is massive hemothorax still an absolute indication for operation in blunt trauma? Injury 52(2):225–30
Ma H-S, Ma J-H, Xue F-L, Fu X-N, Zhang N (2016) Clinical analysis of thoracoscopic surgery combined with intraoperative autologous blood transfusion in the treatment of traumatic hemothorax. Chin J Traumatol 19(6):371–372
Dreizin D, Zhou Y, Chen T, Li G, Yuille AL, McLenithan A, Morrison JJ (2020) Deep learning-based quantitative visualization and measurement of extraperitoneal hematoma volumes in patients with pelvic fractures: potential role in personalized forecasting and decision support. J Trauma Acute Care Surg 88(3):425–433
Dreizin D, Zhou Y, Zhang Y, Tirada N, Yuille AL (2020) Performance of a deep learning algorithm for automated segmentation and quantification of traumatic pelvic hematomas on CT. J Digit Imaging 33(1):243–251
Dreizin D, Zhou Y, Fu S, Wang Y, Li G, Champ K, Siegel E, Wang Z, Chen T, Yuille AL (2020) A multiscale deep learning method for quantitative visualization of traumatic hemoperitoneum at CT: assessment of feasibility and comparison with subjective categorical estimation. Radiol: Artif Intell 2(6):e190220
Fedorov A, Beichel R, Kalpathy-Cramer J, Finet J, Fillion-Robin J-C, Pujol S, Bauer C, Jennings D, Fennessy F, Sonka M (2012) 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn Reson Imaging 30(9):1323–1341
Mackenzie CF, Wang Y, Hu PF, Chen S-Y, Chen HH, Hagegeorge G, Stansbury LG, Shackelford S, Group OS (2014) Automated prediction of early blood transfusion and mortality in trauma patients. J Trauma Acute Care Surg 76(6):1379–85
Parimi N, Hu PF, Mackenzie CF, Yang S, Bartlett ST, Scalea TM, Stein DM (2016) Automated continuous vital signs predict use of uncrossed matched blood and massive transfusion following trauma. J Trauma Acute Care Surg 80(6):897–906. https://doi.org/10.1097/TA.0000000000001047
Litjens G, Kooi T, Bejnordi BE, Setio AAA, Ciompi F, Ghafoorian M, Van Der Laak JA, Van Ginneken B, Sánchez CI (2017) A survey on deep learning in medical image analysis. Med Image Anal 42:60–88
Fang X, Yan P (2020) Multi-organ segmentation over partially labeled datasets with multi-scale feature abstraction. IEEE Trans Med Imaging 39(11):3619–3629
Dreizin D, Chen T, Liang Y, Zhou Y, Paes F, Wang Y, Yuille AL, Roth P, Champ K, Li G, McLenithan A, Morrison JJ (2021) Added value of deep learning-based liver parenchymal CT volumetry for predicting major arterial injury after blunt hepatic trauma: a decision tree analysis. Abdom Radiol (NY) 46(6):2556–2566. https://doi.org/10.1007/s00261-020-02892-x
Zhou Y, Dreizin D, Li Y, Zhang Z, Wang Y, Yuille A (2019) Multi-scale attentional network for multi-focal segmentation of active bleed after pelvic fractures. In International Workshop on Machine Learning in Medical Imaging. Springer, Cham, pp 461–469
Zhou Y, Dreizin D, Wang Y, Liu F, Shen W, Yuille AL (2022) External attention assisted multi-phase splenic vascular injury segmentation with limited data. IEEE Trans Med Imaging 41(6):1346–1357. https://doi.org/10.1109/TMI.2021.3139637
Isensee F, Jaeger PF, Kohl SA, Petersen J, Maier-Hein KH (2021) nnU-Net: a self-configuring method for deep learning-based biomedical image segmentation. Nat Methods 18(2):203–211
Chartrand G, Cheng PM, Vorontsov E, Drozdzal M, Turcotte S, Pal CJ, Kadoury S, Tang A (2017) Deep learning: a primer for radiologists. Radiographics 37(7):2113–2131
Maier-Hein L, Reinke A, Christodoulou E, Glocker B, Godau P, Isensee F, Kleesiek J, Kozubek M, Reyes M, Riegler MA (2022) Metrics reloaded: pitfalls and recommendations for image analysis validation. arXiv preprint arXiv:2206.01653
Kessler LG, Barnhart HX, Buckler AJ, Choudhury KR, Kondratovich MV, Toledano A, Guimaraes AR, Filice R, Zhang Z, Sullivan DC (2015) The emerging science of quantitative imaging biomarkers terminology and definitions for scientific studies and regulatory submissions. Stat Methods Med Res 24(1):9–26
Zou KH, Tuncali K, Silverman SG (2003) Correlation and simple linear regression. Radiology 227(3):617–628
Hunter TB, Taljanovic MS, Krupinski E, Ovitt T, Stubbs AY (2007) Academic radiologists’ on-call and late-evening duties. J Am Coll Radiol 4(10):716–719
Brant-Zawadzki MN (2007) Special focus—outsourcing after hours radiology: one point of view—outsourcing night call. J Am Coll Radiol 4(10):672–674
Banaste N, Caurier B, Bratan F, Bergerot J-F, Thomson V, Millet I (2018) Whole-body CT in patients with multiple traumas: factors leading to missed injury. Radiology 289(2):374–383
Dreizin D, Bodanapally U, Boscak A, Tirada N, Issa G, Nascone JW, Bivona L, Mascarenhas D, O’Toole RV, Nixon E (2018) CT prediction model for major arterial injury after blunt pelvic ring disruption. Radiology 287(3):1061–1069
Borror W, Gaski GE, Steenburg S (2019) Abdominopelvic bleed rate on admission CT correlates with mortality and transfusion needs in the setting of blunt pelvic fractures: a single institution pilot study. Emerg Radiol 26(1):37–44
Dreizin D, Champ K, Dattwyler M, Bodanapally U, Smith EB, Li G, Singh R, Wang Z, Liang Y (2022) Blunt splenic injury in adults: association between volumetric quantitative CT parameters and intervention. J Trauma Acute Care Surg. https://doi.org/10.1097/TA.0000000000003684
Miller PR, Croce MA, Bee TK, Qaisi WG, Smith CP, Collins GL, Fabian TC (2001) ARDS after pulmonary contusion: accurate measurement of contusion volume identifies high-risk patients. J Trauma Acute Care Surg 51(2):223–230
Laughlin B, Chan A, Tai WA, Moftakhar P (2019) RAPID automated CT perfusion in clinical practice. Pract Neurol 2019:41–55
Zhang T, Song Z, Yang J, Zhang X, Wei J (2021) Cerebral hemorrhage recognition based on Mask R-CNN network. Sens Imaging 22(1):1–16
Zapaishchykova A, Dreizin D, Li Z, Wu JY, Faghihroohi S, Unberath M (2021) An interpretable approach to automated severity scoring in pelvic trauma. In International Conference on Medical Image Computing and Computer-Assisted Interventio. Springer, Cham, pp 424–433
Chen H, Gomez C, Huang C-M, Unberath M (2021) INTRPRT: a systematic review of and guidelines for designing and validating transparent AI in medical image analysis. arXiv preprint arXiv:2112.12596
Vlontzos A, Rueckert D, Kainz B (2022) A review of causality for learning algorithms in medical image analysis. arXiv preprint arXiv:2206.05498
Funding
1. NIH K08 EB027141-01A1 (PI: David Dreizin, MD).
2. Accelerated Translational Incubator Pilot (ATIP) award, University of Maryland (PI: David Dreizin, MD).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
IRB approval was obtained for this study at the University of Maryland School of Medicine.
Consent for study
The IRB waived informed consent due to retrospective observational nature and deidentified data.
Consent for publication
IRB approved waiver of informed consent for publication of observational study of deidentified data as above.
Conflict of interest
David Dreizin, MD, is founder of TraumaVisual, LLC.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Dreizin, D., Nixon, B., Hu, J. et al. A pilot study of deep learning-based CT volumetry for traumatic hemothorax. Emerg Radiol 29, 995–1002 (2022). https://doi.org/10.1007/s10140-022-02087-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-022-02087-5