Abstract
Purpose
To evaluate the safety and efficacy of an at-home photobiomodulation (PBM) device for the treatment of diabetic foot ulcers (DFUs) in a frail population with severe comorbidities.
Methods
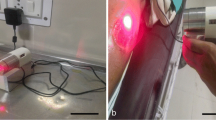
Prospective, randomized, double-blind, sham-controlled pilot study. Patients (age = 63 ± 11 years, male:female 13:7) with insulin-dependent diabetes type 2, neuropathy, peripheral artery disease, significant co-morbidities, and large osteomyelitis-associated DFUs (University of Texas grade ≥ III) were randomized to receive active (n = 10) or sham (n = 10) at-home daily PBM treatments (pulsed near-infrared 808 nm Ga-Al-As laser, 250 mW, 8.8 J/cm2) for up to 12 weeks in addition to standard care. The primary outcome was the %wound size reduction. The secondary was adverse events.
Results
With the numbers available, PBM-treated group had significantly greater %reduction compared to sham (area [cm2], baseline vs endpoint: PBM 10[20.3] cm2 vs 0.2[2.4] cm2; sham, 7.9 [12.0] cm2 vs 4.6 [13.8] cm2, p = 0.018 by Mann–Whitney U test). Wound closure > 90% occurred in 7 of 10 PBM-treated patients but in only 1 of 10 sham patients (p = 0.006). No adverse device effects were observed.
Conclusions
Photobiomodulation at home, in addition to standard care, may be effective for the treatment of severe DFUs in frail patients with co-morbidities and is particularly relevant at these times of social distancing. Our preliminary results justify the conduction of a larger clinical trial. ClinicalTrials.gov: NCT01493895.


Similar content being viewed by others
Code availability
Not applicable.
References
Armstrong DG, Boulton AJM, Bus SA (2017) Diabetic foot ulcers and their recurrence. N Engl J Med 376(24):2367–2375. https://doi.org/10.1056/NEJMra1615439
Thorud JC, Plemmons B, Buckley CJ, Shibuya N, Jupiter DC (2016) Mortality after nontraumatic major amputation among patients with diabetes and peripheral vascular disease: a systematic review. J Foot Ankle Surg 55(3):591–599. https://doi.org/10.1053/j.jfas.2016.01.012
Jeffcoate WJ, Vileikyte L, Boyko EJ, Armstrong DG, Boulton AJM (2018) Current challenges and opportunities in the prevention and management of diabetic foot ulcers. Diabetes Care 41(4):645–652. https://doi.org/10.2337/dc17-1836
Everett E, Mathioudakis N (2018) Update on management of diabetic foot ulcers. Ann N Y Acad Sci 1411(1):153–165. https://doi.org/10.1111/nyas.13569
Tchanque-Fossuo CN, Ho D, Dahle SE, Koo E, Isseroff RR, Jagdeo J (2016) Low-level light therapy for treatment of diabetic foot ulcer: a review of clinical experiences. J Drugs Dermatol 15(7):843–848
Chung H, Dai T, Sharma SK, Huang YY, Carroll JD, Hamblin MR (2012) The nuts and bolts of low-level laser (light) therapy. Ann Biomed Eng 40(2):516–533. https://doi.org/10.1007/s10439-011-0454-7
Anders JJ, Lanzafame RJ, Arany PR (2015) Low-level light/laser therapy versus photobiomodulation therapy. Photomed Laser Surg 33(4):183–184. https://doi.org/10.1089/pho.2015.9848
Gavish L (2013) Chapter 50: Low-Level laser therapy for wound healing. In: Hamblin M, Huang Y (eds) Handbook of Photomedicine. Boca Raton: CRC Press.,
Houreld NN (2014) Shedding light on a new treatment for diabetic wound healing: a review on phototherapy. ScientificWorldJournal 2014:398412. https://doi.org/10.1155/2014/398412
Carvalho AF, Feitosa MC, Coelho NP, Rebelo VC, Castro JG, Sousa PR, Feitosa VC, Arisawa EA (2016) Low-level laser therapy and Calendula officinalis in repairing diabetic foot ulcers. Rev Esc Enferm USP 50(4):628–634. https://doi.org/10.1590/S0080-623420160000500013
El-Kader S, M., Ashmawy E, M. (2015) Impact of different therapeutic modalities on healing of diabetic foot ulcers. Eur J Gen Med 12(4):319–325
Feitosa MC, Carvalho AF, Feitosa VC, Coelho IM, Oliveira RA, Arisawa EA (2015) Effects of the low-level laser therapy (LLLT) in the process of healing diabetic foot ulcers. Acta Cir Bras 30(12):852–857. https://doi.org/10.1590/S0102-865020150120000010
Mathur RK, Sahu K, Saraf S, Patheja P, Khan F, Gupta PK (2017) Low-level laser therapy as an adjunct to conventional therapy in the treatment of diabetic foot ulcers. Lasers Med Sci 32(2):275–282. https://doi.org/10.1007/s10103-016-2109-2
Ortíz MCS, Villabona EH, Lemos DMC, Castellanos R (2014) Effects of low level laser therapy and high voltage stimulation on diabetic wound healing. Rev Univ Ind Santander Salud [online] 46(2):107–117
Frangez I, Nizic-Kos T, Frangez HB (2018) Phototherapy with LED shows promising results in healing chronic wounds in diabetes mellitus patients: a prospective randomized double-blind study. Photomed Laser Surg 36(7):377–382. https://doi.org/10.1089/pho.2017.4382
Priyadarshini LMJ, Babu KEP, Thariq IA (2018) Effect of low level laser therapy on diabetic foot ulcers: a randomized control trial. Int Surg J 5(3):1008–1015
Sangma MB, Selvaraju S, Marak F, Dasiah SD (2019) Efficacy of low level infrared light therapy on wound healing in patients with chronic diabetic foot ulcers: a randomised control trial. Int Surg J 6(5):1650–1653
Flanagan M (2003) Wound measurement can it help us to monitor progression to healing? J Wound Care 12(5):189–194. https://doi.org/10.12968/jowc.2003.12.5.26493
Kajagar BM, Godhi AS, Pandit A, Khatri S (2012) Efficacy of low level laser therapy on wound healing in patients with chronic diabetic foot ulcers-a randomised control trial. Indian J Surg 74(5):359–363. https://doi.org/10.1007/s12262-011-0393-4
Kaviani A, Djavid GE, Ataie-Fashtami L, Fateh M, Ghodsi M, Salami M, Zand N, Kashef N, Larijani B (2011) A randomized clinical trial on the effect of low-level laser therapy on chronic diabetic foot wound healing: a preliminary report. Photomed Laser Surg 29(2):109–114. https://doi.org/10.1089/pho.2009.2680
Landau Z, Migdal M, Lipovsky A, Lubart R (2011) Visible light-induced healing of diabetic or venous foot ulcers: a placebo-controlled double-blind study. Photomed Laser Surg 29(6):399–404. https://doi.org/10.1089/pho.2010.2858
Minatel DG, Frade MA, Franca SC, Enwemeka CS (2009) Phototherapy promotes healing of chronic diabetic leg ulcers that failed to respond to other therapies. Lasers Surg Med 41(6):433–441. https://doi.org/10.1002/lsm.20789
Maiya AG, Kumar AS, Hazari A, Jadhav R, Ramachandra L, Hande HM, Rajgopal SK, Maiya SG, Kalkura P, Keni LG (2018) Photobiomodulation therapy in neuroischaemic diabetic foot ulcers a novel method of limb salvage. J Wound Care 27(12):837–842. https://doi.org/10.12968/jowc.2018.27.12.837
Del Vecchio A, Floravanti M, Boccassini A, Gaimari G, Vestri A, Di Paolo C, Romeo U (2019) Evaluation of the efficacy of a new low-level laser therapy home protocol in the treatment of temporomandibular joint disorder-related pain: a randomized, double-blind, placebo-controlled clinical trial. Cranio:1–10. https://doi.org/10.1080/08869634.2019.1599174
Fornaini C, Pelosi A, Queirolo V, Vescovi P, Merigo E (2015) The “at-home LLLT” in temporo-mandibular disorders pain control: a pilot study. Laser therapy 24(1):47–52. https://doi.org/10.5978/islsm.15-OR-06
Merigo E, Rocca JP, Oppici A, Cella L, Fornaini C (2017) At-home laser treatment of oral neuronal disorders: Case reports. J Clin Exp Dent 9(4):e595–e598. https://doi.org/10.4317/jced.53373
Gavish L, Houreld NN (2019) Therapeutic efficacy of home-use photobiomodulation devices: a systematic literature review. Photobiomodul Photomed Laser Surg 37(1):4–16. https://doi.org/10.1089/photob.2018.4512
Raizman R, Gavish L (2020) At-home self-applied photobiomodulation device for the treatment of diabetic foot ulcers in adults with type 2 diabetes: report of 4 cases. Can J Diabetes 44(5):375–378. https://doi.org/10.1016/j.jcjd.2020.01.010
Merigo E, Tan L, Zhao Z, Rocca J-P, Fornaini C (2020) Auto-administered photobiomodulation on diabetic leg ulcers treatment: a new way to manage it? Case Rep Med 2020:7428472. https://doi.org/10.1155/2020/7428472
Davis FM, Kimball A, Boniakowski A, Gallagher K (2018) Dysfunctional wound healing in diabetic foot ulcers: new crossroads. Curr Diab Rep 18(1):2. https://doi.org/10.1007/s11892-018-0970-z
Buys AV, Van Rooy MJ, Soma P, Van Papendorp D, Lipinski B, Pretorius E (2013) Changes in red blood cell membrane structure in type 2 diabetes: a scanning electron and atomic force microscopy study. Cardiovasc Diabetol 12:25. https://doi.org/10.1186/1475-2840-12-25
Ziegler O, Guerci B, Muller S, Candiloros H, Mejean L, Donner M, Stoltz JF, Drouin P (1994) Increased erythrocyte aggregation in insulin-dependent diabetes mellitus and its relationship to plasma factors: a multivariate analysis. Metabolism 43(9):1182–1186. https://doi.org/10.1016/0026-0495(94)90063-9
Singh M, Shin S (2009) Changes in erythrocyte aggregation and deformability in diabetes mellitus: a brief review. Indian J Exp Biol 47(1):7–15
Schindl A, Merwald H, Schindl L, Kaun C, Wojta J (2003) Direct stimulatory effect of low-intensity 670 nm laser irradiation on human endothelial cell proliferation. Br J Dermatol 148(2):334–336
Chen CH, Hung HS, Hsu SH (2008) Low-energy laser irradiation increases endothelial cell proliferation, migration, and eNOS gene expression possibly via PI3K signal pathway. Lasers Surg Med 40(1):46–54
Kipshidze N, Nikolaychik V, Keelan MH, Shankar LR, Khanna A, Kornowski R, Leon M, Moses J (2001) Low-power helium: neon laser irradiation enhances production of vascular endothelial growth factor and promotes growth of endothelial cells in vitro. Lasers Surg Med 28(4):355–364
Gavish L, Perez L, Gertz SD (2006) Low-level laser irradiation modulates matrix metalloproteinase activity and gene expression in porcine aortic smooth muscle cells. Lasers Surg Med 38(8):779–786. https://doi.org/10.1002/lsm.20383
Hawkins D, Abrahamse H (2006) Effect of multiple exposures of low-level laser therapy on the cellular responses of wounded human skin fibroblasts. Photomed Laser Surg 24(6):705–714. https://doi.org/10.1089/pho.2006.24.705
Houreld N, Abrahamse H (2007) Irradiation with a 632.8 nm helium-neon laser with 5 J/cm2 stimulates proliferation and expression of interleukin-6 in diabetic wounded fibroblast cells. Diabetes Technol Ther 9(5):451–459
Tuby H, Maltz L, Oron U (2006) Modulations of VEGF and iNOS in the rat heart by low level laser therapy are associated with cardioprotection and enhanced angiogenesis. Lasers Surg Med 38(7):682–688. https://doi.org/10.1002/lsm.20377
Gavish L, Perez LS, Reissman P, Gertz SD (2008) Irradiation with 780 nm diode laser attenuates inflammatory cytokines but upregulates nitric oxide in lipopolysaccharide-stimulated macrophages: implications for the prevention of aneurysm progression. Lasers Surg Med 40(5):371–378. https://doi.org/10.1002/lsm.20635
Bagheri M, Amini A, Abdollahifar MA, Ghoreishi SK, Piryaei A, Pouriran R, Chien S, Dadras S, Rezaei F, Bayat M (2018) Effects of photobiomodulation on degranulation and number of mast cells and wound strength in skin wound healing of streptozotocin-induced diabetic rats. Photomed Laser Surg 36(8):415–423. https://doi.org/10.1089/pho.2018.4453
Kilik R, Lakyova L, Sabo J, Kruzliak P, Lacjakova K, Vasilenko T, Vidova M, Longauer F, Radonak J (2014) Effect of equal daily doses achieved by different power densities of low-level laser therapy at 635 nm on open skin wound healing in normal and diabetic rats. Biomed Res Int 2014:269253. https://doi.org/10.1155/2014/269253
Mi XQ, Chen JY, Liang ZJ, Zhou LW (2004) In vitro effects of helium-neon laser irradiation on human blood: blood viscosity and deformability of erythrocytes. Photomed Laser Surg 22(6):477–482. https://doi.org/10.1089/pho.2004.22.477
Keszler A, Lindemer B, Weihrauch D, Jones D, Hogg N, Lohr NL (2017) Red/near infrared light stimulates release of an endothelium dependent vasodilator and rescues vascular dysfunction in a diabetes model. Free Radic Biol Med 113:157–164. https://doi.org/10.1016/j.freeradbiomed.2017.09.012
Santos NR, dos Santos JN, dos Reis JA, Jr., Oliveira PC, de Sousa AP, de Carvalho CM, Soares LG, Marques AM, Pinheiro AL, (2010) Influence of the use of laser phototherapy (lambda660 or 790 nm) on the survival of cutaneous flaps on diabetic rats. Photomed Laser Surg 28(4):483–488. https://doi.org/10.1089/pho.2009.2500
Gavish L, Hoffer O, Rabin N, Halak M, Shkilevich S, Shayovitz Y, Weizman G, Haim O, Gavish B, Gertz SD, Ovadia-Blechman Z (2020) Microcirculatory response to photobiomodulation – why some respond and others do not: a randomised controlled study. Lasers Surg Med 52(9):863–872
Samoilova KA, Zhevago NA, Petrishchev NN, Zimin AA (2008) Role of nitric oxide in the visible light induced rapid increase of human skin microcirculation at the local and systemic levels II healthy volunteers. Photomed Laser Surg 26(5):443–449. https://doi.org/10.1089/pho.2007.2205
Samoilova KA, Zhevago NA, Menshutina MA, Grigorieva NB (2008) Role of nitric oxide in the visible light induced rapid increase of human skin microcirculation at the local and systemic level I diabetic patients. Photomed Laser Surg 26(5):433–442. https://doi.org/10.1089/pho.2007.2197
Schindl A, Schindl M, Schon H, Knobler R, Havelec L, Schindl L (1998) Low-intensity laser irradiation improves skin circulation in patients with diabetic microangiopathy. Diabetes Care 21(4):580–584
Administration FaD (June 2006) Guidance for industry chronic cutaneous ulcer and burn wounds — developing products for treatment. Rockville, MD
Acknowledgements
We would like to thank Vladimir Heiskanen of the University of Helsinki for access to the photobiomodulation comprehensive database (http://www.bitly.com/PBM-database).
Funding
The manufacturer of the device provided active/sham devices and payment for third-party services (caregivers, statistical analysis) and provided a camera for the study. The manufacturer was not involved in the collection or analysis of the data.
Author information
Authors and Affiliations
Contributions
AH, OE, TT, YNG, and ML conceived the study and designed the trial; AH, OE, and TT were responsible for patient recruitment and clinical evaluations, DS was involved with the treatment and collected data, LG validated and analyzed the data, conducted literature review, and together with AH drafted the original manuscript. AH, TT, YNG, LG, and ML reviewed the manuscript critically. AH takes responsibility for the paper as a whole. All authors gave final approval for the version to be published.
Corresponding author
Ethics declarations
Ethics approval
This clinical trial (ClinicalTrials.gov: NCT01493895) was approved by the clinical trial ethical review board of The Hadassah Medical Organization (0122–11-HMO) prior to recruitment.
Consent to participate.
All patients provided written informed consent before entering the study.
Consent for publication
Figure 2 contains feet from 2 patients. The pictures were taken during 2014. Both patients are deceased; one died in 2015 and the other in 2018. The text was anonymized by omitting the exact age and gender from the legend. There is no additional identifiable data in the photos.
Data sharing
The individual measurements collected in this study and details of diabetes status and care (according to Jeffcoat et al. [3]) are reported in Supplementary Tables S1 and S2.
Conflict of interest
LG is paid as a consultant by the manufacturer of the device to give recommendations for treatment protocols. This was not relevant in this study. All other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Haze, A., Gavish, L., Elishoov, O. et al. Treatment of diabetic foot ulcers in a frail population with severe co-morbidities using at-home photobiomodulation laser therapy: a double-blind, randomized, sham-controlled pilot clinical study. Lasers Med Sci 37, 919–928 (2022). https://doi.org/10.1007/s10103-021-03335-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-021-03335-9