Abstract
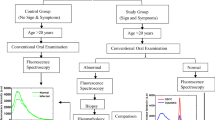
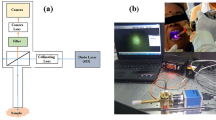
A novel in vivo fluorescence spectroscopic diagnostic method has been developed in an animal model to make a quantified precancer diagnosis. In the study, 40 golden hamsters were randomly divided into four groups (groups A, B, C, and D), with group A being the control group and the other three groups being inducted at different precancer stages. A 1% Rose Bengal (RB) solution was used for the fluorescence spectroscopic diagnosis. A parameter K defined as K = IRB/Iauto was introduced to reflect the amount of RB in the tissue, where IRB and Iauto represent the fluorescence peak intensity of the RB in the tissue and the autofluorescence intensity of tissue at 580 nm, respectively. The average K values of the four groups were calculated and statistically analyzed by analysis of variance (ANOVA), which revealed statistically significant differences within each group as well as between groups (p < 0.001). After analysis by Clementine 11.1 C&R Tree modeling (CART), the following diagnostic criteria were set: normal, K ≤8.91; simple hyperplasia, 8.91 < K ≤41.92; mild dysplasia, 41.92 < K ≤ 70.79; moderate and severe dysplasia, K >70.79. The sensitivity and specificity to detect precancerous lesions compared with scalpel biopsy were calculated. The results of this study showed that the spectrofluorometric method mediated by RB could accurately discriminate different precancer stages.



Similar content being viewed by others
References
Johnson NW, Warnakulasuriya S, Gupta PC et al (2011) Global oral health inequalities in incidence and outcomes for oral cancer: causes and solutions. Adv Dent Res 23:237–246
Rhodus NL (2009) Oral cancer and precancer: improving outcomes. Compend Contin Educ Dent 30:486–488, 490–494, 496–498 passim
Gillenwater A, Papadimitrakopoulou V, Richards-Kortum R (2006) Oral premalignancy: new methods of detection and treatment. Curr Oncol Rep 8:146–154
Güneri P, Epstein JB, Kaya A et al (2011) The utility of toluidine blue staining and brush cytology as adjuncts in clinical examination of suspicious oral mucosal lesions. Int J Oral Maxillofac Surg 40:155–161
Jerjes WK, Upile T, Wong BJ et al (2011) The future of medical diagnostics: review paper. Head Neck Oncol 3:38
Kraft M, Betz CS, Leunig A et al (2011) Value of fluorescence endoscopy for the early diagnosis of laryngeal cancer and its precursor lesions. Head Neck 33:941–948
Rajaram N, Reichenberg JS, Migden MR et al (2010) Pilot clinical study for quantitative spectral diagnosis of non-melanoma skin cancer. Lasers Surg Med 42:716–727
Lingen MW, Kalmar JR, Karrison T et al (2008) Critical evaluation of diagnostic aids for the detection of oral cancer. Oral Oncol 44:10–22
Argüeso P, Tisdale A, Spurr-Michaud S et al (2006) Mucin characteristics of human corneal-limbal epithelial cells that exclude the Rose Bengal anionic dye. Invest Ophthalmol Vis Sci 47:113–119
Wachter E, Dees C, Harkins J et al (2003) Topical Rose Bengal: pre-clinical evaluation of pharmacokinetics and safety. Lasers Surg Med 32:101–110
Du GF, Li CZ, Chen HZ et al (2007) Rose Bengal staining in detection of oral precancerous and malignant lesions with colorimetric evaluation: a pilot study. Int J Cancer 120:1958–1963
MacDonald DG (1981) Comparison of epithelial dysplasia in hamster cheek pouch carcinogenesis and human oral mucosa. J Oral Pathol 10:186–191
Epstein JB, Oakley C, Millner A et al (1997) The utility of toluidine blue application as a diagnostic aid in patients previously treated for upper oropharyngeal carcinom. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 83:537–547
Bsoul SA, Huber MA, Terezhalmy GT (2005) Squamous cell carcinoma of the oral tissues: a comprehensive review for oral healthcare providers. J Contemp Dent Pract 6:1–16
Bedard N, Pierce M, El-Nagger A (2010) Emerging roles for multimodal optical imaging in early cancer detection: a global challenge. Technol Cancer Res Treat 9:211–217
Rahman MS, Ingole N, Roblyer D et al (2010) Evaluation of a low-cost, portable imaging system for early detection of oral cancer. Head Neck Oncol 2:10
Vigneswaran N, Koh S, Gillenwater A (2009) Incidental detection of an occult oral malignancy with autofluorescence imaging: a case report. Head Neck Oncol 1:37
Roblyer D, Kurachi C, Stepanek V et al (2009) Objective detection and delineation of oral neoplasia using autofluorescence imaging. Cancer Prev Res (Phila) 2:423–431
Thong PS, Olivo M, Kho KW et al (2007) Laser confocal endomicroscopy as a novel technique for fluorescence diagnostic imaging of the oral cavity. J Biomed Opt 12:014007
Qin YL, Luan XL, Bi LJ et al (2007) Real-time detection of dental calculus by blue-LED-induced fluorescence spectroscopy. J Photochem Photobiol B 87:88–94
Jiang CF, Wang CY, Chiang CP (2011) Comparative study of protoporphyrin IX fluorescence image enhancement methods to improve an optical imaging system for oral cancer detection. J Biomed Opt 16:076006
Srivastave SK, Modak MJ (1983) Rose Bengal-mediated inhibition of DNA polymerases; mechanism of inhibition of avian myeloblastosis virus reverse transcriptase under photooxidative conditions. Biochemistry 22:2283–2288
Utsuki S, Oka H, Kijima C et al (2011) Utility of intraoperative fluorescent diagnosis of residual hemangioblastoma using 5-aminolevulinic acid. Neurol India 59:612–615
Fukuhara H, Inoue K, Satake H et al (2011) Photodynamic diagnosis of positive margin during radical prostatectomy: preliminary experience with 5-aminolevulinic acid. Int J Urol 18:585–591
Kobayashi W, Liu Q, Nakagawa H et al (2006) Photodynamic therapy with mono-L-aspartyl chlorin e6 can cause necrosis of squamous cell carcinoma of tongue: experimental study on an animal model of nude mouse. Oral Oncol 42:46–50
Konopka K, Goslinski T (2007) Photodynamic therapy in dentistry. J Dent Res 86:694–707
Souza LR, Fonseca-Silva T, Pereira CS et al (2011) Immunohistochemical analysis of p53, APE1, hMSH2 and ERCC1 proteins in actinic cheilitis and lip squamous cell carcinoma. Histopathology 58:352–360
Grizzle WE, Srivastava S, Manne U (2011) The biology of incipient, pre-invasive or intraepithelial neoplasia. Cancer Biomark 9:21–39
Gandolfo S, Pentenero M, Broccoletti R et al (2006) Toluidine blue uptake in potentially malignant oral lesions in vivo: clinical and histological assessment. Oral Oncol 42:89–95
Acknowledgments
This research was supported by the scientific research fund from the Department of Education, Heilongjiang Province (No: 11541148) and the research fund from the First Affiliated Hospital of Harbin Medical University (2011BS006).
Author information
Authors and Affiliations
Corresponding author
Additional information
Lei Zhang and Jinna Shi contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhang, L., Bi, L., Shi, J. et al. A quantitative diagnostic method for oral mucous precancerosis by Rose Bengal fluorescence spectroscopy. Lasers Med Sci 28, 241–246 (2013). https://doi.org/10.1007/s10103-012-1054-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-012-1054-y