Abstract
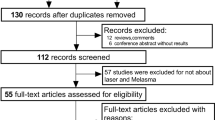
Multiple laser modalities have been used for melasma treatment. However, the effectiveness of picosecond laser in treating melasma remains unclear. This meta-analysis investigated the effectiveness and safety of picosecond laser for melasma treatment. Randomized controlled trials (RCTs) comparing picosecond laser with conventional treatment for melasma were searched through five databases. The melasma area severity index (MASI)/modified MASI (mMASI) was used to quantify the degree of melasma improvement. Standardized mean differences and 95% confidence intervals were calculated using Review Manager for result standardization. Six RCTs, which used picosecond laser at 1064, 755, 595, and 532 nm wavelengths, were included herein. Picosecond laser significantly reduced the MASI/mMASI, but the results were highly heterogeneous (P = 0.008, I2 = 70%). In the subgroup analysis of 1064 and 755 nm picosecond lasers, 1064 nm picosecond laser significantly reduced the MASI/mMASI with no significant side effects (P = 0.04). Meanwhile, 755 nm picosecond laser did not significantly improve the MASI/mMASI compared with topical hypopigmentation agents (P = 0.08) and caused post-inflammatory hyperpigmentation. Other laser wavelengths could not be used in the subgroup analysis owing to an insufficient sample size. Picosecond laser at 1064 nm is safe and effective for melasma treatment. Picosecond laser at 755 nm is not superior to topical hypopigmentation agents in treating melasma. The exact efficacy of other wavelengths of picosecond laser for melasma treatment remains to be verified in large-scale RCTs.




Similar content being viewed by others
References
Kwon S, Park K (2014) Melasma and common pigmentary dermatoses in Asian individuals and an overview of their treatment. J Clin Investigat Dermatol 2(1):8
Pichardo R, Vallejos Q, Feldman SR et al (2009) The prevalence of melasma and its association with quality of life in adult male Latino migrant workers. Int J Dermatol 48(1):22–26
Zhang L, Tan W-Q, Fang Q-Q et al (2018) Tranexamic acid for adults with melasma: a systematic review and meta-analysis. Biomed Res Int 2018
Ogbechie-Godec OA, Elbuluk N (2017) Melasma: an up-to-date comprehensive review. Dermatol Ther (Heidelb) 7(3):305–318
Nautiyal A, Wairkar S (2021) Management of hyperpigmentation: current treatments and emerging therapies. Pigment Cell Melanoma Res 34(6):1000–1014
Cho HH, Choi M, Cho S et al (2013) Role of oral tranexamic acid in melasma patients treated with IPL and low fluence QS Nd: YAG laser. J Dermatolog Treat 24(4):292–296
Zhang B, Xie B, Shen Y et al (2022) Single and combined 1064 nm Q-switched Nd: YAG laser therapy in melasma: a meta-analysis. J Cosmet Dermatol 21(9):3794–3802
Trivedi M, Yang F, Cho B (2017) A review of laser and light therapy in melasma. Int J Womens Dermatol 3(1):11–20
Passeron T, Picardo M (2018) Melasma, a photoaging disorder. Pigment Cell Melanoma Res 31(4):461–465
Freedman JR, Kaufman J, Metelitsa AI et al (2014) Picosecond lasers: the next generation of short-pulsed lasers. Semin Cutan Med Surg 33(4):164–168
Tanghetti EA (2016) The histology of skin treated with a picosecond alexandrite laser and a fractional lens array. Lasers Surg Med 48(7):646–652
Higgins JP, Thomas J, Chandler J et al (2019) Cochrane handbook for systematic reviews of interventions. John Wiley & Sons
Wang YJ, Lin ET, Chen YT et al (2020) Prospective randomized controlled trial comparing treatment efficacy and tolerance of picosecond alexandrite laser with a diffractive lens array and triple combination cream in female Asian patients with melasma. J Eur Acad Dermatol Venereol 34(3):624–632
Manuskiatti W, Yan C, Gulfan MCB et al (2022) Combination of a 755-nm picosecond laser and hydroquinone 2% cream versus hydroquinone 2% cream alone for the treatment of melasma: a randomized, split-face, and controlled trial. Lasers Surg Med 54(10):1245–1250
Chalermchai T, Rummaneethorn P (2018) Effects of a fractional picosecond 1,064 nm laser for the treatment of dermal and mixed type melasma. J Cosmet Laser Ther 20(3):134–139
Choi YJ, Nam JH, Kim JY et al (2017) Efficacy and safety of a novel picosecond laser using combination of 1 064 and 595 nm on patients with melasma: a prospective, randomized, multicenter, split-face, 2% hydroquinone cream-controlled clinical trial. Lasers Surg Med 49(10):899–907
Hong JK, Shin SH, Park SJ et al (2022) A prospective, split-face study comparing 1,064-nm picosecond Nd: YAG laser toning with 1,064-nm Q-switched Nd: YAG laser toning in the treatment of melasma. J Dermatolog Treat:1–7
Naseemullah AQK, Khan FA, Awan SR et al (2022) Efficacy of 2% kojic acid containing formulation vs picosecond laser for treatment of melasma. Pak J Med Sci 16(10):368–368
Pandya AG, Hynan LS, Bhore R et al (2011) Reliability assessment and validation of the melasma area and severity index (MASI) and a new modified MASI scoring method. J Am Acad Dermatol 64(1):78–83
Haimovic A, Brauer JA, Bae Y-SC et al (2016) Safety of a picosecond laser with diffractive lens array (DLA) in the treatment of Fitzpatrick skin types IV to VI: a retrospective review. J Am Acad Dermatol 74(5):931–936
Goldberg D, Metzler C (1999) Skin resurfacing utilizing a low-fluence Nd: YAG laser. J Cutan Laser Ther 1(1):23–27
Grimes PE, Yamada N, Bhawan J (2005) Light microscopic, immunohistochemical, and ultrastructural alterations in patients with melasma. Am J Dermatopathol 27(2):96–101
Hai L, Phuong B, Ha L et al (2021) Dual toning method with the combination of picosecond and microsecond Nd: YAG in refractory melasma unresponsive to picosecond alone. J Cutan Aesthet Surg 14(1):101
Al Jaff MYS, Yawar FJ (2021) Treatment of melasma in Fitzpatrick skin type III and IV by picosecond laser. J Med Surg Pract (JMSP) 7(2):162–171
Wong CSM, Chan MWM, Shek SYN et al (2021) Fractional 1064 nm picosecond laser in treatment of melasma and skin rejuvenation in Asians, a prospective study. Lasers Surg Med 53(8):1032–1042
Chen Y-T, Lin E-T, Chang C-C et al (2019) Efficacy and safety evaluation of picosecond alexandrite laser with a diffractive lens array for treatment of melasma in Asian patients by VISIA imaging system. Photobiomodul Photomed Laser Surg 37(9):559–566
Polnikorn N, Tanghetti E (2020) Treatment of refractory melasma in Asians with the picosecond alexandrite laser. Dermatol Surg 46(12):1651–1656
Funding
This study received financial support from the Hangzhou Medical Key Discipline Construction Project (no. [2021]21-3).
Author information
Authors and Affiliations
Contributions
Jiangfeng Feng: data curation, formal analysis, writing — original draft. Sihao Shen: software. Xiuzu Song: validation. Wenzhong Xiang: methodology, writing — review and editing.
Corresponding author
Ethics declarations
Ethics approval
This research did not include any human subjects.
Informed consent
None.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Feng, J., Shen, S., Song, X. et al. Efficacy and safety of picosecond laser for the treatment of melasma: a systematic review and meta-analysis. Lasers Med Sci 38, 84 (2023). https://doi.org/10.1007/s10103-023-03744-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10103-023-03744-y