Abstract
Background
A randomized phase III study of Japanese patients with advanced gastric cancer, the G-SOX trial, revealed that S-1 and oxaliplatin (SOX) combination therapy was noninferior to S-1 and cisplatin (CS) combination therapy. However, it is unclear whether the efficacy and safety in elderly patients were different between the two regimens.
Methods
A total of 685 patients registered in the G-SOX trial were classified as elderly (70 years or older) or not elderly (younger than 70 years), and 663 patients (SOX therapy, elderly 113 of 333 patients, 34 %; CS therapy, elderly 99 of 330 patients, 30 %) and 673 patients (SOX therapy, elderly 114 of 338 patients, 34 %; CS therapy, elderly 101 of 335 patients, 30 %) were analyzed for efficacy and safety, respectively. Treatment delivery of SOX was also compared between elderly and nonelderly groups.
Results
No differences in efficacy were identified between the elderly and nonelderly groups for either regimen. In the elderly groups, SOX therapy showed better trends in progression-free survival (hazard ratio 0.805, 95 % confidence interval 0.588–1.102) and overall survival (hazard ratio 0.857, 95 % confidence interval 0.629–1.167) compared with CS therapy, although there were no significant differences. Grade 3 or worse adverse events were less frequent in the elderly group receiving SOX than in the elderly group receiving CS except for the low incidence of sensory neuropathy (5.3 % vs 0 %), neutropenia (25.4 % vs 42.6 %), anemia (21.1 % vs 42.6 %), febrile neutropenia (1.8 % vs 10.9 %), increased creatinine level (0.9 % vs 3.0 %), and hyponatremia (7.9 % vs 18.8 %).
Conclusions
SOX is an effective and feasible therapy in both nonelderly and elderly patients with advanced gastric cancer. In elderly patients, SOX demonstrated favorable efficacy and safety compared with CS.
Similar content being viewed by others
Introduction
Gastric cancer has been associated with high incidences and mortality rates worldwide, particularly in eastern Asia [1]. In Japan, the mortality rate for gastric cancer has shown a decreasing trend. However, the mortality rate among patients aged 70 years or older has increased, accounting for 70 % or more of the total number of gastric cancer deaths [2, 3], because this population has been increasing over the past several decades [4].
To date, no standard treatment for elderly patients with gastric cancer has been established. In Japan, a combination therapy of orally administered fluoropyrimidine S-1 and cisplatin (CS) has been regarded as the standard treatment for advanced gastric cancer (AGC) on the basis of results from a randomized phase III study comparing CS with S-1 alone for first-line treatment of AGC [5, 6]. The proportion of elderly patients (70 years or older) included in that trial was only 17 % (50 patients), and the survival benefit of CS appeared slightly decreased in the elderly subgroup [hazard ratio (HR) 0.95]. This might be related to susceptibility to adverse effects of cisplatin in elderly patients. In a German phase III study comparing fluorouracil and leucovorin plus oxaliplatin (FLO) with fluorouracil and leucovorin plus cisplatin (FLP), superior efficacy of FLO over FLP was observed in a subgroup of patients older than 65 years, and severe adverse events and early treatment discontinuation were less frequent with FLO [7]. These reports suggest that oxaliplatin may be more suitable than cisplatin for elderly patients when a platinum combination treatment is used for AGC.
We previously reported a randomized phase III study (the G-SOX trial) that compared S-1 and oxaliplatin (SOX) combination therapy with CS therapy [8]. This study demonstrated noninferiority of SOX to CS in both progression-free survival (PFS) and overall survival (OS). No upper age limit was set as an eligibility criterion for inclusion in the G-SOX trial, and more than 30 % of patients enrolled were 70 years or older in each treatment group. Our preliminary analysis of the G-SOX trial revealed a trend that adverse events were more frequently observed in patients aged 70 years or older than in patients younger than 70 years. In the past analyses for Japanese patients, the definition of elderly patients has often been patients aged 70 years or older [9, 10]. For these reasons, we defined patients aged 70 years or older as elderly patients in the present exploratory study. There is no comparative analysis of SOX therapy and CS therapy in elderly patients with AGC. In the present exploratory study, we aimed to evaluate the efficacy and safety of the SOX and CS treatments in elderly patients with AGC, using the G-SOX trial data.
Patients and methods
Patients
The G-SOX trial was a randomized, open-label, phase III study that compared the efficacy and safety of the SOX and CS regimens in patients with curatively unresectable, advanced or recurrent gastric cancer who had never received chemotherapy or radiotherapy. From January 2010 to October 2011, 685 patients were randomized, and the SOX regimen was confirmed to be noninferior to the CS regimen. In the SOX regimen, S-1 was given orally twice daily for the first 2 weeks of a 3-week cycle. The dosage was 80 mg/day for body surface area (BSA) less than 1.25 m2, 100 mg/day for BSA ranging from 1.25 m2 to less than 1.5 m2, and 120 mg/day for BSA of 1.5 m2 or greater. Oxaliplatin at 100 mg/m2 was infused for 2 h intravenously on day 1 of each cycle. In the CS regimen, S-1 was given in the same way for the first 3 weeks of a 5-week cycle. Cisplatin was administered at 60 mg/m2 as an intravenous infusion with adequate hydration on day 8 of each cycle.
In this subgroup analysis, individuals aged 70 years old or older were defined as elderly patients and those younger than 70 years were defined as nonelderly patients. Safety was analyzed in the safety analysis set, which was a subset of enrolled patients who received at least one dose of oxaliplatin, cisplatin, or S-1 and had no major violations against good clinical practice. Efficacy was analyzed in the full analysis set, which was a subset of patients who met the main inclusion criteria and none of the exclusion criteria in the safety analysis set . The proportions of elderly patients were 33.9 % (113 of 333 patients) for SOX therapy and 30.0 % (99 of 330 patients) for CS therapy in the full analysis set, and 33.7 % (114 of 338 patients) for SOX therapy and 30.1 % (101 of 335 patients) for CS therapy in the safety analysis set.
Statistical analysis
The median OS, PFS, and time to treatment failure (TTF) with each 95 % confidence interval (CI) for the elderly and nonelderly groups were estimated by the Kaplan–Meier method. Differences in therapeutic efficacy between SOX and CS were tested for each age group by means of the log-rank test. The Cox proportional hazards model was used to estimate HRs of SOX therapy compared with CS therapy with 95 % CIs. Interactions between the age groups and treatments were also evaluated.
Patient baseline characteristics and incidences of adverse events (grade 3 or greater) in each age group were compared between the SOX and CS regimens by Fisher’s exact test. Adverse events were assessed in accordance with the Common Terminology Criteria for Adverse Events version 3.0. Furthermore, treatment delivery was evaluated for each age group in both treatment groups.
Statistical analyses were performed with SAS version 9.3 (SAS Institute, Cary, NC, USA).
Results
Patient characteristics
Baseline characteristics of all patients who were registered in the G-SOX trial for each age group are shown in Table 1. They were well balanced between the treatment groups in both age groups. Diffuse-type histologic appearance and peritoneal metastasis were more frequently seen in the nonelderly groups than in the elderly groups for both treatments, whereas liver metastasis was more frequent in the elderly groups than in the nonelderly groups for both treatments, although there were no statistical differences.
Efficacy
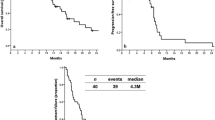
In the elderly groups, the median OS was 17.5 months for SOX therapy and 13.5 months for CS therapy (HR 0.857, 95 % CI 0.629–1.167; P = 0.325) (Fig. 1a), the median PFS was 5.7 months for SOX therapy and 5.5 months for CS therapy (HR 0.805, 95 % CI 0.588–1.102; P = 0.174) (Fig. 1b), and the median TTF was 5.5 months for SOX therapy and 4.3 months for CS therapy (HR 0.683, 95 % CI 0.515–0.907; P = 0.008) (Fig. 1c). In the nonelderly groups, the median OS was 13.3 months for SOX therapy and 13.1 months for CS therapy (HR 0.984, 95 % CI 0.800–1.209; P = 0.877), the median PFS was 4.4 months for SOX therapy and 5.3 months for CS therapy (HR 1.019, 95 % CI 0.827–1.256; P = 0.862), and the median TTF was 4.2 months for SOX therapy and 4.2 months for CS therapy (HR 0.890, 95 % CI 0.735–1.079; P = 0.234). No clear differences in efficacy were identified between the elderly and nonelderly groups for either treatment. No significant interactions between the therapeutic effects and the age groups were demonstrated for OS (P = 0.451) and PFS (P = 0.254). A weak interaction of the age groups with the treatment regimens was suggested for TTF (P = 0.141).
Safety
Common grade 3 or worse adverse events are shown in Table 2, and events of all grades are shown in Table S1. For both treatments, almost of all the adverse events occurred more frequently in the elderly groups than in the nonelderly groups. Grade 3 or worse leukopenia (8.8 % vs 26.7 %), neutropenia (25.4 % vs 42.6 %), anemia (21.1 % vs 42.6 %), febrile neutropenia (1.8 % vs 10.9 %), increased creatinine level (0.9 % vs 3.0 %), and hyponatremia (7.9 % vs 18.8 %) were less frequent in the SOX elderly group than in the CS elderly group. Among nonelderly patients, grade 3 or worse leukopenia (1.8 % vs 16.2 %), neutropenia (16.5 % vs 41.5 %), anemia (12.1 % vs 28.2 %), febrile neutropenia (0.4 % vs 5.1 %), increased creatinine level (0 % vs 1.3 %), and hyponatremia (2.7 % vs 11.1 %) were less frequent in the SOX group than in the CS group. Conversely, sensory neuropathy developed more frequently in the SOX group than in the CS group (5.3 % vs 0 % in the elderly group, 4.5 % vs 0 % in the nonelderly group). Grade 3 or worse febrile neutropenia was seen in the SOX elderly group in two of 71 patients (2.8 %) with a creatinine clearance rate (Ccr) of less than 70 ml/min and in none of 43 patients (0 %) with Ccr ≥70 ml/min, and in the CS elderly group in eight of 55 patients (14.5 %) with Ccr < 70 ml/min and in three of 46 patients (6.5 %) with Ccr ≥70 ml/min. The corresponding results in the SOX nonelderly group were one of 42 patients (2.4 %) with Ccr < 70 ml/min and none of 182 patients (0 %) with Ccr ≥70 ml/min, and in the CS nonelderly group were four of 56 patients (7.1 %) with Ccr < 70 ml/min and eight of 178 patients (4.5 %) with Ccr ≥70 ml/min.
Treatment discontinuations due to adverse events were observed in five of 114 patients (4.4 %) in the SOX elderly group, 14 of 101 patients (13.9 %) in the CS elderly group, five of 224 patients (2.2 %) in the SOX nonelderly group, and 14 of 234 patients (6.0 %) in the CS nonelderly group.
Treatment cycles and dose intensity
The median number of cycles of combination therapy and S-1 therapy were 7.0 [interquartile range (IQR) 5.0–10.0] and 7.5 (IQR 5.0–11.0), respectively, in the SOX elderly group, 6.0 (IQR 4.0–9.0) and 6.0 (IQR 4.0–10.0), respectively, in the SOX nonelderly group, 3.0 (IQR 2.0–6.0) and 4.0 (IQR 2.0–6.0), respectively, in the CS elderly group, and 4.0 (IQR 2.0–6.0) and 5.0 (IQR 3.0–7.0), respectively, in the CS nonelderly group.
The median relative dose intensity of each drug in both age groups is shown in Table 3. The median relative dose intensities of all drugs in the SOX and CS elderly groups were lower than those in the nonelderly groups. The total dose of S-1 and cisplatin in the CS elderly group was lower than that in the CS nonelderly group, and the total dose of S-1 and oxaliplatin in the SOX elderly group was higher than that in the SOX nonelderly group.
The reason for dose modification for the SOX regimen
The major reasons for dose reduction of SOX specified in the protocol were thrombocytopenia [platelet count 75,000/mm3 or greater not met by day 29 (17.5 and 14.3 % in the elderly and nonelderly groups, respectively], diarrhea of grade 3 or worse (5.3 and 3.6 %, respectively), and sensory neuropathy of grade 2 (12.3 and 11.6 %, respectively). The frequency of dose reduction on the basis of the investigator’s judgment was 36.0 and 18.3 % in the elderly and nonelderly groups, respectively (Table 4). The main reason for dose reduction per treatment cycle is shown in Fig. 2. In both age groups, dose reductions on the basis of the investigator’s judgment were frequently observed in the earlier treatment cycles. On the other hand, the frequency of dose reductions because of thrombocytopenia and sensory neuropathy increased in the later treatment cycles.
Discussion
In this study, all HRs of OS, PFS, and TTF between SOX and CS therapy were less than 1.0 in the elderly patients, suggesting a benefit of SOX over CS, although there were no statistically significant interactions between the treatment effects and age groups. The previous multivariate analysis in the G-SOX trial showed that Eastern Cooperative Oncology Group performance status (1, 2), unresectable disease, diffuse-type histologic appearance, and larger sum of tumor diameter correlated with poor prognosis [8]. No imbalance of patient baseline characteristics, including these factors, between the SOX and CS treatments was observed in the elderly groups. Although no clear differences in PFS and OS were observed between the elderly and nonelderly patients for either study regimen, both efficacy parameters appeared slightly better in the elderly patients than in the nonelderly patients. This might be partially explained by the favorable patient background of intestinal-type histologic appearance, good performance status, and more predominant recurrent status in the elderly patients in this study or another potential bias, such as selection bias. From the efficacy viewpoint, these results indicate that SOX treatment could be an option for elderly patients.
The major concern with chemotherapy in elderly patients is safety. Indeed, most adverse events observed in this study were worse in the elderly patients than in the nonelderly patients, probably owing to the low reserve of organ functions, such as bone marrow, cardiac, and renal functions, as often previously reported. However, both regimens were tolerable in the elderly groups. Grade 3 or worse adverse events were apparently less frequent in the elderly patients treated with SOX than in those treated with CS, except for sensory neuropathy. The incidence of grade 3 sensory neuropathy in the SOX elderly patients was only 5.3 %, and it was commonly reversible with treatment interruption and was not life threatening. Hematologic adverse events were noted in the CS elderly patients, and febrile neutropenia was observed in approximately 11 % of them. Careful attention should be paid especially to the adverse events in CS elderly patients. In addition, CS treatment requires a large amount of hydration to prevent renal toxicity of cisplatin. Oxaliplatin administration does not need hydration, and in this point, SOX with its lesser treatment burden is more convenient than CS. Gastrointestinal adverse effects of both SOX and CS in the elderly groups were similar to those in the nonelderly groups. From these results, SOX treatment was considered safer and more feasible than CS treatment for elderly patients with AGC. Furthermore, treatment discontinuation because of adverse events occurred more frequently in CS patients than in SOX patients (13.9 % vs 4.4 %) among elderly patients. This was probably because elderly patients were more susceptible to the higher toxicity of the CS regimen. This suggests that many patients treated with the CS regimen could not obtain a possible benefit from chemotherapy, which is similar to the findings reported in the German trial [7].
Although the incidence of severe adverse events increased in the elderly patients compared with the nonelderly patients for both SOX therapy and CS therapy, similar survival was demonstrated between both age groups. Among patients who received SOX, dose reductions were performed more frequently in elderly patients and resulted in a lower relative dose intensity compared with that in nonelderly patients, but these elderly patients were able to continue the treatment for as long as nonelderly patients, and the total dose administrated in the SOX elderly group reached almost the same amount as that in the nonelderly group. The proportion of patients with dose reductions of SOX specified in the protocol was similar between the elderly and nonelderly groups. On the other hand, the proportion of patients with dose reduction on the basis of the investigator’s judgment, especially in the early treatment cycles, was greater in the elderly group than in the nonelderly group. In most cases the investigator’s decision to reduce the dose was based on multiple adverse events of grade less than 3. This suggests that appropriate dose modifications by physicians are the key to treating elderly patients with SOX safely without compromising its efficacy.
In our study, we defined individuals aged 70 years or older as elderly patients despite heterogeneity of the elderly cancer population. Because of the heterogeneity of this population, it might be difficult to define “elderly” only in terms of a chronological age. Comprehensive geriatric assessment (CGA) is a well-established approach for elderly cancer patients and is defined as a multidimensional and interdisciplinary diagnostic process focused on determining a frail elderly person’s medical, psychological, and functional capabilities in order to develop a coordinated and integrated plan for treatment and long-term follow-up [11]. In 2005, the International Society of Geriatric Oncology recommended the use of CGA in elderly cancer patients [12]. Because CGA is a resource-consuming approach, the International Society of Geriatric Oncology also suggested the use of screening tools to identify elderly patients who require an evaluation by CGA [13]. In elderly cancer patients, the presence of multiple comorbidities often leads to death as a result of non-cancer-related diseases. OS or PFS might not always be suitable end points to access elderly patients. In future trials, integration of a CGA form will be recommended [14].
In conclusion, the present study showed that SOX is an effective and feasible therapy in nonelderly patients (younger than 70 years) and even in elderly patients (70 years or older) with AGC. In elderly patients, SOX demonstrated favorable efficacy and safety compared with CS.
References
Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012 v1.0. Cancer incidence mortality worldwide. IARC CancerBase. 2012. Available via http://globocan.iarc.fr/default.aspx. Accessed 23 Feb 2015.
Ministry of Health, Labour and Welfare. Vital statistics Japan. 2014. Available via http://ganjoho.jp/reg_stat/statistics/dl/index.html. Accessed 6 Feb 2015.
Matsuda A, Matsuda T, Shibata A, Katanoda K, Sobue T, Nishimoto H. Cancer incidence and incidence rates in Japan in 2008: a study of 25 population-based cancer registries for the monitoring of cancer incidence in Japan (MCIJ) project. Jpn J Clin Oncol. 2013;44:388–96.
National Institute of Population and Social Security Research. Population projections for Japan (January 2012 estimates). 2012. Available via http://www.ipss.go.jp/syoushika/tohkei/newest04/sh2401top.html. Accessed 6 Feb 2015.
Koizumi W, Narahara H, Hara T, Takagane A, Akiya T, Takagi M, et al. S-1 plus cisplatin vs. S-1 alone for first-line treatment of advanced gastric cancer (SPIRITS trial): a phase III trial. Lancet Oncol. 2008;9:215–21.
Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines (ver. 4). Tokyo: Kanehara Publication. 2014.
Al-Batran SE, Hartmann JT, Probst S, Schmalenberg H, Hollerbach S, Hofheinz R, et al. Phase III trial in metastatic gastroesophageal adenocarcinoma with fluorouracil, leucovorin plus either oxaliplatin or cisplatin: a study of the Arbeitsgemeinschaft Internistische Onkologie. J Clin Oncol. 2008;26:1435–42.
Yamada Y, Higuchi K, Nishikawa K, Gotoh M, Fuse N, Sugimoto N, et al. Phase III study comparing oxaliplatin plus S-1 with cisplatin plus S-1 in chemotherapy-naïve patients with advanced gastric cancer. Ann Oncol. 2015;26:141–8.
Tsushima T, Hironaka S, Boku N, Machida N, Yamazaki K, Yasui H, et al. Comparison of safety and efficacy of S-1 monotherapy and S-1 plus cisplatin therapy in elderly patients with advanced gastric cancer. Int J Clin Oncol. 2013;18:10–6.
Terazawa T, Iwasa S, Takashima A, Nishitani H, Honma Y, Kato K, et al. Impact of adding cisplatin to S-1 in elderly patients with advanced gastric cancer. J Cancer Res Clin Oncol. 2013;139:2111–6.
Rubenstein LZ, Stuck AE, Siu AL, Wieland D. Impacts of geriatric evaluation and management programs on defined outcomes: overview of the evidence. J Am Geriatr Soc. 1991;39:8S–16S.
Extermann M, Aapro M, Bernabei R, Cohen HJ, Droz JP, Lichtman S, et al. Use of comprehensive geriatric assessment in older cancer patients: recommendations from the task force on CGA of the International Society of Geriatric Oncology (SIOG). Crit Rev Oncol Hematol. 2005;55:241–52.
Decoster L, Van Puyvelde K, Mohile S, Wedding U, Basso U, Colloca G, et al. Screening tools for multidimensional health problems warranting a geriatric assessment in older cancer patients: an update on SIOG recommendations. Ann Oncol. 2015;26:288–300.
Wildiers H, Mauer M, Pallis A, Hurria A, Mohile SG, Luciani A, et al. End points and trial design in geriatric oncology research: a joint European Organisation for Research and Treatment of Cancer–Alliance for Clinical Trials in Oncology–International Society of Geriatric Oncology position article. J Clin Oncol. 2013;31:3711–8.
Acknowledgments
This study was conducted as supportive analysis for the G-SOX study and was supported by Yakult Honsha. We thank all the patients, clinicians, and support staff who participated in this study. We also thank Keigo Makino and Hiroki Kageyama for their helpful advice.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Hideaki Bando received research funding from AstraZeneca. Yasuhide Yamada received honoraria from Yakult Honsha, Chugai Pharmaceutical, and Taiho Pharmaceutical. Naotoshi Sugimoto received research funding from Yakult Honsha and Taiho Pharmaceutical. Akihito Tsuji received honoraria from Yakult Honsha and Taiho Pharmaceutical. Chikuma Hamada and Ichinosuke Hyodo received advisory fees from Yakult Honsha and Daiichi Sankyo. Kenji Amagai received research funding from Taiho Pharmaceutical. The other authors declare that they have no conflict of interest.
Human rights statement and informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964 and later versions. Informed consent or substitute for it was obtained from all patients for their being included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bando, H., Yamada, Y., Tanabe, S. et al. Efficacy and safety of S-1 and oxaliplatin combination therapy in elderly patients with advanced gastric cancer. Gastric Cancer 19, 919–926 (2016). https://doi.org/10.1007/s10120-015-0549-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-015-0549-1