Abstract
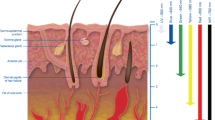
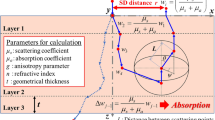
Various techniques to enhance light propagation in skin have been studied in low-level laser therapy. In this study, three mathematical modeling methods for five selected techniques were implemented so that we could understand the mechanisms that enhance light propagation in skin. The five techniques included the increasing of the power and diameter of a laser beam, the application of a hyperosmotic chemical agent (HCA), and the whole and partial compression of the skin surface. The photon density profile of the five techniques was solved with three mathematical modeling methods: the finite element method (FEM), the Monte Carlo method (MCM), and the analytic solution method (ASM). We cross-validated the three mathematical modeling results by comparing photon density profiles and analyzing modeling error. The mathematical modeling results verified that the penetration depth of light can be enhanced if incident beam power and diameter, amount of HCA, or whole and partial skin compression is increased. In this study, light with wavelengths of 377 nm, 577 nm, and 633 nm was used.







Similar content being viewed by others
References
Tuchin VV (2000) Optical properties of tissues with strong (multiple) scattering. In: O’Shea DC (ed) Tissue optics: light scattering methods and instruments for medical diagnosis. SPIE Press, Bellingham, WA, USA, pp 3–98
Gratton G, Maier JS, Fabiani M, Mantulin WW, Gratton E (1994) Feasibility of intracranial near-infrared optical scanning. Psychophysiology 31:211–215. doi:10.1111/j.1469–8986.1994.tb01043.x
Jobsis FF (1977) Noninvasive, infrared monitoring of cerebral and myocardial oxygen sufficiency and circulatory parameters. Science 198:1264–1267. doi:10.1126/science.929199
Tunér J, Hode L (2002) Laser therapy—clinical practice and scientific background. Prima Books, Grängesberg, Sweden
Carroll L, Humphreys TR (2006) LASER-tissue interactions. Clin Dermatol 24:2–7. doi:10.1016/j.clindermatol.2005.10.019
Tuchin VV (2002) Dynamic optical coherence tomography in studies of optical clearing, sedimentation, and aggregation of immersed blood. Appl Opt 41:258–271. doi:10.1364/AO.41.000258
Tuchin VV (2006) Optical clearing of tissues and blood. SPIE Press, Bellingham, WA, USA
Vargas G, Chan EK, Barton JK, Rylander HG, Welch AJ (1999) Use of an agent to reduce scattering in skin. Lasers Surg Med 24:133–141 doi:10.1002/(SICI)1096–9101(1999)24:2<133::AID-LSM9>3.0.CO;2-X
He Y, Wang RK (2004) Improvement of low-level light imaging performance using optical clearing method. Biosens Bioelectron 20:460–467. doi:10.1016/j.bios.2004.04.013
Khan MH, Choi B, Chess S, Kelly KM, McCullough J, Nelson JS (2004) Optical clearing of in vivo human skin: implications for light-based diagnostic imaging and therapeutics. Lasers Surg Med 34:83–85. doi:10.1002/lsm.20014
Tuchin VV (2007) A clear vision for laser diagnostics. IEEE J Sel Top Quantum Electron 13:1621–1628. Review. doi:10.1109/JSTQE.2007.911313
Chan EK, Sorg B, Protsenko D, O’Neil M, Motamedi M, Welch AJ (1996) Effects of compression on soft tissue optical properties. IEEE J Sel Top Quantum Electron 2:943–950. doi:10.1109/2944.577320
Shangguan H, Prahl SA, Jacques SL, Casperson LW, Gregory KW (1998) Pressure effects on soft tissues monitored by changes in tissue optical properties. Proc SPIE 3254:366–371. doi:10.1117/12.308187
Arridge SR (1999) Optical tomography in medical imaging. Inverse Probl 15:R41–R93. doi:10.1088/0266–5611/15/2/022
Van Gemert MJC, Jacques SL, Sterenborg HJCM, Star WM (1989) Skin optics. IEEE T Biomed Eng 36:1146–1154
Wang L, Jacques SL, Zheng L (1995) MCML–Monte Carlo modeling of light transport in multi-layered tissues. Comput Methods Programs Biomed 47:131–146. doi:10.1016/0169–2607(95)01640-F
Wang L, Jacques SL, Zheng L (1997) CONV—convolution for responses to a finite diameter photon beam incident on multi-layered tissues. Comput Methods Programs Biomed 54:141–150. doi:10.1016/S0169–2607(97)00021–7
Desmettre T, Mordon S (2005) Comparison of laser beam intensity profiles produced by photodynamic therapy (PDT) and transpupillary thermotherapy (TTT) lasers. Lasers Surg Med 36:315–322. doi:10.1002/lsm.20159
Acknowledgments
This study was supported by a grant from the Next Generation New Technology Program provided by the Ministry of Commerce, Industry, and Energy, Republic of Korea (10028424). K. Kwon is supported by grants from the Korea Health 21 R & D Project provided by the Ministry of Health & Welfare, Republic of Korea (02-PJ3-PG6-EV07-0002) and from the Brain Research Center of the 21st Century Frontier Research Program provided by the Ministry of Science and Technology, Republic of Korea (M103KV010019-06K2201-01910).
Author information
Authors and Affiliations
Corresponding author
Appendix 1
Appendix 1
Nomenclature
- Φ:
-
photon density profile (W/cm2)
- q:
-
light source function (W/cm3)
- \(\Re \) :
-
Robin function, which is the photon density profile with respect to the Dirac delta source (W/cm3)
- μ a :
-
absorption coefficient (cm−1)
- μ s :
-
scattering coefficient (cm−1)
- g:
-
anisotropy factor
- \(d,\mu _{s} \prime ,\mu _{a} \) :
-
reduced scattering coefficient (cm−1) \({\left( {\mu _{s} \prime {\text{ = }}{\left( {1 - g} \right)}\mu _{s} } \right)}\)
- κ :
-
diffusion coefficient (cm) \({\left( {{\kappa = 1} \mathord{\left/ {\vphantom {{\kappa = 1} {{\left( {3{\left( {\mu _{a} + \mu _{s} \prime } \right)}} \right)}}}} \right. \kern-\nulldelimiterspace} {{\left( {3{\left( {\mu _{a} + \mu _{s} \prime } \right)}} \right)}}} \right)}\)
- n:
-
refractive index
- a:
-
reflection coefficient on the surface
- c:
-
speed of light in a vacuum (cm/s) (c = 2.99 × 1010 cm/s)
- ω :
-
angular modulation frequency of the source intensity(1/s)
- Ω:
-
region of interest (skin structure)
- ∂Ω:
-
boundary of Ω (∂Ω = ∂topΩ + ∂bottomΩ + ∂leftΩ + ∂rightΩ)
- ∂topΩ:
-
top boundary of Ω
- ∂bottomΩ:
-
bottom boundary of Ω
- ∂leftΩ:
-
left boundary of Ω
- ∂rightΩ:
-
right boundary of Ω
- N b :
-
number of finite element basis
Rights and permissions
About this article
Cite this article
Kwon, K., Son, T., Lee, KJ. et al. Enhancement of light propagation depth in skin: cross-validation of mathematical modeling methods. Lasers Med Sci 24, 605–615 (2009). https://doi.org/10.1007/s10103-008-0625-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-008-0625-4