Abstract
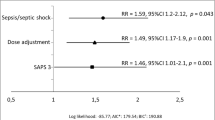
To determine whether target concentration non-attainment can be anticipated in critically ill patients prior to initiating empiric β-lactam antibiotic therapy based on readily available clinical factors. Retrospective review of consecutive patients treated with piperacillin or meropenem and who underwent therapeutic drug monitoring (TDM) at St Vincent’s Hospital (Sydney, Australia) between January 2013 and December 2015 was performed. Predefined subgroups were patients who received continuous renal replacement therapy (CRRT) and those who did not (non-CRRT). Potential risk factors were evaluated by correlation with β-lactam antibiotic trough concentrations (Cmin) lower than or equal to targeted minimum inhibitory concentration (MIC). Only the first drug concentration after initiation of the antibiotic treatment was included to reflect empirical dose selection. A total of n = 249 patients (piperacillin, n = 169; meropenem, n = 80) were investigated. For non-CRRT patients (n = 210), multivariate analysis demonstrated the following: male gender (p = 0.006); younger age (p = 0.015); prescribed daily antibiotic dose less than 1.5 times the product information recommendations (p = 0.004); lack of positive microbiology (p = 0.006); lower overall illness severity (p = 0.005); and estimated glomerular filtration rate (eGFR) ≥ 90 mL/min/1.73 m2 (p < 0.001), to be associated with Cmin ≤ MIC. No predictor variable was found to be significantly associated with Cmin ≤ MIC for the CRRT cohort. Evaluating the risk of target concentration non-attainment using simple clinical factors is possible at the bedside for non-CRRT patients prior to empiric antibiotic initiation. Clinicians should be wary of selecting doses based on the product information especially when treating younger male patients with apparently ‘normal’ renal function.

Similar content being viewed by others
Change history
17 June 2021
A Correction to this paper has been published: https://doi.org/10.1007/s10096-021-04291-6
References
Dulhunty JM, Webb SA, Paterson DL, Bellomo R, Myburgh J, Roberts JA et al (2010) A survey of antibiotic prescribing practices in Australian and New Zealand intensive care units. Crit Care Resusc 12:162
Kollef MH, Sherman G, Ward S, Fraser VJ (1999) Inadequate antimicrobial treatment of infections: a risk factor for hospital mortality among critically ill patients. Chest 115:462–474
Alp E (2016) Right first time! Ann Transl Med 4:331
Ferrer R, Martin-Loeches I, Phillips G, Osborn TM, Townsend S, Dellinger RP et al (2014) Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med 42:1749–1755
Taccone FS, Laterre PF, Dugernier T, Spapen H, Delattre I, Wittebole X et al (2010) Insufficient β-lactam concentrations in the early phase of severe sepsis and septic shock. Crit Care 14:R126
Liu VX, Fielding-Singh V, Greene JD, Baker JM, Iwashyna TJ, Bhattacharya J et al (2017) The timing of early antibiotics and hospital mortality in sepsis. Am J Respir Crit Care Med 196:856–863
Roberts JA, Norris R, Paterson DL, Martin JH (2012) Therapeutic drug monitoring of antimicrobials. Br J Clin Pharmacol 73:27–36
Muller AE, Huttner B, Huttner A (2018) Therapeutic drug monitoring of beta-lactams and other antibiotics in the intensive care unit: which agents, which patients and which infections? Drugs 23:1–13
Craig WA (1998) Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis 26:1–10
McKinnon PS, Paladino JA, Schentag JJ (2008) Evaluation of area under the inhibitory curve (AUIC) and time above the minimum inhibitory concentration (T > MIC) as predictors of outcome for cefepime and ceftazidime in serious bacterial infections. Int J Antimicrob Agents 31:345–351
Roberts JA, Paul SK, Akova M, Bassetti M, De Waele JJ, Dimopoulos G et al (2014) DALI: defining antibiotic levels in intensive care unit patients: are current β-lactam antibiotic doses sufficient for critically ill patients? Clin Infect Dis 58:1072–1083
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, Feldman HI et al (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150:604–612
De Waele JJ, Lipman J, Akova M, Bassetti M, Dimopoulos G, Kaukonen M et al (2014) Risk factors for target non-attainment during empirical treatment with β-lactam antibiotics in critically ill patients. Intensive Care Med 40:1340–1351
Conil JM, Georges B, Mimoz O, Dieye E, Ruiz S, Cougot P et al (2006) Influence of renal function on trough serum concentrations of piperacillin in intensive care unit patients. Intensive Care Med 32:2063–2066
Schaeffner E (2017) Determining the glomerular filtration rate—an overview. J Ren Nutr 27:375–380
Udy AA, Roberts JA, Shorr AF, Boots RJ, Lipman J (2013) Augmented renal clearance in septic and traumatized patients with normal plasma creatinine concentrations: identifying at-risk patients. Crit Care 17:R35
Claus BO, Hoste EA, Colpaert K, Robays H, Decruyenaere J, De Waele JJ (2013) Augmented renal clearance is a common finding with worse clinical outcome in critically ill patients receiving antimicrobial therapy. J Crit Care 28:695–700
Huttner A, Von Dach E, Renzoni A, Huttner BD, Affaticati M, Pagani L et al (2015) Augmented renal clearance, low β-lactam concentrations and clinical outcomes in the critically ill: an observational prospective cohort study. Int J Antimicrob Agents 45:385–392
Thomas DM, Coles GA, Williams JD (1994) What does the renal reserve mean? Kidney Int 45:411–416
Brusselaers N, Vogelaers D, Blot S (2011) The rising problem of antimicrobial resistance in the intensive care unit. Ann Intern Med 1:47
Imani S, Buscher H, Marriott D, Gentili S, Sandaradura I (2017) Too much of a good thing: a retrospective study of β-lactam concentration-toxicity relationships. J Antimicrob Chemother 72:2891–2897
Huttner A, Harbarth S, Hope WW, Lipman J, Roberts JA (2015) Therapeutic drug monitoring of the β-lactam antibiotics: what is the evidence and which patients should we be using it for? J Antimicrob Chemother 70:3178–3183
Woksepp H, Hällgren A, Borgström S, Kullberg F, Wimmerstedt A, Oscarsson A et al (2017) High target attainment for β-lactam antibiotics in intensive care unit patients when actual minimum inhibitory concentrations are applied. Eur J Clin Microbiol Infect Dis 36:553–563
Tam VH, McKinnon PS, Akins RL, Rybak MJ, Drusano GL (2002) Pharmacodynamics of cefepime in patients with gram-negative infections. J Antimicrob Chemother 50:425–428
Acknowledgements
The preliminary results of this study were presented at the 25th European Congress of Clinical Microbiology and Infectious Disease. We wish to thank the staff of the TDM Laboratory, SydPath (assaying of specimens) and Intensive Care (collection of specimens), St Vincent’s Hospital.
Funding
This work was supported by the University of Notre Dame Australia at the School of Medicine Sydney (NO333732 to SI) and an Australian Government Research Training Program (RTP) Scholarship to IS.
Author information
Authors and Affiliations
Contributions
SI collected data and prepared the manuscript. HB, DM, RD and RN assisted with study design and reviewed the manuscript. GJ assisted with study design, data collection and reviewed the manuscript. SG performed data analysis and reviewed the manuscript. IS conceived and designed the study, performed preliminary data analysis and reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics
Ethical review and approval was obtained through St Vincent’s Hospital Sydney Human Research Ethics Committee (Reference: LNR/14/SVH/148, SSA: LNRSSA/14/SVH/226).
Competing interests
The authors declare that they have no competing interests.
Electronic supplementary material
ESM 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Imani, S., Buscher, H., Day, R. et al. An evaluation of risk factors to predict target concentration non-attainment in critically ill patients prior to empiric β-lactam therapy. Eur J Clin Microbiol Infect Dis 37, 2171–2175 (2018). https://doi.org/10.1007/s10096-018-3357-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-018-3357-9