Abstract
Background
The factors that affect the 6-month continuation of adjuvant chemotherapy with S-1 have not been fully evaluated. The objective of this retrospective study was to clarify the risk factors for 6-month continuation of S-1 adjuvant chemotherapy.
Methods
The study selected patients who underwent curative D2 surgery for gastric cancer, were diagnosed with stage 2 or 3 disease, had a serum creatinine level of ≤1.2 mg/dl, and received adjuvant S-1 between June 2002 and March 2011.
Results
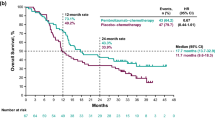
One hundred of these patients were eligible for the present study. A comparison of 6-month continuation of S-1 stratified by various clinical factors, using the log-rank test, revealed a marginally significant difference in creatinine clearance (CCr) between those patients who continued for 6 months and those who did not. A CCr of 60 ml/min was regarded as the critical point. Uni- and multivariate Cox’s proportional hazard analyses demonstrated that CCr was the only significant independent factor for the prediction of 6-month continuation. The 6-month continuation rate was 72.9 % in the patients with CCr ≥60 ml/min, and 40.0 % in patients with CCr <60 ml/min (P = 0.015). Adverse events occurred more frequently and earlier in the patients with CCr <60 ml/min than in those with CCr ≥60 ml/min.
Conclusions
CCr <60 ml/min was a significant risk factor for 6-month continuation of S-1 adjuvant chemotherapy, even though the renal function was judged as normal by the serum creatinine level. Careful attention is therefore required for S-1 continuation in patients with CCr <60 ml/min.
Similar content being viewed by others
Introduction
Gastric cancer is the fourth most common malignant disease and the second most frequent cause of cancer-related death worldwide [1].
The Adjuvant Chemotherapy Trial of TS-1 for Gastric Cancer (ACTS-GC) phase III trial has demonstrated that S-1 was effective as adjuvant chemotherapy for Japanese patients who had undergone curative D2 gastrectomy for gastric cancer and were diagnosed with pathological stage 2 or 3 disease [2]. Therefore, a curative D2 dissection and adjuvant chemotherapy with S-1 are now the standard therapy for these patients in Japan [3].
The aim of adjuvant chemotherapy is to eradicate micro-metastatic tumor cells. It is therefore essential to continue chemotherapy for a minimal length of time to ensure that these cells are eradicated. Six months of treatment is necessary for breast and colon cancer, while 12 months was defined as necessary for gastric cancer in the ACTS-GC trial. Although the optimal duration of adjuvant chemotherapy for gastric cancer is still unclear, the results of studies of other solid malignancies suggest that S-1 adjuvant treatment should be continued for at least 6 months.
Incomplete treatment with adjuvant chemotherapy resulted in markedly inferior disease-free survival in patients with breast cancer [4]. Four hundred and fifty-two of the 517 patients who received S-1 in the ACTS-GC trial continued treatment for at least 3 months (87.4 %) and 403 patients (77.9 %) continued treatment for at least 6 months. The most common cause of withdrawal was the occurrence of adverse events. It is important to identify risk factors for the continuation of S-1 adjuvant chemotherapy, because physicians can support the patients who have risk factors.
This study investigated the risk factors that affected the 6-month continuation of adjuvant chemotherapy with S-1 for gastric cancer patients who underwent D2 gastrectomy.
Patients and methods
Patients
The patients were selected from the prospective database of the Kanagawa Cancer Center, Department of Gastrointestinal Surgery, Yokohama, Japan, according to the following criteria: (1) histologically proven gastric adenocarcinoma, (2) patients who underwent a curative D2 dissection for gastric cancer as a primary treatment between June 2002 and March 2011, (3) stage 2A, 2B, 3A, 3B, or 3C disease was diagnosed pathologically according to the Japanese Gastric Cancer Association Japanese classification of gastric carcinoma, 3rd English edition [5], (4) patients started S-1 adjuvant chemotherapy at a dose of 80 mg/m2 within 6 weeks after surgery, and (5) the serum creatinine level was less than the upper limit of the normal range (≤1.2 mg/dl).
Treatment
The patients received S-1 chemotherapy and were followed on an out-patient basis. Three groups of patients received S-1: (1) those serving as a test arm of the ACTS-GC trial, (2) those serving as a test arm of the Stomach Cancer Adjuvant Multi-institutional Trial Group (SAMIT) trial [6], and (3) those in general clinical practice. The patients who were registered to the ACTS-GC trial received 40 mg of S-1 per square meter of body-surface area twice a day for 4 weeks followed by 2 weeks’ rest as one course (6 weeks’ schedule), and this protocol continued for 1 year after surgery. The patients who were registered to the SAMIT trial between February 2004 and April 2007 received the same dose as those registered to the ACTS-GC trial for 2 weeks, followed by 1 week’s rest (a 3-week schedule), and this protocol continued for 6 months after surgery, while the patients who were registered to the SAMIT trial between May 2007 and September 2009 received the same 3 weeks’ schedule of S-1 as those registered to the SAMIT trial between February 2004 and April 2007, and this protocol continued for 12 months, because the SAMIT was amended in May 2007 based on the report of the ACTS-GC. The remaining patients (those in clinical practice) received S-1 at the same dose as those registered to the SAMIT trial between May 2007 and September 2009 for 12 months following the protocol of the ACTS-GC after the results of ACTS-GC were reported. Patients with a body-surface area of less than 1.25 m2 received 80 mg daily, those with a body-surface area of 1.25 m2 or more but less than 1.5 m2 received 100 mg daily, and those with a body-surface area of 1.5 m2 or more received 120 mg daily. Any reduction of the starting dose, suspension or delay, and dose reduction were determined by the protocol of each clinical trial in the patients registered to the ACTS-GC or the SAMIT trial. Reduction of the starting dose, delay, and dose reduction in the patients who received S-1 in clinical practice were determined following the criteria of the ACTS-GC trial. Briefly, the treatment was delayed when patients had hematological adverse events of grade 3 or more, or non-hematological adverse events of grade 2 or more, until all adverse events recovered to grade 0 or 1; and treatment was re-started at a reduced dose of 100 mg, 80 mg, or 50 mg based on the body surface area described above. The patients who started with the 6-week schedule of S-1 and experienced the adverse events described above at a reduced dose were switched from the 6-week schedule to the 3-week schedule.
Evaluation and statistical analyses
Toxicities were graded according to the National Cancer Institute common toxicity criteria version 3.0. Renal impairment was measured in terms of creatinine clearance, calculated by the formula of Cockroft and Gault [7]. Differences in the 6-month continuation of S-1 were calculated using the Kaplan–Meier method and compared by the log-rank test. In this study, when the patients were given S-1 for more than 6 months after surgery, such patients were treated as censored cases at 6 months. When S-1 was discontinued at less than 6 months after surgery, we defined that the event had occurred on the day when the physicians decided on the discontinuation of S-1 treatment according to the protocol, due to adverse events, the patient’s refusal due to adverse events, the patient’s refusal due to reasons other than adverse events, disease recurrence, or death. Cox’s proportional hazard model was used to perform uni- and multivariate analyses to determine the risk factors for continuation of S-1 chemotherapy. A P value of <0.05 was defined as statistically significant. An SPSS software package (v11.0J Win; SPSS, Chicago, IL, USA) was used for all statistical analyses.
Results
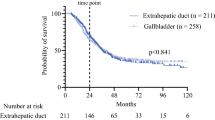
A total of 258 patients underwent surgical resection and were pathologically diagnosed with stage 2A, 2B, 3A, 3B, or 3C disease. A flow diagram of the 258 patients is shown in Fig. 1. One hundred of these patients were eligible for the present study. Nine patients had been registered to the ACTS-GC trial between June 2002 and June 2004, and 20 to the SAMIT trial between August 2004 and February 2009. Seventy-one patients received S-1 treatment in clinical practice after the results of the ACTS-GC trial were reported, while 5 patients in this study rejected S-1 adjuvant chemotherapy between August 2006 and March 2011. One hundred of the above 258 patients were eligible for the present study. The patients’ ages ranged from 36 to 80 years (median 64.5 years). Sixty-nine patients were male, and 31 were female.
The median serum creatinine level was 0.74 mg/dl (range 0.42–1.20 mg/dl) and the median creatinine clearance (CCr) was 80.7 ml/min (range 43.2–138.9 ml/min). The median follow-up period was 25.0 months (range 1.4–78.1 months).
A log-rank test comparison of the 6-month continuation rate with the 3-month continuation rate, stratified by various clinical factors, revealed a marginally significant difference in CCr between the groups (Table 1). A CCr of 60 ml/min was defined as the optimal critical point of classification considering the 3- and 6-month continuation rates. Each clinicopathological factor was categorized as shown in Table 2, and was analyzed for risk of S-1 continuation. Univariate analyses demonstrated that CCr was the only significant risk factor. The CCr and type of gastrectomy were selected for the final model to be submitted to multivariate analysis (Table 2). Figure 2 shows that the continuation rate at 6 months was 72.9 % in patients with high CCr, and it was 40.0 % in those with a low CCr. Five patients stopped S-1 within 6 months after surgery due to disease recurrence. Table 3 shows the details of the patients who stopped S-1 for any reason. The reasons for discontinuation included the protocol-defined rule for adverse events in 12 patients, the patient’s refusal due to adverse events in 12, the patient’s refusal due to reasons other than adverse events in 2, and disease recurrence in 5; there were no deaths. The results showed that adverse events occurred more frequently and earlier in the patients with a low CCr than in those with a high CCr. About half of the patients with a low CCr could not continue S-1 for more than 1 month. Although these patients were informed of the possibility of continuation through dose attenuation or changing the treatment schedule, all rejected further S-1 adjuvant treatment.
Discussion
This report demonstrated that CCr <60 ml/min was a significant risk factor for the continuation of S-1 adjuvant chemotherapy, even though renal function was judged as normal by the serum creatinine level. Therefore, it is necessary to calculate the CCr level when patients are starting S-1 adjuvant chemotherapy. Careful attention is required for S-1 continuation in patients with CCr <60 ml/min. Moreover, only half of the patients with CCr <60 ml/min could continue S-1 for more than 1 month, thus suggesting that these patients had little chance to benefit from S-1 adjuvant chemotherapy.
S-1 is an oral fluoropyrimidine, containing tegafur (a prodrug of fluorouracil), 5-chloro-2,4-dihydropyrimidine (CDHP), and potassium oxonate. CDHP is an inhibitor of dihydropyrimidine dehydrogenase (DPD), which is the rate-limiting enzyme for the degradation of fluorouracil [8]. The clearance of CDHP is reduced by renal dysfunction, resulting in a high blood concentration of 5-FU due to decreased DPD activity [9, 10]. Yamanaka et al. [11] reported that baseline renal impairment was a significant risk factor for grade 3–4 adverse events caused by S-1 chemotherapy in advanced gastric cancer. They showed that the incidences of key severe adverse events, such as neutropenia, nausea/vomiting, diarrhea, stomatitis, rash, and pigmentation were significantly higher in patients with a CCr level under 50 ml/min than in those who had a CCr level over 80 ml/min [11]. In the present series, 8 of 15 patients with low CCr stopped S-1 adjuvant chemotherapy, whereas only 15 of 85 patients with high CCr discontinued treatment due to toxicities. Moreover, 7 of the 8 patients with low CCr stopped S-1 adjuvant chemotherapy in the first cycle due to toxicities, whereas only 6 of the 15 with high CCr withdrew from therapy. Adverse events occurred more frequently and earlier in the patients with a low CCr than in those with a high CCr.
Of note, the type of gastrectomy was only marginally significant in the final model submitted to multivariate analysis. The 6-month continuation of adjuvant chemotherapy with S-1 following total gastrectomy (TG) tended to be worse than that following distal gastrectomy (DG). This may have been associated with the amount of food intake or body weight loss. Generally, body weight loss was reported to decrease by 10–20 % before surgery and to be more severe following TG than that after a distal resection [12]. The patients who undergo DG have a remnant stomach that is usable as a reservoir, while the patients who undergo TG do not. Therefore, patients who undergo TG do not have larger meal volumes than those who undergo DG. For example, Noguchi et al. [13] evaluated 97 patients with gastrectomy that was classified as TG or DG. They found the patients in the TG group were taking only 1020 ± 391 kcal/day at the time of discharge, whereas those in the DG group were taking 1326 ± 442 kcal/day (P < 0.05) [13]. Moreover, most patients with DG started to gain weight within the first three months after discharge, whereas only half of those with TG gained weight in the same period, and their weight recovery was delayed by 3–6 months. Body weight loss and poor food intake may affect the 6-month continuation of adjuvant chemotherapy with S-1.
A comparison of the present findings with the results of the ACTS-GC trial revealed that the continuation rate tended to be lower in the present study. The clinical trial had strictly defined rules for the discontinuation of S-1, while the daily clinical practice cohort did not. In the daily clinical practice cohort, even though the physicians explained the details of the ACTS-GC trial to the patients, S-1 could be discontinued due to grade 1–2 non-hematological toxicities such as anorexia, fatigue, and nausea, because the quality of life of patients is affected more by non-hematological toxicity than by hematological toxicity. In fact, in the present study 9 of the 85 patients with a high CCr and 5 of the 15 patients with a low CCr stopped S-1 chemotherapy due to grade 1–2 non-hematological or hematological toxicity.
Special attention is required when interpreting the present results. This study has several limitations. First, the optimal cutoff value of CCr is unclear. When comparing the 3- and 6-month continuation rates by the log-rank test according to CCr, the two continuation rates were clearly separated by CCr 60 ml/min. Moreover, when we compared the continuation rates of the CCr <50 ml/min group and the group with CCr ≥50 and <60 ml/min, there was no significant difference in the rates between the two groups (data not shown). Therefore, we set the CCr cutoff value at 60 ml/min in this study. However, the appropriate cutoff value might dependon the patients’ backgrounds. Thus, an appropriate cutoff value should be determined in other validation studies. Second, there is a possibility of selection bias in this series, as shown in Fig. 1. (1) All patients who were registered to the adjuvant phase III trial were randomly assigned to surgery alone, S-1, or other chemotherapeutic regimens; therefore, there was no selection bias among these patients. (2) Eighty-six patients were not registered to the trial until after August 2006. Only 5 of these patients rejected S-1 chemotherapy even though S-1 was the standard treatment at this time. Selection bias may have been introduced with these 5 patients, although the proportion is very low. (3) Sixty-nine patients were not registered in the trial before August 2006. None of these patients received S-1 because the standard treatment before August 2006 was surgery alone. On the other hand, 65 patients were registered to the trial and 17 were assigned to S-1. There may have been a selection bias with these 17 patients, because only patients who fulfilled the strict eligibility criteria were enrolled in the trial. However, this proportion is not very high. Third, this was a retrospective single-center study with a small sample size. In this study, we calculated the total days of S-1 treatment based on the patients’ records. We obtained the data from patients’ records. However, it is difficult to know whether the patients actually took the medicine. Thus, the continuation rate might not be accurate. Therefore, the present results should be validated in another series with a larger number of patients.
In summary, a CCr of <60 ml/min was a significant risk factor for the continuation of S-1 adjuvant chemotherapy, even though renal function was judged as normal by the serum creatinine level. Careful attention is required for S-1 continuation in patients with a CCr of <60 ml/min.
References
Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108.
Sakuramoto S, Sasako M, Yamaguchi T, Kinoshita T, Fujii M, Nashimoto A, et al. Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med. 2007;357:1810–20.
Sano T, Aiko T. New Japanese classifications and treatment guidelines for gastric cancer: revision concepts and major revised points. Gastric Cancer. 2011;14:97–100.
Bonadonna G, Valagussa P. Dose-response effect of adjuvant chemotherapy in breast cancer. N Engl J Med. 1981;304:101–5.
Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma, 3rd English edition. Gastric Cancer. 2011;14:101–12.
Tsuburaya A, Sakamoto J, Morita S, et al. A randomized phase III trial of post-operative adjuvant oral fluoropyrimidine versus sequential paclitaxel/oral fluoropyrimidine; and UFT versus S1 for T3/T4 gastric carcinoma: the Stomach Cancer Adjuvant Multi-institutional Trial Group (Samit) Trial. Jpn J Clin Oncol. 2005;35:672–5.
Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41.
Shirasaka T, Shimamato Y, Ohshimo H, Yamaguchi M, Kato T, Yonekura K, et al. Development of a novel form of an oral 5-fluorouracil derivative (S-1) directed to the potentiation of the tumor selective cytotoxicity of 5-fluorouracil by two biochemical modulators. Anticancer Drugs. 1996;7:548–57.
Tatsumi K, Fukushima M, Shirasaka T, Fujii S. Inhibitory effects of pyrimidine, barbituric acid and pyridine derivatives on 5-fluorouracil degradation in rat liver extracts. Jpn J Cancer Res. 1987;78:748–55.
Hirata K, Horikoshi N, Aiba K, Okazaki M, Denno R, Sasaki K, et al. Pharmacokinetic study of S-1, a novel oral fluorouracil antitumor drug. Clin Cancer Res. 1999;5:2000–5.
Yamanaka T, Matsumoto S, Teramukai S, Ishiwata R, Nagai Y, Fukushima M. Safety evaluation of oral fluoropyrimidine S-1 for short- and long-term delivery in advanced gastric cancer: analysis of 3,758 patients. Cancer Chemother Pharmacol. 2008;61:335–43.
Fein M, Fuchs KH, Thalheimer A, Freys SM, Heimbucher J, Thiede A. Long-term benefits of Roux-en-Y pouch reconstruction after total gastrectomy: a randomized trial. Ann Surg. 2008;247:759–65.
Noguchi Y, Tsuburaya A, Makino T, et al. Metabolic alterations in totally gastrectomised patients—caloric intake and energy consumption. Asian J Surg. 1992;15:97–102.
Acknowledgments
This work was supported, in part, by the Non-Governmental Organization Kanagawa Standard Anti-cancer Therapy Support System.
Conflict of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aoyama, T., Yoshikawa, T., Hayashi, T. et al. Risk factors for 6-month continuation of S-1 adjuvant chemotherapy for gastric cancer. Gastric Cancer 16, 133–139 (2013). https://doi.org/10.1007/s10120-012-0158-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-012-0158-1