Abstract
Background
Human epidermal growth factor (HER) 2 positivity and its association with clinicopathological factors remain unclear in Japanese gastric cancer (GC) patients. We performed a prospective, multicenter, observational cohort study to evaluate HER2 protein expression and gene amplification in Japanese metastatic and recurrent GC patients, and explored its correlations with clinicopathological features.
Methods
HER2 protein expression and gene amplification were centrally assessed in formalin-fixed, paraffin-embedded GC tissue by immunohistochemistry (IHC) and fluorescence in situ hybridization (FISH). Patient information was collected, and associations between clinicopathological factors and HER2 positivity (IHC score 3+ and/or FISH positive) and low HER2 expression (IHC score 0/FISH positive or IHC score 1+/FISH positive) were examined.
Results
From September 2011 to June 2012, 1461 patients were registered across 157 sites, and the HER2 status of 1427 patients was evaluated. The rate of HER2 positivity was 21.2 %, whereas the rate of high HER2 expression (IHC score 2+/FISH positive or IHC score 3+) was 15.6 % and that of low HER2 expression was 7.0 %. Multiple logistic regression analysis identified intestinal type, absence of peritoneal metastasis, and hepatic metastasis as significant independent factors related to HER2 positivity. The intestinal type was confirmed to be the GC subtype predominantly associated with lower HER2 expression. Sampling conditions including number of biopsy samples, formalin concentration, and formalin-fixation time did not significantly affect HER2 positivity.
Conclusions
HER2 expression in Japanese patients was comparable to that in other populations examined. Intestinal type was an independent factor related to HER2 positivity and low HER2 expression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trastuzumab (Herceptin) is a monoclonal antibody that specifically targets human epidermal growth factor receptor 2 (HER2), a receptor associated with gastric cancer (GC) tumorigenesis, by directly binding its extracellular domain [1]. The Trastuzumab for GAstric Cancer (ToGA) study, an open-label, international, multicenter, phase III, randomized controlled trial, examined the clinical efficacy and safety of trastuzumab combined with standard chemotherapy (capecitabine or intravenously administered 5-fluorouracil and cisplatin) for first-line treatment of HER2-overexpressing advanced gastric or gastroesophageal junction cancers. Addition of trastuzumab therapy to chemotherapy improved median survival (13.8 months) compared with chemotherapy alone (11.1 months) (P = 0.0046), and showed significant improvements in time to progression and progression-free survival in the trastuzumab-treated group, with a comparable toxicity profile [2]. As a result, trastuzumab therapy plus chemotherapy has become the standard treatment for HER2-positive advanced GC patients, as determined by immunohistochemistry (IHC) and/or fluorescence in situ hybridization (FISH). In Japan and the USA, trastuzumab is approved for patients with metastatic GC whose tumors are HER2 positive, as defined by a positive FISH result or an IHC score of 3+. In the European Union, however, trastuzumab is recommended only for individuals whose tumors have high HER2 protein expression, as defined by an IHC score of 2+/positive FISH result or an IHC score of 3+ based on the subset analysis of the ToGA study. HER2 evaluation has therefore become an important approach for predicting clinical efficacy of trastuzumab. The variation in the HER2-positivity rate between countries possibly reflects the unstandardized testing modality and other country-specific factors; it was identified as 27 % in Japanese patients in the ToGA study [3, 4], which was higher than that identified in previous studies in Japan [5–7].
In the ToGA study, the strong effect of trastuzumab was evident in patients with higher HER2 protein expression (IHC score 2+/FISH positive or IHC score 3+), whereas the efficacy was unclear in patients with low HER2 expression (IHC score 0/FISH positive or IHC score 1+/FISH positive). These results were obtained via a subgroup analysis, and may be affected by the smaller number of patients with low HER2 expression than higher HER2 protein expression. Thus, it is premature to conclude that addition of trastuzumab therapy to chemotherapy is not beneficial in patients with low HER2 expression. Additionally, little has been reported about the clinicopathological features of patients with low HER2 expression [8–10].
In unresectable cases, tumor behavior before treatment is evaluated by biopsy specimens. However, because GC is considered a mixture of heterogeneous tumor types, small biopsy specimens may not reflect its overall behavior, and few studies have focused on HER2-positivity concordance between diagnostic biopsy specimens and surgical specimens [11, 12]. Because of tumor heterogeneity, the accuracy of HER2 testing can be affected by the site of the examined HER2-stained cells; thus, gastric biopsies could yield false-negative results [13].
We performed a prospective, multicenter, observational cohort study (JFMC44-1101) to evaluate HER2 expression and gene amplification in consecutively registered Japanese patients with metastatic (excluding curatively resected cases) or recurrent GC, and explored the clinicopathological features in relation to HER2 positivity (IHC score 3+ and/or FISH positive) or low HER2 expression (IHC score 0/FISH positive or IHC score 1+/FISH positive). Furthermore, we evaluated the relationship between HER2 protein expression/gene amplification and sampling conditions to ascertain whether HER2 positivity in GC patients can be accurately determined from routinely prepared formalin-fixed, paraffin-embedded tissues.
Methods
Patients
JFMC44-1101 is a multicenter, observational cohort study to evaluate HER2 protein expression and gene amplification in consecutively registered Japanese patients with metastatic (excluding curatively resected cases) or recurrent GC. This trial was approved by the central ethics committee of the Japanese Foundation for Multidisciplinary Treatment of Cancer (JFMC) and the institutional review boards of all participating centers. In total, 1427 cases of GC were studied, of which 396 cases were proximal and 1031 were distal. Patients were classified into two groups on the basis of age (younger than 65 years or 65 years or older), according to the WHO classification [14]. All patients provided written informed consent before undergoing study-specific screening procedures. The trial was registered with the University Hospital Medical Information Network (UMIN) Clinical Trials Registry (UMIN ID UMIN000006190). Patient information was collected on the basis of the Japanese Classification of Gastric Carcinoma (third English edition) [15].
Selection criteria
Eligible patients were aged 20 years or older with histologically confirmed adenocarcinoma and in whom metastatic or recurrent GC had been diagnosed after August 2011. Additional eligibility criteria included available pathological tissue samples (six 4-μm-thick tissue sections), and written informed patient consent and consent to disseminate the clinical data.
HER2 evaluation
Excised tissue was formalin fixed and paraffin embedded by conventional histological methods. Six 3–5-µm sections were submitted per paraffin-embedded tissue block to allow assessment of the HER2 status: one section was used for each of hematoxylin and eosin staining, IHC, IHC negative control, and FISH, and the remaining two sections were retained as backup specimens. HER2 evaluation was performed centrally with an in vitro diagnosis kit validated by the Japanese Ministry of Health, Labour and Welfare, according to the manufacturer’s procedure as follows: tissue sections were tested for HER2 status by IHC with the PATHWAY anti-HER2 (4B5) rabbit monoclonal primary antibody (Roche Diagnostics, Tokyo, Japan), and by FISH with a PathVysion HER-2 DNA probe kit (Abbott Japan, Tokyo, Japan). IHC and FISH results were interpreted centrally, and HER2 positivity was defined as an IHC score of 3+ and/or a positive FISH result in accordance with the ToGA study parameters [2]. High HER2 expression was defined as an IHC score of 2+/positive FISH result or an IHC score of 3+, and low HER2 expression was defined as an IHC score of 0/positive FISH result or an IHC score of 1+/positive FISH result. The IHC scoring criteria were as follows: IHC score 0, no staining or membrane staining in less than 10 % of invasive tumor cells; IHC score 1+, weak membrane staining in 10 % or more of invasive tumor cells; IHC score 2+, weak to moderate complete or basolateral membrane staining in 10 % or more of invasive tumor cells; and IHC score 3+, moderate to strong complete or basolateral membrane staining in 10 % or more of invasive tumor cells. To determine FISH-positive status, we determined the fluorescence signal ratio of HER2 (orange) to chromosome enumeration probe 17 (CEP17; green) by counting 20 cancer cells under a fluorescence microscope with a ×100 objective lens. A sample was considered negative for gene amplification (FISH negative) if the HER2-to-CEP17 ratio was less than 2.0, and positive for gene amplification (FISH positive) if the ratio was 2.0 or greater. A HER2-to-CEP17 ratio of 1.8–2.2 (inclusive) was considered equivocal, and was found in 40 cancer cells. Samples were evaluated with a conventional histopathology method, and associations between clinicopathological factors and HER2 positivity or low HER2 expression were examined.
Statistical analysis
Data were analyzed with the Statistical Package for SAS version 9.2 (SAS Institute, Cary, NC, USA). Fisher’s test, Wilcoxon’s test, and the chi-squared test were used to test the association between HER2 status and clinicopathological characteristics. To assess the association of HER2 status with clinicopathological features, univariate and multivariate logistic regression analyses were performed. Confidence intervals were computed with the normal approximation of the binomial distribution.
Results
Patient and sample characteristics
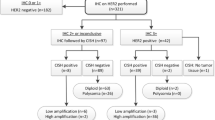
The trial profile is summarized in Fig. 1. A total of 1461 patients from 157 sites were registered between September 2011 and June 2012. Of these, the HER2 status of 1427 patients was evaluated by both IHC and FISH. Samples were collected from the major tumor site in each patient and were categorized as proximal if they were located in the upper third of the stomach or in the esophagus, and distal if they were situated in the middle third or lower third of the stomach; 27.8 % (396/1427) were proximal GCs and 72.2 % (1031/1427) were distal GCs. Patient and sample characteristics at the baseline are summarized in Table 1. The median age of the patients was 68 years (range 23–99 years). The correlations between patient or sample characteristics and HER2 status are summarized in Table 2. Histopathological groupings based on the Lauren classification revealed that 642 patients had intestinal-type tumors and 770 had diffuse-type tumors. Samples were obtained via surgical excision (678 patients) or biopsy (749 patients), and sample collection sites consisted of primary tumors (1348 patients) or metastatic regions (79 patients). HER2-positivity rates in surgically resected tumors and biopsy specimens were significantly different at 18.4 and 23.6 % (Fisher’s test, P = 0.016), respectively (Table 2). In univariate analysis, the factor biopsy specimen was found to be significantly associated with HER2 positivity (Fig. 2a). However, this association was lost in the multivariate analysis (Fig. 2b).
Correlation of human epidermal growth factor receptor 2 (HER2) positivity with clinicopathological factors. a Univariate analysis of HER2 positivity (immunohistochemistry score 3+ and/or fluorescence in situ hybridization positive) in samples from gastric cancer (GC) patients. b Multivariate analysis of HER2-positivity in samples from GC patients (n = 1088). Red squares indicate a significant association with HER2 status (HER2 positive/negative). All P values are two-sided, with P < 0.05 indicating statistical significance. CI confidence interval, CY peritoneal lavage cytology, dM distant metastasis excluding that detected in the peritoneum, by peritoneal lavage cytology, and in the liver, H hepatic metastasis, N lymph node metastasis, P peritoneal metastasis, PS performance status, T depth of tumor invasion (color figure online)
HER2 positivity and correlation with clinicopathological factors
The overall HER2-positivity rate (IHC score 3+ and/or FISH positive) was 21.2 % [95 % confidence interval (CI) 19.1–23.4; 302 of 1427 patients]. There was no significant difference (P = 0.885; Fisher’s exact test, two-sided) in HER2 positivity between proximal GC cases (21.5 %; 85 of 396 cases) and distal GC cases (21.0 %; 217 of 1031 cases). The incidence of high HER2 protein expression (IHC score 3+ or IHC score 2+ and FISH positive) was 15.6 % (223 of 1427 patients). FISH was positive in 47.3 % of IHC score 2+ cases (61 of 129 patients) and 97.5 % of IHC score 3+ cases (158 of 162 patients) (Table 3). In the univariate analysis, HER2 positivity was significantly correlated with sex, histological type, peritoneal metastasis, hepatic metastasis, distant metastasis excluding that detected in the peritoneum, by peritoneal lavage cytology, and in the liver, depth of tumor invasion, macroscopic type, primary tumor location, size, and sample source (Fig. 2a). Multivariate logistic regression analysis revealed that intestinal type, absence of peritoneal metastasis, and hepatic metastasis were independent factors related to HER2 positivity (Fig. 2b). Sampling conditions such as number of biopsy samples, formalin concentration, formalin-fixation time, and sample source had no significant effect on HER2 positivity.
Correlation of HER2 gene amplification by FISH with clinicopathological factors in IHC score 0/1+ cases
The incidence of low HER2 expression (IHC score 0/FISH positive or IHC score 1+/FISH positive) was 7.0 % (79 of 1136 patients); of these patients, 3.2 % of IHC score 0 cases (19 of 592 patients) and 11 % of IHC score 1+ cases (60 of 544 patients) were FISH positive (Table 3). In the univariate analysis, low HER2 expression was significantly correlated with sex, histological type, peritoneal metastasis, hepatic metastasis, depth of tumor invasion, and primary tumor location (Fig. 3a). Finally, multivariate logistic regression analysis revealed that age (65 years or older), intestinal type, and T1–T3 stage were independent factors related to low HER2 expression (Fig. 3b). We performed ad hoc analysis in the surgical specimen group. In the univariate analysis (n = 569), low HER2 expression was significantly correlated with sex (odds ratio 0.409, 95 % CI 0.178–0.940, P = 0.035), histological type (odds ratio 0.257, 95 % CI 0.131–0.507, P < 0.001), hepatic metastasis (odds ratio 4.598, 95 % CI 2.013–10.505, P < 0.001), depth of tumor invasion (odds ratio 0.405, 95 % CI 0.215–0.763, P = 0.005), and formalin concentration (odds ratio 1.949, 95 % CI 1.035–3.669, P = 0.039). However, multivariate logistic regression analysis revealed that there were no independent factors related to low HER2 expression in the 392 of 569 patients for whom data were available.
Correlation of human epidermal growth factor receptor 2 (HER2) gene amplification assessed by fluorescence in situ hybridization (FISH) with clinicopathological factors in immunohistochemistry (IHC) score 0/1+ cases. a Univariate analysis of low HER2 expression as assessed by IHC score 0/FISH-positive or IHC score 1+/FISH-positive samples from gastric cancer patients. b Multivariate analysis of low HER2 expression as assessed by IHC score 0/FISH-positive or IHC score 1+/FISH-positive samples from gastric cancer patients (n = 874). Red squares indicate a significant association with HER2 status (IHC score 0/FISH positive or IHC score 1+/FISH positive). All P values are two-sided, with P < 0.05 indicating statistical significance. CI confidence interval, CY peritoneal lavage cytology, dM distant metastasis excluding that detected in the peritoneum, by peritoneal lavage cytology, and in the liver, H hepatic metastasis, N lymph node metastasis, P peritoneal metastasis, PS performance status, T depth of tumor invasion (color figure online)
Discussion
Previous studies reported that the rate of HER2 positivity (IHC score 3+ and/or FISH positive) in Japanese GC patients was approximately 10–20 % [5–7], but testing methods and interpretation criteria were not standardized. In this study, HER2 status was centrally assessed with a standardized method, which was used to prospectively interpret both the IHC data and the FISH data of the ToGA study; The rate of HER2 positivity was 21.2 % in Japanese patients, identical to the ToGA screening population [3]. The rate of HER2 positivity was reported as 27 % in Japanese patients in the ToGA study [4], higher than previously reported rates. This might be a result of bias toward patient selection from past reports [16–18], because the primary purpose of the ToGA study was to assess the clinical efficacy and safety of trastuzumab rather than to evaluate HER2 positivity. The incidence of higher HER2 protein expression (IHC score 2+/FISH positive or IHC score 3+; 15.6 %) and the proportions of FISH positivity in IHC score 0 and IHC score 1+ cases (3.2 and 11 %) were comparable with those reported in the ToGA study [3]. Similarly, the concordance between IHC and FISH in our results is consistent with that reported in the ToGA study.
A high correlation between HER2 positivity and histological subtype was reported by several authors [19–24]. In the ToGA study, HER2 positivity varied significantly according to histological subtype (intestinal type 31.8 %; diffuse type 6.1 %; mixed type 20 %) [3]; thus, intestinal type was strongly correlated with HER2 expression. Several reports indicated that intestinal type is associated with hematogenous metastasis, particularly to the liver [25], and with older age [26], whereas the diffuse type is adversely related to peritoneal dissemination [27]. In the present study, intestinal type, absence of peritoneal metastasis, and hepatic metastasis were shown to be independent factors related to HER2 positivity in a multivariate logistic regression analysis. This agrees with what is known about the histological type, i.e., intestinal or diffuse, and the association with accompanying hepatic or peritoneal metastasis, respectively.
Moreover, intestinal type, age (65 years or older), and T1–T3 stage were independent factors related to low HER2 expression (IHC score 0/1+ and FISH positive). This result reveals that HER2-related factors are associated with intestinal-type GCs. Diffuse-type GCs are more malignant than their intestinal-type counterparts, demonstrating early invasion into the muscularis propria [25]. A previous report demonstrated that diffuse-type advanced GC was significantly associated with advanced pathological T stage [28]. Thus, diffuse type is commoner in T4 tumors, whereas intestinal type is commoner in T1–T3 tumors. As intestinal type is the most robust factor related to HER2 expression, T1–T3 stage may be an independent factor related to low HER2 expression even in intestinal-type IHC score 0/1+ GC cases. However, the current study was limited by the extent and accuracy of the T staging, which was determined by either pathological or clinical diagnosis methods. To resolve these limitations, we performed ad hoc analyses for low HER2 expression (IHC score 0/FISH positive or IHC score 1+/FISH positive) in the surgical specimen group, because the T stage in the surgical samples was accurately determined pathologically. T1–T3 stage was statistically significantly correlated with low HER2 expression in the univariate analysis, but was not significantly correlated in the multivariate analysis. Likewise, intestinal type, sex, hepatic metastasis, and formalin concentration were statistically significantly associated with low HER2 expression in the univariate analysis; however, there were no significant differences in the multivariate analysis. The discrepancies in these analyses may result from the multivariate analysis being performed only in 392 of 569 cases owing to missing data in the remaining cases, thereby conferring a lack of statistical significance. Further studies are required to confirm this result, and considering these limitations, we cannot conclude that depth of tumor invasion is a factor related to low HER2 expression.
There are several factors that are reported to affect HER2 staining results, such as type of fixative, total fixation time, fixative pH, tissue type, and time before fixation. In the present study, we evaluated the relationship between HER2 expression and sampling conditions; however, the number of biopsy samples, formalin concentration, and formalin-fixation time had no significant effect on HER2 positivity and low HER2 expression. Unfortunately, the recommended conditions for fixation could not be adhered to in this study because the biopsy specimens and surgically resected specimens were mixed up and because correlations between formalin concentration and fixation time could not be undertaken. Moreover, the time before fixation (so-called cold ischemia) and the specimen size were unclear. Further prospective studies aiming to comprehensively evaluate the effects of formalin concentration, formalin-fixation time, and cold ischemia on HER2 testing are required.
There was concern that examination of gastric biopsy samples alone might introduce false-positive and/or false-negative data, because HER2 intratumoral heterogeneity in GC is observed in 20–70 % of HER2-positive tumors [13, 29] and is the major cause of discrepancies between biopsy samples and surgical specimens. In the multivariate analysis of the present study results, HER2-positivity rates in surgically resected tumors and biopsy samples were not significantly different, similar to the findings in the HER-EAGLE study [24]. However, these studies were limited in that the correlation between surgical specimens and biopsy samples was not paired, although this contrasts with the GERCOR study, where the overall concordance rate between surgical specimens and paired biopsy samples reached 94 % [12]. We also examined the concordance between predominant histological type and histological type with a HER2-positive component, which was determined as 81.3 % with the Lauren classification (data not shown). Approximately 20 % of cases showed a discrepancy; therefore, gastroenterologists should consider performing multiple biopsy sampling from varied collection sites to overcome tumor heterogeneity in GC.
In conclusion, HER2 expression in a Japanese GC population was similar in distribution to that identified in the ToGA study. Intestinal type was revealed as an independent factor related to both HER2 positivity and low HER2 expression.
References
Cuello M, Ettenberg SA, Clark AS, Keane MM, Posner RH, Nau MM, et al. Down-regulation of the erbB-2 receptor by trastuzumab enhances tumor necrosis factor related apoptosis inducing ligand mediated apoptosis in breast and ovarian cancer cell lines that overexpress erbB-2. Cancer Res. 2001;61:4892–900.
Bang YJ, Van Cutsem E, Feyereislova A, Chung HC, Shen L, Sawaki A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomized controlled trial. Lancet. 2010;376:687–97.
Van Cutsem E, Bang YJ, Feng-yi F, Xu JM, Lee KW, Jiao SC, et al. HER2 screening data from ToGA: targeting HER2 in gastric and gastroesophageal junction cancer. Gastric Cancer. 2014. doi:10.1007/s10120-014-0402-y.
Bang YJ, Chung H, Xu J, Lordick F, Sawaki A, Lipatov O, et al. Pathological features of advanced gastric cancer (GC): relationship to human epidermal growth factor receptor 2 (HER2) positivity in the global screening programme of the ToGA trial. J Clin Oncol. 2009;27:4556.
Yonemura Y, Ninomiya I, Yamaguchi A, Fushida S, Kimura H, Ohoyama S, et al. Evaluation of immunoreactivity for erbB-2 protein as a marker of poor short term prognosis in gastric cancer. Cancer Res. 1991;51:1034–8.
Uchino S, Tsuda H, Maruyama K, Kinoshita T, Sasako M, Saito T, et al. Overexpression of c-erbB-2 protein in gastric cancer. Cancer. 1993;2:3179–84.
Ooi A, Kobayashi M, Mai M, Nakanishi I. Amplification of c-erbB-2 in gastric cancer: detection in formalin-fixed, paraffin-embedded tissue by fluorescence in situ hybridization. Lab Invest. 1998;78:345–51.
Chen XZ, Zhang WH, Yao WQ, Liu JP, Zhou ZG, Chen ZX, et al. Immunohistochemical HER2 expression not associated with clinicopathological characteristics of stage I-III gastric cancer patients. Hepatogastroenterology. 2014;61:1817–21.
Shan L, Ying J, Lu N. HER2 expression and relevant clinicopathological features in gastric and gastroesophageal junction adenocarcinoma in a Chinese population. Diagn Pathol. 2013;8:76.
Son HS, Shin YM, Park KK, Seo KW, Yoon KY, Jang HK, et al. Correlation between HER2 overexpression and clinicopathological characteristics in gastric cancer patients who have undergone curative resection. J Gastric Cancer. 2014;14:180–6.
Pirrelli M, Caruso ML, Maggio MD, Armentano R, Valentini AM. Are biopsy specimens predictive of HER2 status in gastric cancer patients? Dig Dis Sci. 2013;58:397–404.
Watson S, Validire P, Cervera P, Zorkani N, Scriva A, Lemay F, et al. Combined HER2 analysis of biopsies and surgical specimens to optimize detection of trastuzumab-eligible patients in eso-gastric adenocarcinoma: a GERCOR study. Ann Oncol. 2013;24:3035–9.
Warneke VS, Behrens HM, Boger C, Becker T, Lordick F, Ebert MP, et al. Her2/neu testing in gastric cancer: evaluating the risk of sampling errors. Ann Oncol. 2013;24:725–33.
World Health Organization. Definition of an older or elderly person. http://www.who.int/healthinfo/survey/ageingdefnolder/en/.
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011;14:101–12.
Polkowski W, van Sandick J, Offehaus G, ten Kate FJ, Mulder J, Obertop H, et al. Prognostic value of Lauren classification and c-erbB-2 oncogene overexpression in adenocarcinoma of the esophagus and gastroesophageal junction. Ann Surg Oncol. 1999;6:290–7.
Tanner M, Hollmén M, Junttila TT, Kapanen AI, Tommola S, Soini Y, et al. Amplification of HER-2 in gastric carcinoma: association with topoisomerase IIa gene amplification, intestinal type, poor prognosis and sensitivity to trastuzumab. Ann Oncol. 2005;16:273–8.
Lee KE, Lee HJ, Kim YH, Yu HJ, Yang HK, Kim WH, et al. Prognostic significance of p53, nm23, PCNA and c-erbB-2 in gastric cancer. Jpn J Clin Oncol. 2003;33:173–9.
Grabsch H, Silvakumar S, Gray S, Gabbert HE, Müller W. HER2 expression in gastric cancer: rare, heterogeneous and of no prognostic value-conclusions from 924 cases of two independent serious. Cell Oncol. 2010;63:839–42.
Marx AH, Tharun L, Muth J, Dancau AM, Simon R, Yekebas E, et al. Her-2 amplification is highly homogeneous in gastric cancer. Hum Pathol. 2009;40:769–77.
Barros-Silva JD, Leitao D, Afonso L, Vieira J, Dinis-Ribeiro M, Fragoso M, et al. Association of ERBB2 gene status with histopathological parameters and disease-specific survival in gastric carcinoma patients. Br J Cancer. 2009;100:487–93.
Matsubara J, Yamada Y, Hirashima Y, Takahari D, Okita N, Takashima A, et al. Impact of insulin-like growth factor type 1 receptor, epidermal growth factor receptor, and HER2 expressions on outcomes of patients with gastric cancer. Clin Cancer Res. 2008;14:3022–9.
Sheng WQ, Huang D, Ying JM, Lu N, Wu HM, Liu YH, et al. HER2 status in gastric cancers: a retrospective analysis from four Chinese representative clinical centers and assessment of its prognostic significance. Ann Oncol. 2013;24:2360–4.
Huang D, Lu N, Fan Q, Sheng W, Bu H, Jin X, et al. HER2 status in gastric and gastroesophageal junction cancer assessed by local and central laboratories: Chinese results of the HER-EAGLE study. PLoS One. 2013;8:1–7.
Esoki Y, Hirayama R, Hirokawa K. A comparison of patterns of metastasis in gastric cancer by histologic type and age. Cancer. 1990;65:2086–90.
Zheng H, Takahashi H, Murai Y, Cui Z, Nomoto K, Miwa S, et al. Pathobiological characteristics of intestinal and diffuse-type gastric carcinoma in Japan: an immunostaining study on the tissue microarray. J Clin Pathol. 2007;60:273–7.
Wu MS, Yang KC, Shun CT, Hsiao TJ, Lin CC, Wang HP, et al. Distinct clinicopathological characteristics of diffuse- and intestinal-type gastric cancer in Taiwan. J Clin Gastroenterol. 1997;25:646–9.
Yamashita K, Sakuramoto S, Katada N, Futawatari N, Moriya H, Hirai K, et al. Diffuse type advanced gastric cancer showing dismal prognosis is characterized by deeper invasion and emerging peritoneal cancer cell: the latest comparative study to intestinal advanced gastric cancer. Hepatogastroenterology. 2009;56:276–81.
Sauter G, Lee J, Bartlett JMS, Slamon DJ, Press MF. Guidelines for human epidermal growth factor receptor 2 testing: biologic and methodological considerations. J Clin Oncol. 2009;27:1323–33.
Acknowledgments
This trial was supported by the Japanese Foundation for Multidisciplinary Treatment of Cancer. Editorial support was provided by H. Nikki March and was funded by Chugai Pharmaceutical Co. Ltd.
Conflict of interest
S. Matsusaka has received commercial research grants from Taiho Pharmaceutical Co. Ltd. K. Nishikawa has received commercial research grants and personal fees from Yakult Honsha Co. Ltd, Taiho Pharmaceutical Co. Ltd, and Ajinomoto Pharmaceuticals, and personal fees from Chugai Pharmaceutical Co. Ltd. Tsumura Co. Ltd, and Terumo Corporation. T. Yoshikawa received commercial research grants and personal fees from Chugai Pharmaceutical Co. Ltd during the conduct of the study, has received grants and personal fees from Taiho Pharmaceutical Co. Ltd, Novartis Pharma K.K., Ono Pharmaceutical Co. Ltd, Yakult Honsha Co. Ltd, Covidien Japan Co. Ltd, and the nonprofit organization Kanagawa Standard Anti-cancer Therapy Support System, has received personal fees from Eli Lilly Japan K.K., Abbott Japan Co. Ltd, Kaken Pharmaceutical Co. Ltd, Johnson & Johnson K.K., Takeda Pharmaceutical Co. Ltd, Secom Medical System Co. Ltd, Nikkei Business Publications, and the nonprofit organizations Tokyo Cooperative Oncology Group, Clinical Training Support Council, and Cancer Net Japan, and has received grants from Daiichi Sankyo Co. Ltd and Nippon Kayaku Co. Ltd. A. Ochiai has received commercial research grants from Bayer Ltd, Ventana Medical Systems Inc., Eli Lilly Japan K.K., Toray Industries Inc., Takeda Pharmaceutical Co. Ltd, Taiho Pharmaceutical Co. Ltd, Merck Serono Co. Ltd, Janssen Pharmaceutical K.K., Eisai Co. Ltd, Otsuka Pharmaceutical Co. Ltd, and Daiichi Sankyo Co. Ltd, and nonfinancial support from Fujifilm Co. Ltd. S. Morita has received commercial research grants and personal fees from Chugai Pharmaceutical Co. Ltd. T. Sano has received personal fees from Taiho Pharmaceutical Co. Ltd, Sanofi K.K., Yakult Honsha Co. Ltd, and Chugai Pharmaceutical Co. Ltd. Y. Kodera has received commercial research grants and personal fees from Chugai Pharmaceutical Co. Ltd, grants and personal fees from Taiho Pharmaceutical Co. Ltd, Sanofi K.K., Bristol-Myers Squib Ltd, Merck Serono Co. Ltd, Yakult Honsha Co. Ltd, Daiichi Sankyo Co. Ltd, Otsuka Pharmaceutical Co. Ltd, Takeda Pharmaceutical Co. Ltd, Johnson & Johnson K.K., Asahi Kasei Pharma Corporation, Shionogi & Co. Ltd, Eli Lilly Japan K.K., Pfizer Japan Inc., Ajinomoto Pharmaceuticals, Ono Pharmaceutical Co. Ltd, Kaken Pharmaceutical Co. Ltd, Covidien Japan Co. Ltd, Tsumura Co. Ltd, and grants from Eisai Co. Ltd, Abbott Japan Co. Ltd, CSL Behring Ltd, Teijin Pharma Ltd, the Japan Blood Products Organization, Torii Pharmaceutical Co. Ltd, and Mitsubishi Tanabe Pharma Corporation. Y. Kakeji has received personal fees from Chugai Pharmaceutical Co. Ltd. J. Sakamoto has received personal fees from Takeda Pharmaceutical Co. Ltd and Tsumura Co. Ltd. K. Yoshida received commercial research grants from Chugai Pharmaceutical Co. Ltd during the conduct of the study, has received grants and personal fees from Taiho Pharmaceutical Co. Ltd, Pfizer Japan Inc., Chugai Pharmaceutical Co. Ltd, Yakult Honsha Co. Ltd, Bristol-Myers Squibb Ltd, and Kyowa Hakko Kirin Co. Ltd, honoraria from Taiho Pharmaceutical Co. Ltd, Pfizer Japan Inc., Chugai Pharmaceutical Co. Ltd, Kyowa Hakko Kirin Co. Ltd, and Yakult Honsha Co. Ltd, and has acted as a consultant or advisor for Taiho Pharmaceutical Co. Ltd and F. Hoffmann-La Roche Ltd. All remaining authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Matsusaka, S., Nashimoto, A., Nishikawa, K. et al. Clinicopathological factors associated with HER2 status in gastric cancer: results from a prospective multicenter observational cohort study in a Japanese population (JFMC44-1101). Gastric Cancer 19, 839–851 (2016). https://doi.org/10.1007/s10120-015-0518-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-015-0518-8