Abstract
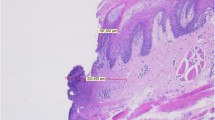
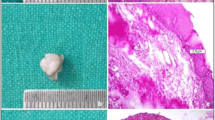
The objective of this study was to describe the histological artifacts caused by high-power laser use compared to cold scalpel surgery in oral soft tissue lesions. Clinical studies that evaluated and compared histological artifacts resulting from the use of high-power lasers and cold scalpels in oral soft tissue lesions biopsies were retrieved from seven databases and four grey literatures, up to July 2022. The risk of bias was investigated using the ROBINS-I tool. The certainty of the evidence was assessed using the Grading of Recommendations, Assessment, Development, and Evaluation approach. Seven studies were eligible for qualitative analysis. Based on the results obtained, those four studies had a low risk of bias, and three studies had an unclear risk of bias. The certainty of the evidence was classified as low. Limited evidence showed that epithelial artifacts such as loss of intraepithelial and subepithelial adhesions, accompanied by pyknotic, fusiform, and/or hyperchromic nuclei, were more common when a high-power laser device was used. Four articles reported that the use of high-power lasers did not interfere with the histopathological diagnosis of oral soft tissue lesions. Due to the heterogeneity of the data, a meta-analysis was not performed. Compared to the use of cold scalpels, histological artifacts, particularly those observed in epithelial tissue, are more common when high-powered lasers are used in oral lesions biopsies. The eligibility criteria and adequate indications of high-power lasers in different oral soft tissue lesion treatments must be respected to avoid tissue artifacts that impair precise histopathological diagnosis.


Similar content being viewed by others
Data Availability
All data supporting the results reported in this work can be accessed through the DOI provided in the references section.
References
Cercadillo-Ibarguren I, España-Tost A, Arnabat-Domínguez J, Valmaseda-Castellón E, Berini-Aytés L, Gay-Escoda C (2010) Histologic evaluation of thermal damage produced on soft tissues by CO2, Er,Cr:YSGG and diode lasers. Med Oral Patol Oral Cir Bucal 15. https://doi.org/10.4317/MEDORAL.15.E912
Jin JY, Lee SH, Yoon HJ (2010) A comparative study of wound healing following incision with a scalpel, diode laser or Er,Cr:YSGG laser in guinea pig oral mucosa: a histological and immunohistochemical analysis. Acta Odontol Scand 68:232–238. https://doi.org/10.3109/00016357.2010.492356
Monteiro L, Delgado ML, Garcês F, Machado M, Ferreira F, Martins M, Salazar F, Pacheco JJ (2019) A histological evaluation of the surgical margins from human oral fibrous-epithelial lesions excised with CO2 laser, Diode laser, Er:YAG laser, Nd:YAG laser, electrosurgical scalpel and cold scalpel. Med Oral Patol Oral Cir Bucal 24:e271–e280. https://doi.org/10.4317/MEDORAL.22819
Suter VGA, Altermatt HJ, Bornstein MM (2020) A randomized controlled trial comparing surgical excisional biopsies using CO 2 laser, Er:YAG laser and scalpel. Int J Oral Maxillofac Surg 49:99–106. https://doi.org/10.1016/J.IJOM.2019.05.012
Romeo U, Libotte F, Palaia G, del Vecchio A, Tenore G, Visca P, Nammour S, Polimeni A (2012) Histological in vitro evaluation of the effects of Er:YAG laser on oral soft tissues. Lasers Med Sci 27:749–753. https://doi.org/10.1007/S10103-011-0969-Z
Bhatsange A, Meshram EP, Waghamare A, Shiggaon L, Mehetre V, Shende A (2016) A clinical and histological comparison of mucosal incisions produced by scalpel, electrocautery, and diode laser: a pilot study. J Dental Lasers 10:37. https://doi.org/10.4103/2321-1385.196962
Angiero F, Parma L, Crippa R, Benedicenti S (2012) Diode laser (808 nm) applied to oral soft tissue lesions: a retrospective study to assess histopathological diagnosis and evaluate physical damage. Lasers Med Sci 27:383–388. https://doi.org/10.1007/S10103-011-0900-7
Gill K, Sandhu SV, Sethi N, Bhandari R (2021) Biopsy of oral soft tissue lesions by 808 nm and 980 nm diode laser: a morphological and histochemical evaluation. Lasers Dent Sci 5:207–222. https://doi.org/10.1007/S41547-021-00132-Z/FIGURES/6
Eversole LR (1997) Laser artifacts and diagnostic biopsy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 83:639–640. https://doi.org/10.1016/s1079-2104(97)90308-5
Lopes-Santos G, da Silva Santos PS, Oliveira DT (2023) Cytological artifacts mimicking vulgar pemphigus caused by diode laser surgery in oral lesion. Int J Surg Pathol 31(7):1323–1325. https://doi.org/10.1177/10668969221143482
Merigo E, Clini F, Fornaini C, Oppici A, Paties C, Zangrandi A, Fontana M, Rocca JP, Meleti M, Manfredi M, Cella L, Vescovi P (2013) Laser-assisted surgery with different wavelengths: a preliminary ex vivo study on thermal increase and histological evaluation. Lasers Med Sci 28:497–504. https://doi.org/10.1007/S10103-012-1081-8
Parker S (2007) Lasers and soft tissue: “loose” soft tissue surgery. Br Dental J 202(4):185–191. https://doi.org/10.1038/bdj.2007.128
Azevedo AS, Monteiro LS, Ferreira F, Delgado ML, Garcês F, Carreira S, Martins M, Suarez-Quintanilla J (2016) In vitro histological evaluation of the surgical margins made by different laser wavelengths in tongue tissues. J Clin Exp Dent 8:e388. https://doi.org/10.4317/JCED.52830
Seoane J, Caballero TG, Urizar JMA, Almagro M, Mosquera AG, Varela-Centelles P (2010) Pseudodysplastic epithelial artefacts associated with oral mucosa CO2 laser excision: an assessment of margin status. Int J Oral Maxillofac Surg 39:783–787. https://doi.org/10.1016/J.IJOM.2010.04.046
Seoane J, González-Mosquera A, García-Martín JM, García-Caballero L, Seoane-Romero JM, Varela-Centelles P (2015) Pseudoepitheliomatous hyperplasia after diode laser oral surgery. An experimental study. Med Oral Patol Oral Cir Bucal 20:e554. https://doi.org/10.4317/MEDORAL.20519
Vescovi P, Corcione L, Meleti M, Merigo E, Fornaini C, Manfredi M, Bonanini M, Govoni P, Rocca JP, Nammour S (2010) Nd:YAG laser versus traditional scalpel. A preliminary histological analysis of specimens from the human oral mucosa. Lasers Med Sci 25:685–691. https://doi.org/10.1007/S10103-010-0770-4
Capodiferro S, Loiudice AM, Pilolli G, Lajolo C, Giuliani M, Maiorano E, Favia G (2009) Diode laser excision of chondroid lipoma of the tongue with microscopic (conventional and confocal laser scanning) analysis. Photomed Laser Surg 27:683–687. https://doi.org/10.1089/PHO.2008.2359
Romeo U, Russo C, Palaia G, Giudice RL, del Vecchio A, Visca P, Migliau G, de Biase A (2014) Biopsy of different oral soft tissues lesions by KTP and diode laser: histological evaluation. Sci World J 2014. https://doi.org/10.1155/2014/761704
Amaral MBF, de Ávila JMS, Abreu MHG, Mesquita RA (2015) Diode laser surgery versus scalpel surgery in the treatment of fibrous hyperplasia: a randomized clinical trial. Int J Oral Maxillofac Surg 44:1383–1389. https://doi.org/10.1016/J.IJOM.2015.05.015
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372. https://doi.org/10.1136/BMJ.N71
Broccoletti R, Cafaro A, Gambino A, Romagnoli E, Arduino PG (2015) Er:YAG laser versus cold knife excision in the treatment of nondysplastic oral lesions: a randomized comparative study for the postoperative period. Photomed Laser Surg 33:604–609. https://doi.org/10.1089/PHO.2015.3967
Isola G, Matarese G, Cervino G, Matarese M, Ramaglia L, Cicciù M (2018) Clinical efficacy and patient perceptions of pyogenic granuloma excision using diode laser versus conventional surgical techniques. J Craniofac Surg 29:2160–2163. https://doi.org/10.1097/SCS.0000000000004734
Monteiro L, Barbieri C, Warnakulasuriya S, Martins M, Salazar F, Pacheco JJ, Vescovi P, Meleti M (2017) Type of surgical treatment and recurrence of oral leukoplakia: a retrospective clinical study. Med Oral Patol Oral Cir Bucal 22:e520–e526. https://doi.org/10.4317/MEDORAL.21645
Syed TF, Thukral N (2009) CO2 laser surgery for the excision of leukoplakia: a comparison with the traditional technique. He J Oral Laser Appl:213–2018 http://www.quintpub.com/journals/jola/abstract.php?iss2_id=723&article_id=8597&article=4#.Yv0tgHbMJMw (accessed August 16, 2022)
Vu J, Coleman HG, Palme CE, Riffat F, Schifter M, Zoellner H (2019) Diagnostic utility of microsurgical carbon dioxide laser excision of oral potentially malignant lesions vs incisional biopsy: a retrospective histopathological review. Oral Surg Oral Med Oral Pathol Oral Radiol 127:516–525. https://doi.org/10.1016/J.OOOO.2018.12.010
Yagüe-García J, España-Tost A-J, Berini-Aytés L, Gay-Escoda O (2009) Treatment of oral mucocele-scalpel versus CO2 laser. Med Oral Patol Oral Cir Bucal 14:469–474. https://doi.org/10.1016/j.kjms.2010.09.006
Barbieri C, Monteiro L, Meleti M, Merigo E, Manfredi M, Fornaini C, Vescovi P (2013) Laser vs. quantic molecular resonance surgery of oral leukoplakia: histomorphometrical compared analysis of surgical margins. Lasers Med Sci 28:1405–1433. https://doi.org/10.1007/S10103-013-1431-1
Tuncer I, Ozçakir-Tomruk C, Sencift K, Cöloǧlu S (2010) Comparison of conventional surgery and CO2 laser on intraoral soft tissue pathologies and evaluation of the collateral thermal damage. Photomed Laser Surg 28:75–79. https://doi.org/10.1089/PHO.2008.2353
Palaia G, Impellizzeri A, Tenore G, Caporali F, Visca P, del Vecchio A, Galluccio G, Polimeni A, Romeo U (2020) Ex vivo histological analysis of the thermal effects created by a 445-nm diode laser in oral soft tissue biopsy. Clin Oral Investig 24:2645–2652. https://doi.org/10.1007/S00784-019-03123-4/FIGURES/9
Tenore G, Mohsen A, Nuvoli A, Palaia G, Rocchetti F, Rosaria C, di Gioia T, Cicconetti A, Romeo U, del Vecchio A (2023) The impact of laser thermal effect on histological evaluation of oral soft tissue biopsy: systematic review. Dent J 11:28. https://doi.org/10.3390/DJ11020028
Chatterjee S (2014) Artefacts in histopathology. J Oral Maxillofac Pathol 18:S111. https://doi.org/10.4103/0973-029X.141346
Romeo U, Mohsen M, Palaia G, Bellisario A, del Vecchio A, Tenore G (2020) CO2 laser ablation of oral leukoplakia: with or without extension of margins? Clin Ter 171:E209–E215. https://doi.org/10.7417/CT.2020.2215
Vilar-Villanueva M, Somoza-Martín JM, Blanco-Carrión A, García-García A, García-Carnicero T, Marichalar-Mendía X, Gallas-Torreira M, Gándara-Vila P (2022) Importance of the vaporization margin during CO2 laser treatment of oral leukoplakia: a survival study. Oral Dis. https://doi.org/10.1111/ODI.14345
Montebugnoli L, Frini F, Gissi DB, Gabusi A, Cervellati F, Foschini MP, Marchetti C (2012) Histological and immunohistochemical evaluation of new epithelium after removal of oral leukoplakia with Nd:YAG laser treatment. Lasers Med Sci 27:205–210. https://doi.org/10.1007/S10103-011-0941-Y
Romeo U, Palaia G, del Vecchio A, Tenore G, Gambarini G, Gutknecht N, de Luca M (2010) Effects of KTP laser on oral soft tissues. an in vitro study. Lasers Med Sci 25:539–543. https://doi.org/10.1007/S10103-010-0756-2
Gundlapalle P, Nagappan N, Ramesh P, Ziauddhin S, Karthick BP, Paleti VSM, Kumar BV (2022) Comparison of oral mucosal biopsies done using scalpel and diode lasers: a vivo study. J Pharm Bioallied Sci 14:S947–S954. https://doi.org/10.4103/jpbs.jpbs_861_21
Funding
This work was supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES—code 001).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
Supplementary Table 1 - Database Search strategy (DOCX 26 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lopes-Santos, G., Peralta-Mamani, M. & Oliveira, D.T. Histological implications of high-power laser use in the oral soft tissue lesions: a systematic review. Lasers Med Sci 38, 263 (2023). https://doi.org/10.1007/s10103-023-03923-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-023-03923-x