Abstract
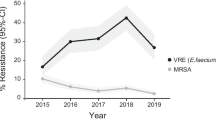
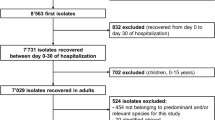
We characterize the epidemiology of pediatric bloodstream infections (BSIs) in Switzerland. We analyzed pathogen distribution and resistance patterns in monomicrobial and polymicrobial BSIs in children from 2008 to 2014 using data from the Swiss antibiotic resistance centre (ANRESIS). A confirmatory statistical analysis was performed comparing pathogens and resistance across 20 acute care hospitals. We identified 3,067 bacteremia episodes, of which 1,823 (59 %) were considered true BSI episodes. Overall, S. aureus (16.5 %, 300) was the most frequent pathogen, followed by E. coli (15.1 %, 276), coagulase-negative staphylococci (CoNS, 12.9 %, 235), S. pneumoniae (11.1 %, 202) and non-E. coli Enterobacteriaceae (8.7 %, 159). S. aureus and E. coli showed similar frequencies in all of the variables analyzed (e.g., hospital acquisition, hospital type, medical specialty). The proportion of these microorganisms did not change over time, resistance rates remained low (4.3 % methicillin resistance in S. aureus; 7.3 % third-/fourth-generation cephalosporin resistance in E. coli), and no significant resistance trends were observed. We observed a 50 % increase of CoNS BSIs from 2008 (9.8 %, 27) to 2014 (15.2 %, 46, p value for trend = 0.03). S. pneumoniae decreased from 17.5 % (48) to 6.6 % (20) during that timeframe (p for trend = 0.007). S. aureus and E. coli remained the most significant pathogens among pediatric BSIs in Switzerland, exhibiting low resistance rates. CoNS accounted for a greater proportion of BSIs over time. The decrease in bacteremic pneumococcal infections can likely be attributed to the introduction of the 13-valent conjugate vaccine in 2011.



Similar content being viewed by others
References
Wilson J, Elgohari S, Livermore DM et al (2011) Trends among pathogens reported as causing bacteraemia in England, 2004–2008. Clin Microb Infect 17:451–458
Skogberg K, Lyytikainen O, Ollgren J, Nuorti JP, Ruutu P (2012) Population-based burden of bloodstream infections in Finland. Clin Microb Infect 18:E170–E176
Anderson DJ, Moehring RW, Sloane R et al (2014) Bloodstream infections in community hospitals in the 21st century: a multicenter cohort study. PLoS One 9:e91713
Henderson KL, Johnson AP, Muller-Pebody B, Charlett A, Gilbert R, Sharland M (2010) The changing aetiology of paediatric bacteraemia in England and Wales, 1998–2007. J Med Microbiol 59:213–219
Laupland KB, Gregson DB, Vanderkooi OG, Ross T, Kellner JD (2009) The changing burden of pediatric bloodstream infections in Calgary, Canada, 2000–2006. Pediatr Infect Dis J 28:114–117
Larru B, Gong W, Vendetti N et al (2016) Bloodstream infections in hospitalized children: epidemiology and antimicrobial susceptibilities. Pediatr Infect Dis J 35(5):507–510
Bundesamt für Gesundheit (BAG), (Federal Office of Public Health) (2015) Impfempfehlungen (vaccine recommendations). Available online from: http://www.bagadminch. Accessed 25 November 2015
De Kraker ME, Jarlier V, Monen JC, Heuer OE, van de Sande N, Grundmann H (2013) The changing epidemiology of bacteraemias in Europe: trends from the European Antimicrobial Resistance Surveillance System. Clin Microb Infect 19:860–868
Anresis.ch. Swiss Centre for Antibiotic Resistance (2016) Bern: Institut für Infektionskrankheiten Universität Bern. Available online from: http://www.anresisch/en/index.html. Accessed 1 June 2016
Bundesamt für Gesundheit (BAG), (Federal Office of Public Health) (2014) Spitalstatistiken. (Hospital statistics). Available from: http://www.bag.admin.ch/index.html
Asgeirsson H, Gudlaugsson O, Kristinsson KG et al (2015) Low mortality of Staphylococcus aureus bacteremia in Icelandic children: nationwide study on incidence and outcome. Pediatr Infect Dis J 34:140–144
Naidoo R, Nuttall J, Whitelaw A, Eley B (2013) Epidemiology of Staphylococcus aureus bacteraemia at a tertiary children’s hospital in Cape Town, South Africa. PLoS One 8:e78396
ECDC Surveillance Report (2015) Annual epidemiological report antimicrobial resistance and healthcare-associated infections 2014 (EARS-Net)
Bielicki JA, Lundin R, Sharland M, Project A (2015) Antibiotic resistance prevalence in routine bloodstream isolates from children’s hospitals varies substantially from adult surveillance data in Europe. Pediatr Infect Dis J 34:734–741
Eggimann P, Pittet D (2001) Nonantibibiotic measures for the prevention of Gram-positive infections. Clin Microb Infect 7 [Suppl 4]:91–99
Burdet C, Clermont O, Bonacorsi S et al (2014) Escherichia coli bacteremia in children: age and portal of entry are the main predictors of severity. Pediatr Infect Dis J 33:872–879
Sharland M, Subgroup SP (2007) The use of antibacterials in children: a report of the Specialist Advisory Committee on Antimicrobial Resistance (SACAR) Paediatric Subgroup. J Antimicrob Chemother 60 [Suppl 1]:i15–i26
Tamma PD, Robinson GL, Gerber JS et al (2013) Pediatric antimicrobial susceptibility trends across the United States. Infect Control Hosp Epidemiol 34:1244–1251
Pereira CA, Marra AR, Camargo LF et al (2013) Nosocomial bloodstream infections in Brazilian pediatric patients: microbiology, epidemiology, and clinical features. PLoS One 8:e68144
Hamer DH, Darmstadt GL, Carlin JB et al (2015) Etiology of bacteremia in young infants in six countries. Pediatr Infect Dis J 34:e1–e8
Biondi E, Evans R, Mischler M et al (2013) Epidemiology of bacteremia in febrile infants in the United States. Pediatrics 132:990–996
Marra AR, Camargo LF, Pignatari AC et al (2011) Nosocomial bloodstream infections in Brazilian hospitals: analysis of 2,563 cases from a prospective nationwide surveillance study. J Clin Microbiol 49:1866–1871
Farnham AC, Zimmerman CM, Papadouka V et al (2015) Invasive pneumococcal disease following the introduction of 13-valent conjugate vaccine in children in New York City from 2007 to 2012. JAMA Pediatr 169:646–652
Tagarro A, Benito A, Sanchez A et al (2016) Bacteremic pneumonia before and after withdrawal of 13-valent pneumococcal conjugate vaccine from a public vaccination program in Spain: a case-control study. J Pediatr 171:111–115.e3
Hauser C, Kronenberg A, Allemann A, Muhlemann K, Hilty M (2016) Serotype/serogroup-specific antibiotic non-susceptibility of invasive and non-invasive Streptococcus pneumoniae, Switzerland, 2004 to 2014. Euro Surveil. doi:10.2807/1560-7917.ES.2016.21.21.30239
Mueller M, Henle A, Droz S et al (2014) Intrapartum detection of Group B streptococci colonization by rapid PCR-test on labor ward. Eur J Obstet Gynecol Reprod Biol 176:137–141
Barcaite E, Bartusevicius A, Tameliene R, Kliucinskas M, Maleckiene L, Nadisauskiene R (2008) Prevalence of maternal group B streptococcal colonisation in European countries. Acta Obstet Gynecol Scand 87:260–271
Surbek D, Henle-Gross A, Seydoux J, Honegger CH, Irion O, Drack G (2012) Prophylaxe der early-onset-Neugeborenensepsis durch Streptokokken der Gruppe B. Gynecologie Suisse, Expertenbrief No 19
Giannoni E, Berger C, Stocker M et al (2016) Incidence and outcome of Group B streptococcal sepsis in infants in Switzerland. Pediatr Infect Dis J 35:222–224
Mermel LA (2015) Catheter tip cultures: are they really relegated to the archives of historical medical interest? Clin Infect Diseases 60:975
Acknowledgements
We thank all the microbiology laboratories participating in the ANRESIS network: Institute for Laboratory Medicine, Cantonal Hospital Aarau; Central Laboratory, Microbiology Section, Cantonal Hospital Baden; Clinical Microbiology, University Hospital Basel; Viollier AG, Basel; Laboratory Medicine EOLAB, Department of Microbiology, Bellinzona; Institute for Infectious Diseases, University Bern; Microbiology Laboratory, Unilabs, Coppet; Central Laboratory, Cantonal Hospital Graubünden; Microbiology Laboratory, Hospital Thurgau; Microbiology Laboratory Hôpital Fribourgeois, Fribourg; Bacteriology Laboratory, Geneva University Hospitals, Geneva; ADMED Microbiology, La Chaux-de-Fonds; Institute for Microbiology, Université de Lausanne; Centre for Laboratory Medicine, Cantonal Hospital Luzern; Centre for Laboratory Medicine, Cantonal Hospital Schaffhausen; Centre for Laboratory Medicine Dr Risch, Schaan; Central Institute, Hôpitaux Valaisans (ICHV), Sitten; Centre of Laboratory Medicine St Gallen; Institute for Medical Microbiology, University Hospital Zürich; Laboratory for Infectious Diseases, University Children’s Hospital Zürich
We also thank the steering committee of the ANRESIS network.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Funding
The ANRESIS database is funded by the Federal Office of Public Health, the Conference of Cantonal Health Ministers, and the University of Bern, Switzerland.
Conflicts of interest
The authors declare that they have no conflicts of interest
Ethical approval
This analysis was carried out on routinely collected, anonymous, nongenetic surveillance data; thus, ethical consent was not required according to the Swiss law for research on humans.
Informed consent
No clinical data were included
Additional information
J. Marschall and A. Kronenberg contributed equally to this work
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 24 kb)
Swiss Centre for Antibiotic resistance (ANRESIS)
Swiss Centre for Antibiotic resistance (ANRESIS)
R. Auckenthaler, Synlab Suisse, Switzerland; A. Cherkaoui, Bacteriology Laboratory, Geneva University Hospitals, Switzerland; M. Dolina, Department of Microbiology, EOLAB, Bellinzona, Switzerland; O. Dubuis, Viollier AG, Basel, Switzerland; R. Frei, Clinical Microbiology Laboratory, University Hospital Basel, Switzerland; D. Koch, Federal Office of Public Health, Bern, Switzerland; A. Kronenberg, Institute for Infectious Diseases, University of Bern, Switzerland; S. Leib, Institute for Infectious Diseases, University of Bern, Switzerland; S. Luyet, Swiss Conference of the Cantonal Ministers of Public Health, Switzerland; P. Nordmann, Molecular and Medical Microbiology, Department of Medicine, University Fribourg, Switzerland; V. Perreten, Institute of Veterinary Bacteriology, University of Bern, Switzerland; J.-C. Piffaretti, Interlifescience, Massagno, Switzerland; G. Prod’hom, Institute of Microbiology, Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland; J. Schrenzel, Bacteriology Laboratory, Geneva University Hospitals, Geneva, Switzerland; A.F. Widmer, Division of Infectious Diseases and Hospital Epidemiology, University of Basel, Switzerland; G. Zanetti, Service of Hospital Preventive Medicine, Centre Hospitalier Universitaire Vaudois, Lausanne, Switzerland; R. Zbinden, Institute of Medical Microbiology, University of Zürich, Switzerland.
Rights and permissions
About this article
Cite this article
Buetti, N., Atkinson, A., Kottanattu, L. et al. Patterns and trends of pediatric bloodstream infections: a 7-year surveillance study. Eur J Clin Microbiol Infect Dis 36, 537–544 (2017). https://doi.org/10.1007/s10096-016-2830-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2830-6