Abstract
The objective of this work is to test the ablation capability and fiber degradation of the novel Twister fibers (TW), in both the large (LTW) and the standard (STW) sizes, against the standard side-firing (SF) fiber in a clinical setting during the treatment of BPH patients using the 980-nm high-power diode laser (HPDL). One hundred and twenty BPH patients treated with HPDL (Ceralase300, Biolitec AG, Jena, Germany) were randomized to receive treatment by one of the three fibers. Operative time corrected to tissue volume, laser treatment time, and laser energy were measured. Ablation rate was calculated as follows: the decrease of the prostate volume after 6 months/laser time. The fibers’ resistance to degradation was defined by the laser energy needed to degrade the fiber completely. Preoperative prostate volume of 76 ± 38, 70 ± 39, and 88 ± 49 cc decreased by 49 ± 16, 51 ± 20, and 63 ± 16% for the SF, STW, and LTW fibers, respectively. This difference was highly significant when the LTW was compared to the other two fibers (p < 0.001). Prostate volume reduction post-operatively within each group as compared to the pre-operative volume was highly significant (p < 0.001). The ablation rate was highest in LTW, being 1.31 ± 0.59, 1.09 ± 0.51, and 1.54 ± 0.44 cc/min for the SF, STW, and LTW fibers, respectively. The LTW fiber resisted degradation more than the other fibers and the STW more than the SF fiber (p < 0.001). This study demonstrates the higher ablation efficiency and resistance to degradation of the LTW fiber as compared to the STW and SF fibers. The STW fiber has a similar ablation rate of the SF fiber but resists degradation better.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laser ablation of the prostate has gained wide popularity in recent years. Many studies have shown its advantage in being as efficacious as transurethral resection of the prostate without its side-effects and drawbacks. Consequently, new systems with higher power have been introduced to increase the efficiency of the procedure. Nevertheless, all these ablative procedures depend on the side-firing (SF) fiber to convey the laser power to the tissues [1–3]. Many disadvantages have been encountered while working with the side-firing fiber including fast degradation, leading to decreased power with the progress of the procedure leading to increased tissue coagulation rather than ablation and, hence, post-operative side-effects. [4] For this reason, the need for newer types of laser fibers to convey the laser energy to the tissue became clear.
The Twister laser (TW) fiber was introduced 2 years ago as an alternative to the standard SF fiber used for laser ablation of the prostate using the 980-nm high-power diode laser [5]. Contrary to the SF fiber, the TW fiber is an end-firing contact fiber with an angulated distal tip covered with quartz. It concentrates the laser power at this tip, transforming it into high heat, which leads to instant vaporization of tissue in contact with the tip of the fiber (Fig. 1). It works in contact mode, giving the surgeon the familiar tactile sensation of the TURP [6]. It does not emit a free beam, and the tissue effect depends on the temperature reached at the fiber tip. In contrast, free laser beam emitted from the SF fibers becomes absorbed in the tissue according to its wavelength and then transformed into heat energy. The final tissue effect in both fibers is thermal, and is dependent on the temperature generated in the tissues. At 60 degrees, tissue coagulation occurs, and at 100 degrees carbonization is the result, while ablation occurs only at 300°C. [7]
In a previous study, we tested the ablation rate and fiber degradation of the TW fiber versus the side-firing fiber on a bovine animal model. It was demonstrated in that study that both fibers work equally well regarding the ablative power and fiber degradation except at 200 W, where the side-firing fiber performed better. In that study, we had used the standard size Twister fiber (STW) for these experiments [6].
The ablative power and the degradation of this novel fiber were not tested in a clinical setting. It was our observation that this fiber performs very differently during laser ablation of the prostate as compared to our previous experimental experience that triggered this work. Recently, a newer TW fiber with a larger end size was introduced (LTW). In this work, we tried to quantify the ablative power and fiber degradation of these fibers during laser ablation of the prostate.
Materials and methods
One hundred and twenty patients were subjected to the 980-nm high-power diode laser ablation of the prostate due to lower urinary tract symptoms secondary to the BPH. These patients were randomized (simple 1:1 randomization) to receive this treatment with either the SF, the STW, or the LTW fibers (40 patients in each group) (Fig. 1). All cases were operated by a single surgeon (HS). We used a 300 watts machine (Ceralase, Biolitec AG, Jena, Germany) to generate a 980-nm laser through a diode semiconductor. All factors other than the fibers were standardized. All patients underwent the procedure under spinal anesthesia. The laser sheath used was a 23-F continuous irrigation laser scope (Karl Storz, Tuttlingen, Germany). The irrigation fluid used was normal saline at room temperature and its height fixed at 60 cm above the patient. Both the SF and TW fibers (Biolitec AG, Jena, Germany) were 600-μm fibers. The SF fiber has a reflective surface at its distal end that reflects the laser beam with a 70° forward angle. The distal end of the TW fiber is covered by quartz, which is angled by 30° on the horizontal plane. The laser energy is concentrated at the quartz tip. The SF fiber was operated in a non-contact mode keeping a distance of 0.5 to 1 mm from the tissue. The TW fibers were operated in a contact fashion. The maximum recommended power to be used with the SF and STW is 220 W and for the LTW is 300 W. The investigational nature of the study was explained to the patients and all signed an informed consent form. The study protocol was approved by the local ethics committee of the hospital.
Operative time corrected to prostate volume (operative time divided by prostate volume), laser treatment time, and laser energy were measured or calculated. Prostate volume, by transrectal ultrasonography, preoperatively and 6 months postoperatively were measured.
The ablation rate of the laser was measured by the prostate volume reduction after 6 months divided by laser time. The energy needed to ablate one cc of tissue was also calculated.
Fiber degradation was measured when the fibers ceased to function properly and tissue ablation decreased significantly as judged by the surgeon. In the side-firing fiber, this was manifested by damage of the reflective tip. In the Twister fiber, the limit was shown by the degradation of the angled tip.
Measuring the laser output at the fiber tip was not possible in the TW fiber since this fiber concentrates the laser energy at the tip and no laser beam is emitted from the tip. For that reason, the methodology used by Hermanns and colleagues [4] could not be used with the TW fibers.
Statistical analysis
Statistical analysis of data was done using SPSS (Statistical Package for the Social Sciences, version 16). All quantitative variables were expressed in the text as mean ±SD and range. Analysis of variance was used to compare parametric quantitative variables in the three groups. Whenever a significant difference between the groups’ means was obtained, LSD post-hoc analysis was performed. Non-parametric quantitative variables in the three groups were compared using the Kruskal–Wallis test. Pre-operative prostate size was compared to post-operative data within the same group using Wilcoxon signed-rank test. Chi-square test was used to compare qualitative variables of different groups. Fisher’s exact probability test was used instead of Chi-square when one or more expected cells value are less than 5. Spearman correlation test was used to rank variables positively or inversely versus each other. The difference between means was considered significant if the p value was <0.05 and highly significant if <0.001 [8].
Results
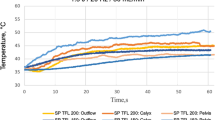
One hundred and seventeen patients were evaluable. Seventy-six of them reached 6-month post-operative follow-up point at the time of this study with three patients dropping out of the study (two from the STW group and one from the SF group). Pre-operative prostate volume, operative time, and laser treatment time were not significantly different between groups (Tables 1 and 2). Operative time corrected to prostate volume was significantly longer in the SF fiber as compared to those of both TW fibers. It was significantly less in the LTW fiber in comparison to that of the STW fiber (Fig. 2). This higher efficiency of the LTW fiber was reflected on both the 6 months prostate volume reduction and the ablation rate. Both were significantly higher in the LTW fiber as compared to the other two fibers (Figs. 3, 4). Prostate volume decreased significantly within each group after 6 months when compared to baseline (p < 0.001).
Regarding the resistance to degradation, 47 fibers reached their maximum usability as judged by the surgeon and had to be replaced with another fiber. This occurred in 25 SF, 12 STW, and ten LTW fibers. The LTW fiber has the highest durability. Additionally, the STW fiber has a higher durability as compared to that of the SF fiber (Fig. 5). This was not reflected on the number of fibers used per case statistically. This was 1.30 ± 0 .55 SF, 1.14 ± 0.42 STW, and 1.15 ± 0.36 LTW fibers/case.
Fiber resistance to degradation. The energy specified for each fiber type represents the mean energy at which fibers degraded and ceased to function properly. This occurred in 25 SF, 12 STW, and ten LTW fibers. a High significant difference between the SF and STW fibers. b High statistical significant difference between the SF and the LTW. c High significant difference between the STW and LTW fibers
There was a highly significant positive correlation between the prostatic volume on one hand and the operative and laser treatment times on the other (Table 3).
Discussion
The 980-nm high-power diode laser was introduced a few years ago to treat benign prostatic hyperplasia (BPH). Several studies have shown that using the side-firing fiber to convey the laser energy to the tissues produced superb ablation and hemostasis and had a good clinical outcome. The improvements involved patient symptomatology, symptoms score, flow rates, and a significant decrease in the prostate volume and PSA without a negative effect on sexual function. Furthermore, it allowed the use of this technology with morbid patients commonly found in this age group [1–3]. Nevertheless, long-term high-quality outcome studies are needed before a final conclusion can be reached.
Several potential problems are encountered while working with SF fibers. Firstly, they suffer degradation with use. This was recognized when using these fibers with the Nd-YAG [9], KTP [4], and 980-nm diode lasers [6]. Degradation of the laser fiber power renders it more coagulative than ablative due to beam scattering [10]. Additionally, due to the absorption of the 980-nm wavelength in water, the SF fiber has to be operated at a close but non-contact distance from the tissues of about 0.5 mm [13]. This distance is very hard to maintain throughout the procedure. The same finding was encountered in groups with vast experience in prostatic ablation using PVP [11]. Should this distance increase, laser power at tissue surface decreases rendering it more coagulative and hence increasing the side-effects. On the other hand, if the fiber gets into contact with the tissues, or if debris sticks to the reflective surface, it becomes overheated and subsequently damaged. The above-mentioned reasons may explain the discrepancy between the small coagulative zone found in experimental studies and that experienced in clinical settings, resulting in increased post-operative irritative symptoms and tissue sloughing, which results from deep coagulation zones [1, 3, 5, 10]. Another problem that may occur with the non-contact laser in general and is not dependent on the laser wavelength is its partial reflection from the tissues boundary layer. This may be a potential hazard to the surrounding tissues [10] and of course to the optics. For this particular reason, and due to the scatter that occurs due to the fiber degradation, some authors have suggested to lower the laser power while ablating prostatic tissue close to the sphincter [1], while others have suggested adopting an alternative technique that avoids working close to the sphincter towards the end of the procedure when the fiber is most degraded [11]. Our results support most of the above-mentioned concerns. We have shown that the SF fibers are most susceptible to degradation.
Several theoretical advantages are expected from the TW fiber. Being a contact fiber cancels many of the disadvantages of the SF fiber. No tissue distance needs to be observed, which is of particular importance at the beginning of the procedure due to the lack of working space within the prostatic urethra. Consistency of the ablation throughout the procedure is also expected, since the fiber does not depend on the distance from the tissue to execute an effect and has no reflective surface that may get damaged or degrades with the advancement of the procedure. Since there is no free beam, reflection from tissue boundaries is not problematic, increasing its safety to the nearby tissue. This is in addition to the similarity of this fiber to TURP decreasing the learning curve and increasing the attractiveness of the procedure to endo-urologists. Nevertheless, none of these hypothesized advantages was proved. To our knowledge, this study is the first to address the novel TW fiber ablation rate and degradation in clinical settings.
All three of the fibers performed superbly in ablating the prostatic tissue. Nevertheless, the efficiency of the LTW fiber was significantly higher in prostatic volume reduction. This translated to a higher ablation rate of the LTW fiber. The corrected operative time per tissue volume is another way of illustrating the higher efficiency of both TW fibers over the SF fiber and superior efficiency of LTW over the other fibers. This can be of importance in decreasing the operative time for the same prostatic volume.
Another great advantage of TW fibers in general and the LTW in particular is their durability. The TW fiber can resist degradation and can withstand much higher energy as compared to the side-firing fiber. The large fiber showed the highest resistance to degradation and the maximum durability. The reason that this was not reflected on the number of fibers used per case is due to the larger volume the LTW fiber ablates per case. This may have cost-advantages, especially in large prostates.
Whether the previously mentioned results will be reflected in the clinical outcome is yet to be addressed. A randomized study is needed to address the clinical impact of the higher ablation rate and resistance to degradation of the LTW fiber on patient symptomatology. Unfortunately, no such studies are available in the literature at this time.
Lastly, it was clear in this study that there are big differences and discrepancies between experimental studies and studies in clinical settings. Our current results contradict our previous experimental study that showed a higher ablation rate of the SF fiber at high power [6]. Similar discrepancies were found in other types of ablative lasers such as the KTP laser [12, 13]. Many explanations can be provided for such phenomenon. The use of chromophore-endowed or chromophore-deprived models can lead to big differences in the experimental results [14]. The strict distance of the SF fibers from the tissue that can be maintained during experimental settings is seldom possible during clinical applications [11]. The cooling effect of the continuous irrigation and the blood flow may also give rise to some discrepancies. For these previously mentioned reasons, the importance of such experiments in clinical settings is clear when compared to ex vivo and in vitro studies.
Conclusions
The LTW fiber appears to have a higher prostatic ablation rate and resists degradation in comparison to the STW and the SF fibers. This is reflected in a higher decrease in prostatic volume. Clinical outcome studies are needed for this promising novel fiber to see whether these superior characteristics would have an impact on the BPH patients’ outcome.
References
Erol A, Cam K, Tekin A et al (2009) High-power diode laser vaporization of the prostate: preliminary results for benign prostatic hyperplasia. J Urol 82(3):1078–1082
Leonardi R (2009) Preliminary results on selective light vaporization with the side-firing 980-nm diode laser in benign prostatic hyperplasia: an ejaculation sparing technique. Prostate Cancer Prostatic Dis 12(3):277–280
Chen CH, Chiang PH, Chuang YC et al (2010) Preliminary results of prostate vaporization in the treatment of benign prostatic hyperplasia by using a 200-W high-intensity diode laser. Urology 75(3):658–663
Hermanns T, Sulser T, Fatzer M et al (2008) Laser fiber deterioration and loss of power output during photo-selective 80-W potassium-titanyl-phosphate laser vaporisation of the prostate. Eur Urol 55:685
Wendt-Nordahl G, Huckele S, Honeck P et al (2007) 980-nm Diode laser: a novel laser technology for vaporization of the prostate. Eur Urol 52(6):1723–8
Shaker H, Salman M (2010) The Twister Fiber. A comparative study of tissue interaction between this novel fiber and the side-firing fiber using the 980-nm laser in bovine kidneys. J Endourol 24(11):1851–1855
Niemz MH (2004) Laser-tissue interactions: fundamentals and applications, 3rd edn. Springer, Berlin Heidelberg New York
Knapp RG, Miller MC (1992) Clinical epidemiology and biostatistics, 3rd edn. Williams & Wilkins, Baltimore and Malvern
Reich O, Michel MS, Schneede P et al (2004) Durability of probes for interstitial laser coagulation: impact of power setting and probe design. J Endourol 18:299–302
Teichmann HO, Herrmann TR, Bach T (2007) Technical aspects of lasers in urology. World J Urol 25:221–225
Gomez Sancha F, Bachmann A, Choi BB et al (2007) Photoselective vaporization of the prostate (GreenLight PV): lessons learnt after 3500 procedures. Prostate Cancer Prostatic Dis 10:316–322
Seitz M, Reich O, Gratzke C et al (2009) High-power diode laser at 980 nm for the treatment of benign prostatic hyperplasia: ex vivo investigations on porcine kidneys and human cadaver prostates. Lasers Med Sci 24:172–178
Ahmed HU, Thwaini A, Shergill IS et al (2007) Greenlight prostatectomy: a challenge to the gold standard? A review of KTP photoselective vaporization of the prostate. Surg Laparosc Endosc Percutan Tech 17:156–163
Sroka R, Ackermann A, Tilki D et al (2007) In-vitro comparison of the tissue vaporization capabilities of different lasers. Med Laser Appl 22:227–231
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Shaker, H., Alokda, A. & Mahmoud, H. The Twister laser fiber degradation and tissue ablation capability during 980-nm high-power diode laser ablation of the prostate. A randomized study versus the standard side-firing fiber. Lasers Med Sci 27, 959–963 (2012). https://doi.org/10.1007/s10103-011-1017-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-011-1017-8