Abstract
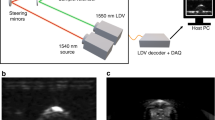
Successful laser surgery is characterized by a precise cut and effective hemostasis with minimal collateral thermal damage to the adjacent tissues. Consequently, the surgeon needs to control several parameters, such as power, pulse repetition rate, and velocity of movements. In this study we propose utilizing optoacoustics for providing the necessary real-time feedback of cutting efficiency and collateral thermal damage. Laser ablation was performed on a bovine meat slab using a Q-switched Nd-YAG laser (532 nm, 4 kHz, 18 W). Due to the short pulse duration of 7.6 ns, the same laser has also been used for generation of optoacoustic signals. Both the shockwaves, generated due to tissue removal, as well as the normal optoacoustic responses from the surrounding tissue were detected using a single broadband piezoelectric transducer. It has been observed that the rapid reduction in the shockwave amplitude occurs as more material is being removed, indicating decrease in cutting efficiency, whereas gradual decrease in the optoacoustic signal likely corresponds to coagulation around the ablation crater. Further heating of the surrounding tissue leads to carbonization accompanied by a significant shift in the optoacoustic spectra. Our results hold promise for real-time monitoring of cutting efficiency and collateral thermal damage during laser surgery. In practice, this could eventually facilitate development of automatic cut-off mechanisms that will guarantee an optimal tradeoff between cutting and heating while avoiding severe thermal damage to the surrounding tissues.







Similar content being viewed by others
References
Neukam FW, Stelzle F (2010) Laser tumor treatment in oral and maxillofacial surgery. Phys Procedia 5:91–100
White JM, Goodis HE, Rose CL (1991) Use of the pulsed Nd:YAG laser for intraoral soft tissue surgery. Lasers Surg Med 11:455–461
Tuchmann A, Bauer P, Plenk H, Braun O (1986) Comparative study of conventional scalpel and CO2-laser in experimental tumor surgery. Res Exp Med 186:375–386
Lanzafame RJ, Rogers DW, Naim JO, Herrera HR, DeFranco C, Hinshaw JR (1986) The effect of CO2 laser excision on local tumor recurrence. Lasers Surg Med 6:103–105
Pogrel MA, McCracken KJ, Daniels TE (1990) Histologic evaluation of the width of soft tissue necrosis adjacent to carbon dioxide laser incisions. Oral Surg, Oral Med, Oral Pathol 70:564–568
Parker S (2007) Lasers and soft tissue: “loose” soft tissue surgery. Br Dent J 202:185–191
White JM, Chaudhry S, Kudler J (1998) Nd:YAG and CO2 laser therapy of oral mucosal lesions. J Clin Laser Med Surg 16:299–304
Shakhov AV, Terentjeva AB, Kamensky VA, Snopova LB, Gelikonov VM, Feldchtein FI, Sergeev AM (2001) Optical coherence tomography monitoring for laser surgery of laryngeal carcinoma. J Surg Oncol 77:253–258
Walsh JT, Flotte TJ, Deutsch TF (1989) Er:YAG laser ablation of tissue: effect of pulse duration and tissue type on thermal damage. Lasers Surg Med 9:314–326
Das D, Reed S, Klokkevold P, Wu B (2013) A high-throughput comparative characterization of laser-induced soft tissue damage using 3D digital microscopy. Lasers Med Sci 28:657–658
Ryan RW, Wolf T, Spetzler RF, Coons SW, Fink Y, Preul MC (2010) Application of a flexible CO2 laser fiber for neurosurgery: laser-tissue interactions. J Neurosurg 112:434–443
Nahen K, Vogel A (1999) Investigations on acoustic on-line monitoring of IR laser ablation of burned skin. Lasers Surg Med 25:69–78
Rupprecht S, Tangermann-Gerk K, Wiltfang J, Neukam FW, Schlegel A (2004) Sensor-based laser ablation for tissue specific cutting: an experimental study. Lasers Med Sci 19:81–88
Stelzle F, Tangermann-Gerk K, Adler W, Zam A, Schmidt M, Douplik A, Nkenke E (2010) Diffuse reflectance spectroscopy for optical soft tissue differentiation as remote feedback control for tissue-specific laser surgery. Lasers Surg Med 42:319–325
Stelzle F, Zam A, Adler W, Tangermann-Gerk K, Douplik A, Nkenke E, Schmidt M (2011) Optical nerve detection by diffuse reflectance spectroscopy for feedback controlled oral and maxillofacial laser surgery. J Transl Med 9:20
Douplik A, Zam A, Hohenstein R, Kalitzeos A, Nkenke E, Stelzle F (2010) Limitations of cancer margin delineation by means of autofluorescence imaging under conditions of laser surgery. J Innov Opt Health Sci 03:45–51
Wang LV (2009) Photoacoustic imaging and spectroscopy. CRC Press, Boca Raton
Ntziachristos V, Razansky D (2010) Molecular imaging by means of multispectral optoacoustic tomography (MSOT). Chem Rev 110:2783–2794
Razansky D (2012) Multi-spectral optoacoustic tomography—volumetric color hearing in real time. IEEE J Sel Top Quant Electron 18:1234–1243
Larin KV, Larina IV, Esenaliev RO (2005) Monitoring of tissue coagulation during thermotherapy using optoacoustic technique. J Phys D: Appl Phys 38:2645–2653
Cui H, Yang X (2011) Real-time monitoring of high-intensity focused ultrasound ablations with photoacoustic technique: an in vitro study. Med Phys 38:5345
Chitnis PV, Brecht H-P, Su R, Oraevsky AA (2010) Feasibility of optoacoustic visualization of high-intensity focused ultrasound-induced thermal lesions in live tissue. J Biomed Opt 15:021313
Esenaliev RO, Oraevsky AA, Letokhov VS, Karabutov AA, Malinsky TV (1993) Studies of acoustical and shock waves in the pulsed laser ablation of biotissue. Lasers Surg Med 13:470–484
Park HK, Kim D, Grigoropoulos CP, Tam AC (1996) Pressure generation and measurement in the rapid vaporization of water on a pulsed-laser-heated surface. J Appl Phys 80:4072
Agah R, Gandjbakhche aH, Motamedi M, Nossal R, Bonner RF (1996) Dynamics of temperature dependent optical properties of tissue: dependence on thermally induced alteration. IEEE Trans Bio-Med Eng 43:839–846
Lin WC, Buttemere C, Mahadevan-Jansen A (2003) Effect of thermal damage on the in vitro optical and fluorescence characteristics of liver tissues. IEEE J Sel Top Quant Electron 9:162–170
Jallo GI, Kothbauer KF, Epstein FJ (2002) Contact laser microsurgery. Child's Nerv Syst: ChNS: Off J Int Soc Pediatr Neurosurg 18:333–336
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bay, E., Douplik, A. & Razansky, D. Optoacoustic monitoring of cutting efficiency and thermal damage during laser ablation. Lasers Med Sci 29, 1029–1035 (2014). https://doi.org/10.1007/s10103-013-1434-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-013-1434-y