Abstract
Background
Decision-making for surgical palliation remains one of the most challenging clinical scenarios. We investigated the optimal indications for surgical palliation in advanced gastric cancer (AGC) patients presenting with gastrointestinal (GI) obstruction.
Methods
A retrospective analysis was performed on 53 consecutive patients who underwent surgical palliation for GI obstruction caused by AGC between 2000 and 2007 at Osaka National Hospital. The clinical course of each patient was followed until death. Postoperative improvement of oral intake, achievement of hospital discharge, and implementation of chemotherapy in each patient were documented and used as a triad to assess the quality of life (QOL). Prognostic factors for overall survival were investigated by univariate and multivariate analyses. In addition, postoperative morbidity and mortality rates were recorded.
Results
Of the entire patient cohort, 64% demonstrated a QOL improvement by having achieved the triad. Performance status (PS) of 1 or less was the only significant predictive factor for QOL improvement. The median survival time (MST) of the whole patient cohort following surgical palliation was 161 days, while the MSTs of patients fulfilling the triad and of those failing to achieve the triad were 253 and 60 days, respectively, with a significant difference between them (P < 0.0001). PS of 1 or less (hazard ratio 0.265, P = 0.0008) and recurrent disease (hazard ratio 0.394, P = 0.043) were identified as significant independent prognostic factors for longer survival on multivariate analysis. Overall morbidity and 30-day postoperative mortality rates were 24.5% (13 patients) and 7.5% (4 patients) respectively.
Conclusions
In AGC patients presenting with GI obstruction, surgical palliation was beneficial in patients with PS of 0–1 and those with recurrent disease, in terms of improved QOL and prolonged survival, with acceptable operative morbidity and mortality rates.
Similar content being viewed by others
Introduction
Gastric cancer is the second leading cause of cancer-related death worldwide [1]. Unfortunately, the disease in some patients is so advanced at diagnosis as to preclude curative resection. The prognosis of patients with incurable advanced gastric cancer (AGC) is dismal and most of them die within 1 year [2]. In addition, patients with incurable AGC often present with various clinical symptoms such as abdominal pain/distension, anorexia, weight loss, and nausea/vomiting [3], as well as poor oral intake due to gastrointestinal (GI) obstruction, represented by gastric outlet obstruction and bowel obstruction caused by peritoneal dissemination, features which underscore the importance of palliative treatment for AGC. The severity of these presentations, ranging from mild and elective to severe and emergent, sometimes demands palliative operative procedures to relieve symptoms, maintain patient independence and function, allow for home care, and minimize the burden of care-givers [4]. However, decision-making for surgical care is very difficult because a number of patient factors such as age, performance status (PS), nutritional status, co-morbidities, and previous and future anti-cancer treatment, as well as postoperative morbidity and mortality, could affect the outcome of surgical palliation. Surgical palliation can be one of the most challenging clinical scenarios, balancing the risks and benefits of the intervention in terms of quality of life (QOL) and prognosis. Ideal surgical palliation is expected to obtain durable symptom resolution leading to improved QOL and prolonged survival.
This retrospective analysis was conducted to investigate the factors that affect the outcome of surgical palliation in patients with incurable AGC presenting with malignant GI obstruction and to clarify optimal indications for surgical palliation, thus avoiding worthless operation.
Patients and methods
Patient characteristics
A retrospective analysis was performed on 53 consecutive patients who underwent surgical palliation for GI obstruction caused by primary unresectable or incurable recurrent gastric cancer (GC) between January 1, 2000 and December 31, 2007 at Osaka National Hospital. Patients who had received gastrectomy with palliative intent or tumor debulking were excluded from the present study. The clinical characteristics of these 53 patients, 37 males and 16 females, with a median age of 62 (range 33–86) years, are summarized in Table 1. Thirty-six patients had a PS of 1 or less on the Eastern Cooperative Oncology Group (ECOG) scale, and 17 patients had a PS of 2. Fourteen patients had primary unresectable GC, causing gastric outlet obstruction in 6 and peritoneal dissemination in 8; while 39 patients had incurable recurrent GC involving peritoneum in 36, gastric remnant in 2, and gastroduodenostomy in 1. With respect to co-morbidities such as obstructive jaundice and/or ureteral stenosis, which are sometimes developed with GI obstruction, only 2 patients required ureteral catheter insertion due to hydronephrosis before surgery, while no one had obstructive jaundice. All the patients suffered from poor oral intake requiring parenteral nutrition, and they showed various symptoms such as abdominal cramps, nausea, vomiting, anorexia, and abdominal distension. As for the number of non-curative factors, such as T4 tumor (tumor infiltrating to adjacent organs) deemed to be unresectable radically, para-aortic lymph node metastasis (N3), hepatic metastasis (H), peritoneal metastasis (P), and distant metastasis (M), 34 patients had a single non-curative factor and 19 patients had two or more. Serum C-reactive protein (CRP), serum albumin (Alb), and body mass index (BMI) were measured in all patients. Twenty-nine patients showed a normal range of CRP (≤0.3 mg/dl), while only 10 patients maintained a normal range of Alb (≥4.0 g/dl). Twenty-three patients presented with a reduced BMI value below normal (18.5–24.9 kg/m2). The types of surgery performed with palliative intent to manage symptoms caused by GI obstruction were as follows: gastrojejunostomy in 14 patients, small bowel bypass/colonic bypass in 17 patients, small bowel resection/colonic resection in 10 patients, ileostomy/colostomy in 17 patients, and catheter-ileostomy for decompressing obstructive intestine in 5 patients (some patients had more than one procedure simultaneously). No additional surgical intervention was performed in any patients.
QOL assessment
Postoperative improvement of oral intake, achievement of hospital discharge, and implementation of chemotherapy in each patient were estimated and these three parameters were used as a triad to assess the patient’s QOL.
Analyses of prognostic factors
The clinical course of each patient was followed until death. All the patients died during the observation period, which lasted until December 31, 2008. The survival time was defined as the duration from the date of surgical palliation to death. A univariate analysis was used to assess the association between each clinicopathological factor and overall survival (OS). A multivariate analysis was performed to identify variables independently associated with survival.
Evaluation of operative morbidity and mortality
Surgical and non-surgical complications were collected. Anastomotic leakage, abdominal abscess, pleural effusion, and pneumonia were diagnosed radiographically, based on clinical suspicion. Reoperation details and length of hospital stay were also recorded. Operative mortality was defined as postoperative death of any cause within 30 days of surgery, or during the same hospital stay.
Statistical analysis
SAS statistical software 5.0 (SAS Institute, Cary, NC, USA) was used for all statistical analyses and a P value of less than 0.05 was considered significant. The χ2 test was employed to evaluate differences in proportions. The survival rates were calculated according to the Kaplan–Meier method and difference was evaluated by the log-rank test. Cox’s proportional hazards regression model was used to identify prognostic factors for survival.
Results
Predictive factors for QOL improvement
Following the surgical palliations for GI obstruction, 40 of the 53 patients were eventually able to eat solid food without any need for parenteral nutrition and 42 patients were discharged from hospital, while 40 patients could receive chemotherapy. Distribution of the whole patient cohort for these three goals as an index of QOL improvement is shown in Fig. 1. Eventually, 64% (34/53) of the entire patient cohort demonstrated a QOL improvement by having achieved the triad, and 11% (6/53) could not obtain any kind of QOL improvement. When dividing the patients into two groups, 34 patients who achieved the triad and the other 19 patients who did not, the distribution of PS was significantly different between the two groups, as shown in Table 2. Patients with PS of 1 or less showed a good probability of obtaining an improvement of QOL through surgical palliation.
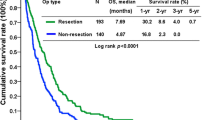
Overall survival (OS) and prognostic factors
The median survival time (MST) of the whole patient cohort following surgical palliation was 161 days, as shown in Fig. 2. In terms of a QOL improvement, the MST of patients fulfilling the triad was 253 days, while that in patients failing to achieve the triad was 60 days, with a significant difference between them (P < 0.0001), as shown in Fig. 3. The results of univariate and multivariate analyses of various clinicopathological factors, such as gender, age, PS, tumor status, number of non-curative factors, CRP, Alb, and BMI for OS are summarized in Table 3. Among these, PS of 1 or less [hazard ratio 0.265 (95% confidence interval [CI] 0.121–0.578)] and recurrent disease [hazard ratio 0.394 (95% CI 0.160–0.971)] were identified as significant independent prognostic factors for longer OS.
Operative morbidity and mortality
Postoperative complications were identified in 13 patients, and the overall morbidity rate was 24.5%, as shown in Table 4. Anastomotic leakage was observed in 1 patient after small bowel resection; this leakage persisted for 84 days until death. Four patients had an abdominal abscess, which occurred after small bowel resection in 1 patient and after colonic resection in the other 3 patients. Wound infection was comparatively more frequent, and occurred in 8 patients (15.1%). Pleural effusion developed in 4 patients, while neither pneumonia nor cardiac failure was observed in any patient. Reoperation was never performed. There were 11 hospital deaths (20.8%), all of which were caused by disease progression, not by postoperative complications; in particular, 7.5% (4/53) of patients died in the hospital within 30 days of the surgical procedure. The median hospital stay of all 53 patients was 31 (range 8–176) days.
Discussion
Although surgery provides the only possibility of cure in patients with AGC, some patients have incurable advanced disease associated with a poor prognosis of less than 1 year [2] at presentation. AGC can cause various symptoms, such as abdominal pain/distension, anorexia, weight loss, and nausea/vomiting [3], and the severity of these presentations ranges from mild and elective to severe and emergent. On occasion, patients suffer from poor oral intake, malnutrition, and ileus due to GI obstruction caused by advanced disease. Surgical palliation can be the treatment of choice in this situation to relieve the obstructive symptoms. Unfortunately, few data exist that define the specific indications for palliative surgery in the management of GI obstruction caused by AGC, as the most frequently cited tumors in the palliative surgical literature were esophageal, colorectal, pancreatic, and biliary cancers [5], and the palliative surgery decision is often made based on the combined experiences and impressions of the patient and surgeon. Therefore, in the present study, to elucidate the optimal indications for surgical palliation, in terms of improvement of QOL and survival, we retrospectively analyzed the outcomes of patients presenting with GI obstruction due to incurable AGC followed by palliative surgery.
QOL is an important outcome in patients undergoing surgery in general and oncologic palliative surgery in particular, because patients with incurable disease have a limited survival. The triad of solid food intake, hospital discharge, and chemotherapy implementation following surgical palliation was used as an index of improved QOL in the present study. Two-thirds of the whole patient cohort obtained a QOL improvement, and PS of 1 or less was a predictive factor for QOL improvement following surgical palliation. Palliative operative or endoscopic procedures were reported to relieve symptoms, such as GI obstruction, neurologic symptoms, pain, dyspnea, and jaundice, in 80% of patients with advanced cancer [6]. Similarly, in the present study, 89% of the patients accomplished at least one goal of the triad after palliative surgery.
Among the triad, improved oral intake and hospital discharge are clearly associated with QOL improvement and are generally accepted QOL indices. Implementation of chemotherapy following surgical palliation was also assessed as a parameter of QOL improvement in the present study, because chemotherapy is a widely accepted mainstay of palliative treatment, given its superiority over best supportive care with respect to the palliation of tumor-associated symptoms and prolongation of OS [7, 8]. Patients with improved QOL through the delivery of chemotherapy demonstrated prolonged survival, as shown in Fig. 3. Likewise, there has recently been increasing aggressiveness for delivering chemotherapy as end-of-life therapy, aiming at prolonged OS as well as improved QOL [9, 10].
In the present study, the MST of the whole patient cohort following surgical palliation was 161 days, which is similar to that of around 6 months reported in other palliative surgical literature [6, 11]. However, patients achieving the triad of a QOL improvement showed a longer MST, of 253 days, as shown in Fig. 3, which suggests that successful surgical palliation could have an impact on the survival of patients affected by incurable AGC causing GI obstruction. This prolonged survival was significantly associated with good PS of 1 or less and recurrent disease, as shown in Table 3.
Several studies have been undertaken in order to establish palliative prognostic indices or scores in terminally ill cancer patients [12, 13]. The survivals of terminally ill patients were found to be often overestimated by physicians in a large prospective cohort study [14], and against this background, we consider that prognostic factors are essential for planning optimal end-of-life treatment. In accordance with our findings, poor PS of 2 or more [6, 12, 15–17], and advanced disease with no prior history of cancer therapy [6] have been reported to correlate with poor prognosis in terminally ill cancer patients. Although the presence of multiple metastatic sites [16] and raised CRP level [17–20] were reported as valuable prognostic factors both in patients with advanced cancer and in palliative care patients, neither of these factors were prognostically significant in the present study, despite the short survival of the respective cohort. In addition, an association of decreased Alb level with poor prognosis was not demonstrated in this study, partly due to the comparatively well-maintained Alb level (median value of 3.5 g/dl) in our patients, though this association has been identified in the literature [3, 6, 13, 16, 19]. Even when the cut-off value of Alb was set at 3.0 g/dl or a prognostic nutritional index [PNI; 10 × Alb (g/dl) + 0.005 × lymphocyte counts (/mm3)] of 40 or less was used as an indicator of malnutrition in multivariate analysis, neither nutritional index was prognostically significant (P = 0.5433; hazard ratio = 1.370; 95% CI 0.497–3.779 for Alb, and P = 0.8741; hazard ratio = 0.948; 95% CI 0.490–1.835 for PNI). With respect to BMI, patients maintaining a BMI above normal showed diminished survival in the present study; this could be attributed to several factors, such as the presence of ascites and edema, which has been indicated as a negative prognostic factor [3, 12, 16]. Because of this unstable characteristic of BMI, it has not been assessed as a prognostic index in palliative care patients [3, 6, 16, 17]. As for the impact of the macroscopic type of primary GC (especially type 4), or the type of surgical procedure on the patients’ survival, neither factor affected the outcome. The MST for the 24 patients with type 4 GC was 251 days, while that for the remaining 29 patients with other types was 152 days, with no significant difference between them (P = 0.1516). Likewise, the MST for 11 patients who underwent gastrojejunostomy was 161 days, whereas the MST for 23 patients who received an intestinal resection/bypass was 202 days and that for 3 patients with gastrojejunostomy plus intestinal resection/bypass was 152 days, with no significant difference among them (P = 0.5367).
The potential benefits of surgical palliation can be minimized by postoperative complications. Although no one in the present study died from postoperative complications, 7.5% (4/53) of patients received no benefit from palliative surgery because they died in the hospital due to disease progression within 30 days of the surgical procedure. The 30-day postoperative mortality rate of 7.5% was in marked contrast to the 30-day operative mortality of 0.8% associated with elective curative-intent surgical oncology procedures for AGC in Japan [21]. In general, 30-day postoperative mortality rates of 11–12% and morbidity rates as high as 21–29% have been noted in the palliative surgery literature [6, 11]; these rates are consistent with our present findings. Postoperative morbidity can prolong the length of hospitalization and reduce the rate of symptom improvement [6]. However, in the present study, 79.2% (42/53) of the patients were discharged from hospital and 75.5% (40/53) of the patients showed restored solid food intake following surgical palliation, findings which reflect that less than 25% of the patients had a considerable negative influence from the surgical procedure.
With respect to a palliative role for endoscopic stenting, all the patients in the present study received surgical palliation rather than stent insertion because endoscopic stenting for GI obstruction, except for esophageal obstruction, has not been reimbursed by the Japanese national insurance system until recent days. For at least 6 patients presenting with gastric outlet obstruction caused by the primary unresectable GC, endoscopic stenting could have been an option. However, for patients with PS of 0–1 and those with recurrent disease, who have a relatively longer life expectancy based on our findings, surgical bypass is considered the preferred option because patients managed with stent insertion have a greater need for re-intervention, as a result of delayed stent occlusion, compared with surgically treated patients [22]. The decision on operative bypass versus endoscopic stenting should be made on a case-by-case basis, taking into account each patient’s life expectancy.
The appropriate indications of surgical palliation for incurable AGC presenting with GI obstruction are less clearly defined than those associated with curative therapy. The present study demonstrated that surgical palliation could be justified, in terms of improved QOL and prolonged survival, in patients with PS of 0-1 and those with recurrent disease. Owing to the retrospective nature of this study, which was performed in a single institution, and the relatively small size of the studied population, limitations of the present data need to be taken into account before the application of our results can be generalized in daily practice; for this we must wait until a prospective multicenter validation has been conducted. However, we believe that our findings will contribute to improving the ability of practitioners to prognosticate the course of disease more accurately and facilitate decision-making on the management of malignant GI obstruction caused by incurable AGC, and this will help both physicians and their patients, as well as their care-givers.
References
Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55:74–108.
Ohtsu A. Chemotherapy for metastatic gastric cancer: past, present, and future. J Gastroenterol. 2008;43:256–64.
Gencer D, Kastle-Larralde N, Pilz LR, Weiss A, Buchheidt D, Hochhaus A, et al. Presentation, treatment, and analysis of prognostic factors of terminally ill patients with gastrointestinal tumors. Onkologie. 2009;32:380–6.
McCahill LE, Krouse R, Chu D, Juarez G, Uman GC, Ferrell B, et al. Indications and use of palliative surgery–results of Society of Surgical Oncology survey. Ann Surg Oncol. 2002;9:104–12.
Miner TJ, Jaques DP, Tavaf-Motamen H, Shriver CD. Decision making on surgical palliation based on patient outcome data. Am J Surg. 1999;177:150–4.
Miner TJ, Brennan MF, Jaques DP. A prospective, symptom related, outcomes analysis of 1022 palliative procedures for advanced cancer. Ann Surg. 2004;240:719–27.
Glimelius B, Hoffman K, Haglund U, Nyrén O, Sjödén PO. Initial or delayed chemotherapy with best supportive care in advanced gastric cancer. Ann Oncol. 1994;5:189–90.
Pyrhönen S, Kuitunen T, Nyandoto P, Kouri M. Randomised comparison of fluorouracil, epidoxorubicin and methotrexate (FEMTX) plus supportive care with supportive care alone in patients with non-resectable gastric cancer. Br J Cancer. 1995;71:587–91.
Earle CC, Landrum MB, Souza JM, Neville BA, Weeks JC, Ayanian JZ. Aggressiveness of cancer care near the end of life: is it a quality-of-care issue? J Clin Oncol. 2008;26:3860–6.
Yun YH, Kwak M, Park SM, Kim S, Choi JS, Lim HY, et al. Chemotherapy use and associated factors among cancer patients near the end of life. Oncology. 2007;72:164–71.
Krouse RS, Nelson RA, Farrell BR, Grube B, Juarez G, Wagman LD, et al. Surgical palliation at a cancer center. Arch Surg. 2001;136:773–8.
Morita T, Tsunoda J, Inoue S, Chihara S. The palliative prognostic index: a scoring system for survival prediction of terminally ill cancer patients. Support Care Cancer. 1999;7:128–33.
Tassinari D, Montanari L, Maltoni M, Ballardini M, Piancastelli A, Musi M, et al. The palliative prognostic score and survival in patients with advanced solid tumors receiving chemotherapy. Support Care Cancer. 2008;16:359–70.
Christakis NA, Lamont EB. Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study. BMJ. 2000;320:469–72.
Maltoni M, Nanni O, Pirovano M, Scarpi E, Indelli M, Martini C, et al. Successful validation of the palliative prognostic score in terminally ill cancer patients. J Pain Symptom Manage. 1999;17:240–7.
Barbot AC, Mussault P, Ingrand P, Tourani JM. Assessing 2-month clinical prognosis in hospitalized patients with advanced solid tumors. J Clin Oncol. 2008;26:2538–43.
Maltoni M, Caraceni A, Brunelli C, Broeckaert B, Christakis N, Eychmueller S, et al. Prognostic factors in advanced cancer patients: evidence-based clinical recommendations—a study by the steering committee of the European Association for Palliative Care. J Clin Oncol. 2005;23:6240–8.
Kelly L, White S, Stone PC. The B12/CRP index as a simple prognostic indicator in patients with advanced cancer: a confirmatory study. Ann Oncol. 2007;18:1395–9.
Elahi MM, McMillan DC, McArdle CS, Angerson WJ, Sattar N. Score based on hypoalbuminemia and elevated C-reactive protein predicts survival in patients with advanced gastrointestinal cancer. Nutr Cancer. 2004;48:171–3.
Mahmoud FA, Rivera NI. The role of C-reactive protein as a prognostic indicator in advanced cancer. Curr Oncol Rep. 2002;4:250–5.
Sano T, Sasako M, Yamamoto S, Nashimoto A, Kurita A, Hiratsuka M, et al. Gastric cancer surgery: morbidity and mortality results from a prospective randomized controlled trial comparing D2 and extended para-aortic lymphadenectomy—Japan Clinical Oncology Group Study 9501. J Clin Oncol. 2004;22:2767–73.
Jeurnink SM, Steyerberg EW, Hof G, van Eijck CH, Kuipers EJ, Siersema PD. Gastrojejunostomy versus stent placement in patients with malignant gastric outlet obstruction: a comparison in 95 patients. J Surg Oncol. 2007;96:389–96.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fujitani, K., Yamada, M., Hirao, M. et al. Optimal indications of surgical palliation for incurable advanced gastric cancer presenting with malignant gastrointestinal obstruction. Gastric Cancer 14, 353–359 (2011). https://doi.org/10.1007/s10120-011-0053-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10120-011-0053-1