Abstract
Background
The number of patients who die from causes other than gastric cancer after R0 resection is increasing in Japan, due in part to the aging population. However, few studies have comprehensively investigated the clinicopathological risks associated with deaths from other causes after gastrectomy. This study aimed to build a risk score for predicting such deaths.
Methods
We retrospectively reviewed clinical data for 3575 patients who underwent gastrectomy for gastric cancer at nine institutions in Japan between January 2010 and December 2014.
Results
The final study population of 1758 patients were assigned to Group A (n = 187): patients who died from other causes within 5 years of surgery, and Group B (n = 1571): patients who survived ≥ 5 years after surgery. Multivariate analysis identified nine characteristics as risk factors for poor survival: age ≥ 75 years, male sex, body mass index < 22 kg/m2, Eastern Cooperative Oncology Group Performance Status (≥ 1), diabetes mellitus, cardiovascular/cerebrovascular disease, other malignant diseases, preoperative albumin level < 3.5 g/dL, and total gastrectomy. Patients with risk scores of 0–2, 3–4, or 5–9 (based on 1 point per characteristics) were classified into Low-risk, Intermediate-risk, and High-risk groups, respectively. The 5-year survival rates were 96.5%, 85.3%, and 56.5%, for the Low-, Intermediate-, and High-risk groups, respectively, and the hazard ratio (95% confidence intervals) was 16.33 (10.85–24.58, p < 0.001) for the High-risk group.
Conclusions
The risk score defined here may be useful for predicting deaths from other causes after curative gastrectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In Japan, the number of deaths from gastric cancer began to decrease after 2013, which was the year in which eradication of Helicobacter pylori infection for the treatment of chronic gastritis was first covered under the National Health Insurance system [1]. However, these gains have been offset by the facts that the average age of the Japanese population has steadily risen and the number of gastrectomies performed on patients with a variety of comorbidities has also increased [2, 3]. Consequently, the total number of patients who die from other causes after curative gastrectomy has increased. Thus, to provide comprehensive care for patients with gastric cancer, it is essential that attention be paid not only to cure gastric cancer but also to manage other diseases.
Gastrectomy is a highly invasive surgery with nutrition-related complications that can lead to other life-threatening diseases such as pneumonia [4, 5]. Several studies have reported risk factors that predict postoperative nutritional disorders or pneumonia after gastrectomy [6,7,8,9]. However, few studies have comprehensively investigated the clinicopathological risk factors or compiled an overall risk score to predict death from other causes after gastrectomy. In this study, we have retrospectively analyzed a large dataset of patients who underwent curative gastrectomy with the aim of building a risk score for predicting death from causes other than gastric cancer.
Materials and methods
Patients
We retrospectively reviewed the clinical data for 3575 patients who underwent gastrectomy for gastric cancer at nine institutions in Japan between January 2010 and December 2014. The clinical and pathological stages were based on the TNM Classification of Malignant Tumors, 8th Edition [10]. This study conformed with the ethical guidelines of the World Medical Association Declaration of Helsinki-Ethical Principles for Medical Research Involving Human Subjects. Written informed consent for surgery and use of clinical data was obtained from all patients, as required by the Institutional Review Board of each participating institution. We employed opt-out recruitment according to the policy of the Japanese government because this clinical research was conducted using only retrospective clinical data without intervention. The purpose, design, and objectives of the study were posted on the homepage of the Nagoya University Graduate School of Medicine to provide an opportunity for patients to decline to contribute to our study.
Patient management
Patients underwent gastrectomy with D1 + or D2 lymphadenectomy according to the clinical stage, and the reconstruction method was selected at the surgeon’s discretion. Upper gastrointestinal endoscopy and contrast-enhanced chest and abdominal computed tomography (CT) were performed on all patients for preoperative staging, and magnetic resonance imaging was undertaken as considered necessary. Patients received postoperative follow-up that included physical examinations, laboratory tests, and enhanced CT (chest and abdominal cavity) once every 6 months for 5 years or until recurrence [11]. S-1 (an oral fluoropyrimidine derivative) monotherapy, or doublet chemotherapy was recommended as postoperative adjuvant treatment unless contraindicated by the patient’s condition or refusal [12, 13]. Treatment after recurrence was determined according to the information available at the time of treatment, the patient’s condition, and the patient’s consent [14, 15].
Statistical analysis
Qualitative variables were compared using the χ2 test, and quantitative variables were compared using the Mann–Whitney U test between two patient groups, and the Kruskal–Wallis test among three patient groups. Logistic regression analysis was used for the multivariate analysis. Survival rates were estimated using the Kaplan–Meier method. Hazard ratios (HRs) and 95% confidence intervals (CIs) were estimated using the Cox proportional hazards model. Statistical analysis was performed using EZR statistical software [16]. A p value of < 0.05 was considered statistically significant.
Results
Patient selection
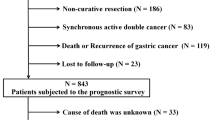
The flowchart of patient enrollment is shown in Fig. 1. We excluded a total of 1285 patients who died from postoperative complications during hospitalization (n = 29), had pathological stage IV (n = 366) or clinical stage IVB gastric cancer (n = 20), had recurrent gastric cancer (n = 505), had gastric stump cancer (n = 60), or had insufficient data for analysis (n = 305). In addition, we excluded 532 patients with follow-up shorter than 5 years. Finally, a total of 1758 patients were included as the study population and were assigned to two groups: those who died from other causes within 5 years after surgery (Group A, n = 187) and those who survived for ≥ 5 years after surgery (Group B, n = 1571).
Definitions of patient’s status and comorbidities
Age at the time of surgery was used for the risk score. Body mass index (BMI) and Eastern Cooperative Oncology Group Performance Status (ECOG-PS) were determined within 3 days before surgery. Serum albumin levels were measured within 14 days prior to surgery. Definitions and disease names for each comorbidity were presented in Supplementary Table 1. For hypertension and diabetes mellitus, patients who were receiving medical care such as diet control and medication at the time of surgery were selected. For cardiovascular diseases, patients having all heart diseases, macrovascular diseases such as abdominal aortic aneurysm and aortic dissection, and peripheral arterial diseases such as arteriosclerosis obliterans met the definitions. Basically, patients diagnosed by imaging or undergoing therapeutic intervention were included. For cerebrovascular diseases, patients with a history of cerebral hemorrhage, stroke, or transient ischemic attack were included. For respiratory diseases, patients who received treatment at the time of surgery or had previously received medical treatment, or had undergone a pulmonary resection. For other malignant diseases, concurrent or past history of malignant diseases other than gastric cancer were included.
Clinical characteristics
Table 1 shows the causes of death for patients in Group A. The most common causes of death were other malignant diseases (32.6%), respiratory diseases (19.8%), and cardiovascular/cerebrovascular diseases (12.3%). A comparison of the clinical characteristics of patients in Group A and Group B is shown in Supplementary Table 2. Group A had a significantly higher median age than Group B (77 vs 67 years, p < 0.001), a significantly lower median BMI than Group B (21.2 vs 22.4 kg/m2, p < 0.001), and a significantly lower median preoperative albumin level than Group B (3.8 vs 4.2 g/dL, p < 0.001). There were also significant differences between Groups A and B in the sex ratio, the proportion of ECOG-PS scores, the proportion of patients who took antiplatelet or anticoagulant drugs, and the proportion of patients with underlying disorders such as hypertension, diabetes mellitus, respiratory diseases, cardiovascular/cerebrovascular diseases, or other malignant diseases. In addition, significant inter-group differences were observed with respect to the surgical approach, the type of gastrectomy, the extent of dissection, and the administration of postoperative adjuvant chemotherapy. In contrast, there were no significant differences between Groups A and B in either clinical stage or administration of preoperative chemotherapy.
Risk score and classification of groups
We performed univariate and multivariate analysis of 13 clinicopathological factors to determine whether they were significantly associated with deaths from other causes within 5 years after surgery: age (≥ 75 years), sex (male), BMI (< 22 kg/m2), ECOG-PS (≥ 1), antiplatelet or anticoagulant drugs, hypertension, diabetes mellitus, respiratory diseases, cardiovascular diseases, other malignant diseases, the level of preoperative albumin (< 3.5 g/dL), the type of gastrectomy (total gastrectomy), and the extent of dissection (D2). Multivariate analysis identified nine of these factors as significantly associated with 5-year survival based on death from other causes: age ≥ 75 years, male sex, BMI < 22 kg/m2, ECOG-PS ≥ 1, diabetes mellitus, cardiovascular /cerebrovascular diseases, other malignant diseases, preoperative albumin level < 3.5 g/dL, and total gastrectomy (Table 2).
To build a risk score for predicting death from other causes after gastrectomy, the nine factors were allocated 1 point each, and patients with total scores of 0–2 points, 3–4 points, and 5–9 points were assigned to Low-risk, Intermediate-risk, and High-risk groups, respectively. All nine of the identified risk factors were significantly different among the three risk groups (Supplementary Table 3).
Survival rates according to risk group
Figure 2 shows the overall survival curves for the three risk groups censored at 5 years after surgery. Significant differences in survival rates were detected for the Intermediate-risk group (HR 4.44, 95% CI 3.01–6.55, p < 0.001) and the High-risk group (HR 16.33, 95% CI 10.85–24.58, p < 0.001). The 1–, 3–, and 5-year survival rates were 99.3%, 98.2%, and 96.5%, respectively for the Low-risk group; 96.6%, 90.0%, and 85.3%, respectively, for the Intermediate-risk group; and 88.4%, 66.7%, and 56.5%, respectively, for the High-risk group. The survival curves for the three risk groups over the entire 10-year observation period are shown in Supplementary Fig. 1. This analysis also identified significant differences in survival rates between the three groups (Intermediate-risk: HR 3.70, 95% CI 2.75–4.99, p < 0.001; High-risk: HR 11.82, 95% CI 8.51–16.43, p < 0.001).
We next divided each of the three risk groups into two subgroups based on age ≥ 75 years and < 75 years and compared the survival curves of each risk group censored at 5 years (Fig. 3). The overall 5-year survival rate of the High-risk group was 64.7% and 54.0% for the < 75-years and ≥ 75-years groups, respectively. There were significant differences in survival rates among the three risk groups for both of the < 75-years and ≥ 75-years groups. This result indicates that the risk score is not depending simply on the age of patients.
Subgroup analyses according to the extent of gastrectomy
To determine the impact of the extent of gastrectomy on the risk of death from other causes, we performed an additional subgroup analysis comparing survival between patients who underwent total gastrectomy (total group) and the others (non-total group). The results showed that the total group had a significantly shorter overall survival time than the non-total group (HR 1.66, 95% CI 1.22–2.24, P = 0.001) (Supplementary Fig. 2).
Discussion
The goal of this study was to identify key clinicopathological risk factors and to build a composite risk score to aid in predicting patients most likely to die from other causes after curative gastrectomy. To this end, we excluded patients who died from postoperative complications during hospitalization, and those with stage IV and recurrent gastric cancer, which eliminated the influence of gastric cancer on death from other causes, such as pneumonia exacerbated by gastric cancer. In addition, we excluded patients with gastric stump cancer based on the possibility that the first gastrectomy might affect death from other causes. The cutoff for follow-up was selected as 5 years because we assumed that patients who had no recurrence would be expected to survive for at least 5 years after surgery. Finally, by excluding the patients who were followed up for < 5 years, we could directly compare patients who died from other causes within 5 years after surgery and those who survived at least 5 years after surgery.
In multivariate analysis, we identified nine factors that differed significantly between patients who survived and those who died from other causes within 5 years after surgery, and built a composite risk score based on those nine characteristics. We then performed a weighting based on odds ratio of each risk factor, and found that performance of the risk model was similar between one with and without weighting. Therefore, we decided to employ a simpler risk model that allocate one point for all parameters. Patients in the Low-, Intermediate-, and High-risk groups showed clear and significant differences in survival rates, indicating that the score may be useful for predicting death from other causes after gastrectomy. Indeed, the survival rate of the High-risk group at 5 years after surgery was only 56.6% (HR 16.33, 95% CI 10.85–24.58, p < 0.001).
How the risk score for predicting postoperative death from other causes can be applied to clinical practice should be pondered. Firstly, this score will allow us to provide objective data on postoperative risk of mortality from other causes in addition to surgical complications and possibility of recurrences of gastric cancer during preoperative explanation to the patients and family. Since some patients undergoing gastrectomy believe that long-term survival should be achieved if gastric cancer is cured, it is desirable to fully explain the risk of death from other causes particularly for patients at high risk before making a decision on whether to perform gastrectomy as the standard of care. Secondly, postoperative survival time can be estimated by the risk score for predicting death from other causes particularly in patients with stage I gastric cancer, which have high expectations for long-term cancer-free survival after curative resection. The 5-year overall survival rates were reportedly 89.6% for stage IA gastric cancer, 83.8% for stage IB, 77.3% for stage IIA, 69.1% for stage IIB, 58.7% for stage IIIA, 44.1% for stage IIIB. 30.1% for stage IIIC, and 13.4% for stage IV, respectively [17]. For patients with stage III or IV gastric cancer, treatment of gastric cancer is naturally given a priority because the risk of death from primary disease is higher than that from other causes. On the other hand, the risk score for predicting death from other causes can be useful to estimate long-term survival after surgery in patients with stage I gastric cancer, where a high probability of cure of primary disease can be expected. Thirdly, physicians can devise patient management during postoperative follow-up based on the results of the risk score for predicting death from other causes. Body weight loss is more likely to occur during the first year after gastrectomy [18]. If the patient’s condition including nutritional status severely declines, it will be difficult to recover to the baseline. Therefore, patients at high risk for postoperative death from other causes may benefit from close follow-up than recommended by the treatment guidelines, constant rehabilitation and nutritional support in parallel with treatment of comorbidities [19]. Moreover, respiratory disease was one of major causes of death within 5 years after gastrectomy, accounting for approximately 20%. It was speculated that the deteriorated swallowing functions mainly due to muscle mass loss after gastrectomy made patients susceptible to aspiration pneumonia. Respiratory rehabilitation and swallowing training may reduce the incidence of respiratory disease considering several previous reports indicated that age (75 years and older), poor preoperative respiratory functions, and total gastrectomy were associated with increased risks of postoperative pneumonia (6,7,8,9). In fact, our additional subgroup analyses also indicated that the total group had a significantly shorter overall survival time than the non-total group. We hypothesized that the long-term and negative effects of total gastrectomy on nutrition and quality of life led to an increased risk of death from other causes. Since it is impossible to conclude the effectiveness of respiratory rehabilitation and swallowing training from results of the present study, prospective clinical studies will be needed.
There are several limitations to this study. First, this was a retrospective study and 305 patients were excluded for missing data, mainly preoperative albumin levels. Second, the cause of death was unknown for about 20% of the patients who died from other causes within 5 years after surgery. Third, this study was restricted to the Japanese population. Our predictive score needs to be verified in broader populations, including Western countries. Finally, other factors that can affect death from other causes may have been excluded from our multivariate analysis.
In conclusion, we have established a risk score to predict death from other causes after gastrectomy that may be useful for the management of gastric cancer patients.
Data availability
All the data obtained and/or analyzed during the current study were available from the corresponding authors on reasonable request.
References
Asaka M, Kobayashi M, Kudo T, Akino K, Asaka Y, Fujimori K, et al. Gastric cancer deaths by age group in Japan: outlook on preventive measures for elderly adults. Cancer Sci. 2020;111(10):3845–53.
Nunobe S, Oda I, Ishikawa T, Akazawa K, Katai H, Isobel Y, et al. Surgical outcomes of elderly patients with Stage I gastric cancer from the nationwide registry of the Japanese gastric cancer association. Gastric Cancer. 2020;23(2):328–38.
Asaka M, Sugiyama T, Nobuta A, Kato M, Takeda H, Graham DY. Atrophic gastritis and intestinal metaplasia in Japan: results of a large multicenter study. Helicobacter. 2001;6(4):294–9.
Rogers C. Postgastrectomy nutrition. Nutr Clin Pract. 2011;26(2):126–36.
Zheng HL, Lu J, Zheng CH, Li P, Xie JW, Wang JB, et al. Short- and long-term outcomes in malnourished patients after laparoscopic or open radical gastrectomy. World J Surg. 2018;42(1):195–203.
Fujiya K, Kawamura T, Omae K, Makuuchi R, Irino T, Tokunaga M, et al. Impact of malnutrition after gastrectomy for gastric cancer on long-term survival. Ann Surg Oncol. 2018;25(4):974–83.
Cho H, Tsuchida K, Iwasaki K, Maezawa Y. Risk factors of post-operative pneumonia in elderly patients with gastric cancer: a retrospective cohort study. Jpn J Clin Oncol. 2021;51(7):1044–50.
Inokuchi M, Kojima K, Kato K, Sugita H, Sugihara K. Risk factors for post-operative pulmonary complications after gastrectomy for gastric cancer. Surg Infect. 2014;15(3):314–21.
Miki Y, Makuuchi R, Tokunaga M, Tanizawa Y, Bando E, Kawamura T, et al. Risk factors for postoperative pneumonia after gastrectomy for gastric cancer. Surg Today. 2016;46(5):552–6.
Liu JY, Peng CW, Yang XJ, Huang CQ, Li Y. The prognosis role of AJCC/UICC 8thedition staging system in gastric cancer a retrospective analysis. Am J Translat Res. 2018;10(1):292–303.
Japanese gastric cancer association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric cancer. 2017;20(1):1–19.
Kanda M, Kodera Y, Sakamoto J. Updated evidence on adjuvant treatments for gastric cancer. Exp Rev Gastroenterol Hepatol. 2015. https://doi.org/10.1586/17474124.2015.1094373.
Kanda M, Murotani K, Kobayashi D, Tanaka C, Yamada S, Fujii T, et al. Postoperative adjuvant chemotherapy with S-1 alters recurrence patterns and prognostic factors among patients with stage II/III gastric cancer: a propensity score matching analysis. Surgery. 2015;158(6):1573–80.
Kanda M, Kasahara Y, Shimizu D, Miwa T, Umeda S, Sawaki K, et al. Amido-bridged nucleic acid-modified antisense oligonucleotides targeting syt13 to treat peritoneal metastasis of gastric cancer. Molecular Ther-Nucle Acids. 2020;22:791–802.
Kanda M, Shimizu D, Sawaki K, Nakamura S, Umeda S, Miwa T, et al. Therapeutic monoclonal antibody targeting of neuronal pentraxin receptor to control metastasis in gastric cancer. Mol Cancer. 2020. https://doi.org/10.1186/s12943-020-01251-0.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2013;48(3):452–8.
Suzuki S, Takahashi A, Ishikawa T, Akazawa K, Katai H, Isobe Y, et al. Surgically treated gastric cancer in Japan: 2011 annual report of the national clinical database gastric cancer registry. Gastric Cancer. 2021;24(3):545–66.
Kimura Y, Nishikawa K, Kishi K, Inoue K, Matsuyama J, Akamaru Y, et al. Long-term effects of an oral elemental nutritional supplement on post-gastrectomy body weight loss in gastric cancer patients (KSES002). Ann Gastroenterol Surg. 2019;3(6):648–56.
Japanese gastric cancer association. Japanese gastric cancer treatment guidelines 2018. Gastric Cancer. 2021;24(1):1–21.
Acknowledgements
We thank Anne M. O’Rourke, PhD, from Edanz Group (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10120_2022_1354_MOESM2_ESM.tif
Supplementary file2 FIG. 2 Overall survival rates of the total study population stratified by the type of gastrectomy (total vs non-total) (TIF 6661 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ito, Y., Miwa, T., Kanda, M. et al. Risk score for predicting death from other causes after curative gastrectomy for gastric cancer. Gastric Cancer 26, 317–323 (2023). https://doi.org/10.1007/s10120-022-01354-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-022-01354-1