Abstract
Background
Peritoneal cytology has been used as a part of the cancer staging of gastric cancer patients. The primary aim of this systematic review was to evaluate the value of peritoneal cytology as part of the staging of gastric cancer and survival prediction. The second aim was to establish if positive cytology may be modified by neoadjuvant therapy, to improve prognosis.
Methods
An electronic literature search was performed using Embase, Medline, Web of Science, and Cochrane library databases up to January 2016. The logarithm of the hazard ratio (HR) with 95% confidence intervals (CI) was used as the primary summary statistic. Comparative studies were used, and the outcome measure was survival in three groups: (1) positive versus negative cytology at staging laparoscopy immediately preceding surgery; (2) effect of neoadjuvant therapy on cytology and survival; and (3) positive cytology in the absence of macroscopic peritoneal disease was compared with obvious macroscopic peritoneal disease.
Results
Pooled analysis demonstrated that positive cytology was associated with significantly reduced overall survival (HR, 3.46; 95% CI, 2.77–4.31; P < 0.0001). Interestingly, negative cytology following neoadjuvant chemotherapy was associated with significantly improved overall survival (HR, 0.42; 95% CI, 0.31–0.57; P < 0.0001). The absence of macroscopic peritoneal disease with positive cytology was associated with significantly improved overall survival (HR, 0.64; 95% CI, 0.56–0.73; P < 0.0001).
Conclusion
This study suggests that patients with initial positive cytology may have a good prognosis following neoadjuvant treatment if the cytology results change to negative after treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The main treatment of advanced nonmetastatic gastric cancer is surgical resection with perioperative chemotherapy or chemoradiotherapy [1, 2]. Efforts to prolong survival in metastatic gastric cancer have showed little improvement [1, 2]. Accurate staging of gastric cancer is crucial in selecting the appropriate treatment option, whether curative or palliative. The Japanese Gastric Cancer Association included the results of cytological examination of peritoneal lavage fluid as a key prognostic factor in their classification of gastric carcinoma [1, 3]. However, recently published guidelines suggested that cytology-positive status in the absence of other noncurative factors, that is, macroscopic disease, can be managed with D2 gastrectomy and perioperative chemotherapy [4]. Initial data of those treated with surgery alone showed poor 5-year survival; however, more recent publications have shown that the use of postoperative chemotherapy improves overall survival rates to 26%, [5, 6]. On the other hand, if the information on cytology status were available before surgery, a chemotherapy-first strategy could be taken whereby patients whose cytology status turned negative could be preferentially treated with curative surgery [7, 8].
The incidence of positive peritoneal cytology for patients with gastric cancer varies, in published reports, from 4% to 41% [9]. Peritoneal washings positive for cancer cells have been demonstrated to correlate with the extent of cancer (T1/T2, 0%; T3/T4, 10%; M+, 59%) [10] and have been considered as stage IV disease [11]. The influence of positive cytology on survival has been shown as a powerful independent predictor of survival when compared to other postoperative pathological variables such as the tumor serosal invasion or lymph node involvement [2, 6, 12, 13]. Positive cytology was shown to be the most powerful predictor of outcome, with a risk ratio of 2.7 for patients undergoing curative resection [2]. Furthermore, studies have also shown that the number and arrangement of cytology-positive cells have an effect on survival at the time of gastrectomy [10, 12].
The results of the randomized controlled trial by the apan Clinical Oncology Group (JCOG 0705) and Korea Gastric Cancer Association (KGCA01), comparing gastrectomy plus chemotherapy versus chemotherapy alone in advanced gastric cancer with a single noncurable factor, showed no advantage of resecting the primary gastric cancer in the presence of peritoneal metastasis [11]. Nevertheless, the treatment recommendations for gastric cancer in the event of positive cytology range from palliative chemotherapy to attempts at neoadjuvant therapy followed by surgical resection [4, 14].
The aim of this study was to evaluate the value of peritoneal cytology as part of the staging of gastric cancer and survival prediction. The secondary aim is to establish if positive cytology may be modified by neoadjuvant therapy to improve prognosis.
Methods
Literature search strategy
An electronic literature search was undertaken using Embase, Medline, Web of Science, and Cochrane Library databases up to January 2016. The search terms ‘gastric cancer,’ ‘laparoscopy,’ ‘peritoneal cytology,’ ‘cancer staging,’ and ‘prognosis,’ and Medical Subject Headings (MeSH) ‘stomach neoplasms,’ ‘neoplasm metastasis,’ ‘laparoscopy,’ and ‘cytology’ were used in combination with the Boolean operators AND or OR (Fig. 1). Two authors (S.J. and S.R.M.) performed the electronic search independently in January 2016. The electronic search was supplemented by a hand-search of published abstracts from meetings of the Society of Academic and Research Surgery, Digestive Disease Week, the Association of Upper Gastro-Intestinal Surgeons of Great Britain and Ireland, and the American Society of Clinical Oncology for 2005–2015. The reference lists of articles obtained were also searched to identify further relevant citations; as was the Current Controlled Trials Register (http://www.controlled-trials.com). Abstracts of the articles identified by the electronic search were scrutinized by two of the authors (S.J. and S.R.M.) to determine their suitability for inclusion in the pooled analysis. Any discordances regarding study inclusion between these two authors were settled in discussion with a third independent author (A.A.). The quality of evidence provided by each study was evaluated using the Oxford levels of evidence-based medicine scoring system (http://www.cebm.net/oxford-centre-evidence-based-medicine-levels-evidence-march-2009).
Publications were included in this review if they meet the following criteria:
-
Studies concerning patients with gastric cancer
-
Comparative studies of patients with positive and negative peritoneal cytology
-
Comparative studies evaluating the effect of neoadjuvant chemotherapy upon patients with positive cytology from gastric cancer
-
Comparative studies of patients with positive peritoneal cytology in the absence of macroscopic peritoneal disease and patients with macroscopic peritoneal disease.
Publications were excluded if they met any of the following criteria:
-
Studies published in a language other than English
-
Case reports or cohort studies including fewer than ten patients
-
Noncomparative studies or studies not concerning peritoneal cytology and gastric cancer.
In the situation in which authors from the same institution had published a primary paper and then an updated analysis with a larger patient cohort, the most recent publication was included in the analysis.
Outcome measures for meta-analysis of comparative studies
The primary outcome measure evaluated was the hazard ratio (HR) for overall survival. Three comparisons were made:
-
1.
Positive versus negative cytology at staging laparoscopy immediately preceding surgery.
-
2.
Initially positive cytology that became negative following neoadjuvant therapy was compared with positive cytology that remained positive despite neoadjuvant therapy.
-
3.
Positive cytology in the absence of macroscopic peritoneal disease was compared with obviously macroscopic peritoneal disease.
Statistical analysis
The logarithm of the hazard ratio (HR) with 95% confidence intervals (CI) was used as the primary summary statistic. To estimate HR and its variance, this was extracted from the study directly or required additional calculation depending on the method of data being presented: annual mortality rates, survival curves, number of deaths, or percentage of freedom from death [15].
Meta-analysis of data was conducted using a random effects model. Publication bias was explored graphically with funnel plots to detect asymmetry and any outliers. Interstudy heterogeneity was assessed using the chi-square statistic and the I 2 value to measure the degree of variation not attributable to chance alone: this was graded as low (I 2 < 25%), moderate (I 2 = 25–75%), or high (I 2 > 75%). The significance level was set at P < 0.05. Calculations were performed by G.M. and verified by T.A. This study was performed in line with Cochrane recommendations, following the MOOSE guidelines, using appropriate statistical software (STATA/SE12) [16].
Results
Patient demographics
The total number of patients included in this meta-analysis was 7970, with a male to female ratio of 1:1.6 (Table 1). The tumor demographics have been described for each group: negative versus positive cytology (Table 2).
Meta-analysis
Positive versus negative cytology
Pooled analysis of 21 studies [2, 3, 5, 9, 17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34] included 6499 patients in total, 1052 in the positive and 4948 in the negative cytology group at staging laparoscopy. The median follow-up period ranged from 24 to 140 months. This pooled analysis demonstrated that positive cytology was associated with a significantly reduced overall survival (HR, 3.46; 95% CI, 2.77–4.31; P < 0.0001) (Fig. 2). There was evidence of significant statistical heterogeneity for this result (I 2 = 84.1%).
Following neoadjuvant therapy: positive versus negative cytology
Pooled analysis of five studies [7, 24, 35,36,37] included 519 patients in total; 73 in the positive cytology and 139 in the negative cytology group. The median follow-up period ranged from 60 to 84 months. This pooled analysis demonstrated that negative cytology following neoadjuvant chemotherapy was associated with significantly improved overall survival (HR, 0.42; 95% CI, 0.31–0.57; P < 0.0001) (Fig. 3). There was evidence of significant statistical heterogeneity for this result (I 2 = 62.5%).
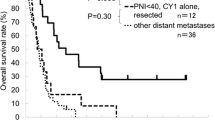
Positive cytology versus macroscopic peritoneal disease
Pooled analysis of seven studies [3, 7, 9, 17, 20, 25] included 1035 patients in total, 465 in the positive cytology and 537 in the macroscopic peritoneal disease group. The median follow-up period ranged from 36 to 120 months. This pooled analysis demonstrated that positive cytology in the absence of macroscopic peritoneal disease was associated with a significantly improved overall survival (HR, 0.64; 95% CI, 0.56–0.73; P < 0.0001) (Fig. 4). There was no evidence of significant statistical heterogeneity for this result (I 2 = 0%).
Bias exploration/sensitivity analyses
Funnel plots were created for combined and subgroup analysis for the various factors to visually assess the publication bias; these demonstrated symmetry. To determine the influence of each study’s individual dataset, we performed sensitivity analyses for the subgroups as described. A single study involved in the pooled meta-analysis was excluded each time, and the corresponding HR was not changed noticeably (data not shown).
Discussion
This meta-analysis has demonstrated negative peritoneal cytology before treatment improves survival rate when compared with positive cytology. Cytology should be considered a modifiable factor as it was found in this meta-analysis, that the change in cytology status from a positive to negative result following chemotherapy was shown to carry an improvement in overall survival. Furthermore, although positive cytology is considered stage IV disease, the prognosis and overall survival associated with positive cytology versus macroscopic peritoneal metastasis are not equivalent [31]. Fujiwara et al. have shown that the change in cytology status to negative following receiving neo-adjuvant intraperitoneal chemotherapy and systemic chemotherapy improved prognosis [37]. It is worth noting that although Lorenzen et al. have also shown that the change in cytological status to negative following chemotherapy led to improved prognosis, almost 25% with negative cytology became positive following chemotherapy, thus worsening their prognosis and outcome [36]. The prediction of response of patients to neoadjuvant therapy as assessed by cytology remains a challenging area for future research to provide patient- and tumor-targeted therapy.
Regarding peritoneal disease, this meta-analysis has shown that positive cytology alone carries better survival compared with macroscopic peritoneal dissemination. Although survival with no treatment can be similar between these two groups, the use of neo-adjuvant chemotherapy was shown to improve the 3-year overall survival from 0% in gross peritoneal disease to 12% in positive cytology with no overt peritoneal disease [9]. Therefore, the concept that positive cytology is a potentially modifiable factor is further supported. Interestingly, Miyashiro et al. also studied the number of cancer cells detected in cytology studies versus peritoneal metastasis and found that when a higher number of cells was detected, survival was similar to those with peritoneal metastasis [3]. There was insufficient evidence available to define a threshold of positive cancer cells from cytology that changed survival from this review, which remains an important area for future research.
There are a number of limitations to this systematic review and meta-analysis that need to be acknowledged. First, the lack of randomized control trials (RCTs) that met the inclusion criteria is therefore reducing the power of the analyses. Second, only studies in the English-language literature were included, so it is possible that relevant studies in other languages will be identified in the future. Also, patient demographics and co-morbidities were not reported in all the included studies.
In conclusion, the results of this meta-analysis support the importance of peritoneal cytology results in the assessment of gastric cancer patients. We have shown that negative cytology and the change in cytological status from positive to negative improve survival in gastric cancer. This knowledge justifies the notion to reconsider the presence of positive peritoneal cytology as an absolute indication for palliative intent of treatment without further consideration to changing status following chemotherapy (Fig. 5). The change of initial positive cytology to negative subsequent to treatment should be the subject of a prospective large-scale multicenter study that examines long-term survival benefits.
References
Japanese classification of gastric carcinoma. Japanese gastric cancer, 2nd edn. Gastric Cancer. 1998;1:10–24.
Bentrem D, Wilton A, Mazumdar M, et al. The value of peritoneal cytology as a preoperative predictor in patients with gastric carcinoma undergoing a curative resection. Ann Surg Oncol. 2005;12:347–53.
Miyashiro I, Takachi K, Doki Y, et al. When is curative gastrectomy justified for gastric cancer with positive peritoneal lavage cytology but negative macroscopic peritoneal implant? World J Surg. 2005;29:1131–4.
Association Japanese Gastric Cancer. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017;20:1–19.
Kodera Y, Ito S, Mochizuki Y, et al. Long-term follow up of patients who were positive for peritoneal lavage cytology: final report from the CCOG0301 study. Gastric Cancer. 2012;15:335–7.
Bando E, Makuuchi R, Miki Y, et al. Clinical significance of intraoperative peritoneal cytology in gastric carcinoma-analysis of 3124 patients. 10th International Gastric Cancer Congress 2013; abstract P27–5.
Mezhir JJ, Shah MA, Jacks LM, et al. Positive peritoneal cytology in patients with gastric cancer: natural history and outcome of 291 patients. Indian J Surg Oncol. 2011;2:16–23.
Okabe H, Hata H, Ueda S, et al. A phase II study of neoadjuvant chemotherapy with S-1 and cisplatin for stage III gastric cancer: KUGC03. J Surg Oncol. 2016;113:36–41.
Badgwell B, Cormier JN, Krishnan S, et al. Does neoadjuvant treatment for gastric cancer patients with positive peritoneal cytology at staging laparoscopy improve survival? Ann Surg Oncol. 2008;15:2684–91.
Conlon KC. Staging laparoscopy for gastric cancer. Ann Ital Chir. 2001;72:33–7.
Fujitani K, Yang HK, Kurokawa Y, et al. Randomized controlled trial comparing gastrectomy plus chemotherapy with chemotherapy alone in advanced gastric cancer with a single non-curable factor: Japan Clinical Oncology Group Study JCOG 0705 and Korea Gastric Cancer Association Study KGCA01. Jpn J Clin Oncol. 2008;38:504–6.
Itsuka Y, Kaneshima S, Tanida O, et al. Intraperitoneal free cancer cells and their viability in gastric cancer. Cancer (Phila). 1979;44:1476–80.
Bonenkamp JJ, Songun I, Hermans J, et al. Prognostic value of positive cytology findings from abdominal washings in patients with gastric cancer. Br J Surg. 1996;83:672–4.
Sakuramoto S, Sasako M, Yamaguchi T, et al. Adjuvant chemotherapy for gastric cancer with S-1, an oral flu-oropyrimidine. N Engl J Med. 2007;357:1810–20.
Parmar MK, Torri V, Stewart L. Extracting summary statistics to perform meta-analyses of the published literature for survival endpoints. Stat Med. 1998;17:2815–34.
Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–12.
Lee SD, Ryu KW, Eom BW, et al. Prognostic significance of peritoneal washing cytology in patients with gastric cancer. Br J Surg. 2012;99:397–403.
La Torre M, Ferri M, Giovagnoli MR, et al. Peritoneal wash cytology in gastric carcinoma. Prognostic significance and therapeutic consequences. Eur J Surg Oncol. 2010;36:982–6.
Ribeiro U Jr, Safatle-Ribeiro AV, Zilberstein B, et al. Does the intraoperative peritoneal lavage cytology add prognostic information in patients with potentially curative gastric resection? J Gastrointest Surg. 2006;10:170–6.
Rosenberg R, Nekarda H, Bauer P, et al. Free peritoneal tumour cells are an independent prognostic factor in curatively resected stage IB gastric carcinoma. Br J Surg. 2006;93:325–31.
Brito AM, Sarmento BJ, Mota ED, et al. Prognostic role of positive peritoneal cytology in patients with resectable gastric cancer. Rev Col Bras Cir. 2013;40:121–6.
Chuwa EW, Khin LW, Chan WH, et al. Prognostic significance of peritoneal lavage cytology in gastric cancer in Singapore. Gastric Cancer. 2005;8:228–37.
Emoto S, Kitayama J, Ishigami H, et al. Clinical significance of cytological status of peritoneal lavage fluid during intraperitoneal chemotherapy for gastric cancer with overt peritoneal dissemination. Ann Surg Oncol. 2015;22:780–6.
Euanorasetr C, Lertsithichai P. Prognostic significance of peritoneal washing cytology in Thai patients with gastric adenocarcinoma undergoing curative D2 gastrectomy. Gastric Cancer. 2007;10:18–23.
Fukagawa T, Katai H, Saka M, et al. Significance of lavage cytology in advanced gastric cancer patients. World J Surg. 2010;34:563–8.
Jiang CG, Xu Y, Wang ZN, et al. Clinicopathological analysis and prognostic significance of peritoneal cytology in Chinese patients with advanced gastric cancer. ANZ J Surg. 2011;81:608–13.
Kang KK, Hur H, Byun CS, et al. Conventional cytology is not beneficial for predicting peritoneal recurrence after curative surgery for gastric cancer: results of a prospective clinical study. J Gastric Cancer. 2014;14:23–31.
Katsuragi K, Yashiro M, Sawada T, et al. Prognostic impact of PCR-based identification of isolated tumour cells in the peritoneal lavage fluid of gastric cancer patients who underwent a curative R0 resection. Br J Cancer. 2007;20(97):550–6.
Makino T, Fujiwara Y, Takiguchi S, et al. The utility of pre-operative peritoneal lavage examination in serosa-invading gastric cancer patients. Surgery (St. Louis). 2010;148:96–102.
de Manzoni G, Verlato G, Di Leo A, et al. Peritoneal cytology does not increase the prognostic information provided by TNM in gastric cancer. World J Surg. 2006;30:579–84.
Nakagawa S, Nashimoto A, Yabusaki H. Role of staging laparoscopy with peritoneal lavage cytology in the treatment of locally advanced gastric cancer. Gastric Cancer. 2007;10:29–34.
Noda S, Yashiro M, Toyokawa T, et al. Borrmann’s macroscopic criteria and p-Smad2 expression are useful predictive prognostic markers for cytology-positive gastric cancer patients without overt peritoneal metastasis. Ann Surg Oncol. 2011;18:3718–25.
Wong J, Kelly KJ, Mittra A, et al. RT-PCR increases detection of submicroscopic peritoneal metastases in gastric cancer and has prognostic significance. J Gastrointest Surg. 2012;16:889–96.
Shimizu H, Imamura H, Ohta K, et al. Usefulness of staging laparoscopy for advanced gastric cancer. Surg Today. 2010;40:119–24.
Aizawa M, Nashimoto A, Yabusaki H, et al. The clinical significance of potentially curative resection for gastric cancer following the clearance of free cancer cells in the peritoneal cavity by induction chemotherapy. Surg Today. 2015;45:611–7.
Lorenzen S, Panzram B, Rosenberg R, et al. Prognostic significance of free peritoneal tumor cells in the peritoneal cavity before and after neoadjuvant chemotherapy in patients with gastric carcinoma undergoing potentially curative resection. Ann Surg Oncol. 2010;17:2733–9.
Fujiwara Y, Takiguchi S, Nakajima K, et al. Neoadjuvant intraperitoneal and systemic chemotherapy for gastric cancer patients with peritoneal dissemination. Ann Surg Oncol. 2011;18:3726–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No funding sources were used in the preparation of this manuscript, and the authors have no conflicts of interest to declare.
Ethical approval
No ethical approval or informed consent statement was required for this review article.
Sources of funding
Sheraz R. Markar is supported by the National Institute for Health Research (NIHR). The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Jamel, S., Markar, S.R., Malietzis, G. et al. Prognostic significance of peritoneal lavage cytology in staging gastric cancer: systematic review and meta-analysis. Gastric Cancer 21, 10–18 (2018). https://doi.org/10.1007/s10120-017-0749-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-017-0749-y