Abstract
Ceftaroline is a broad-spectrum antibiotic with activity against methicillin-resistant Staphylococcus aureus (MRSA) strains. Ceftaroline susceptibility of an MRSA set archived between 1994 and 2003 in the Geneva University Hospitals detected a high percentage (66 %) of ceftaroline resistance in clonotypes ST228 and ST247 and correlated with mutations in PBP2a. The ceftaroline mechanism of action is based on the inhibition of PBP2a; thus, the identification of PBP2a mutations of recently circulating clonotypes in our institution was investigated. We analyzed ceftaroline susceptibility in MRSA isolates (2013 and 2014) and established that resistant strains correlated with PBP2a mutations and specific clonotypes. Ninety-six MRSA strains were analyzed from independent patients and were isolated from blood cultures (23 %), deep infections (38.5 %), and superficial (skin or wound) infections (38.5 %). This sample showed a ceftaroline minimum inhibitory concentration (MIC) range between 0.25 and 2 μg/ml and disk diameters ranging from 10 to 30 mm, with a majority of strains showing diameters ≥20 mm. Based on the European Committee on Antimicrobial Susceptibility Testing (EUCAST) breakpoints, 76 % (73/96) of isolates showed susceptibility to ceftaroline. Nevertheless, we still observed 24 % (23/96) of resistant isolates (MIC = 2 μg/ml). All resistant isolates were assigned to clonotype ST228 and carried the N146K mutation in PBP2a. Only two ST228 isolates showed ceftaroline susceptibility. The decreasing percentage of ceftaroline-resistant isolates in our hospital can be explained by the decline of ST228 clonotype circulating in our hospital since 2008. We present evidence that ceftaroline is active against recent MRSA strains from our hospital; however, the presence of PBP2a variants in particular clonotypes may affect ceftaroline efficacy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Infections caused by methicillin-resistant Staphylococcus aureus (MRSA) are a major worldwide health problem. MRSA, initially identified as a nosocomial pathogen, is now responsible for both hospital- and community-acquired infections [1]. MRSA treatment options include glycopeptides and combination regimens [2], as well as new agents like daptomycin and last-generation cephalosporins (ceftobiprole and ceftaroline). Despite the availability of several antimicrobials, resistance to a particular antibiotic has repeatedly brought complications for the successful treatment of MRSA infections.
β-Lactam antibiotics were first developed to inhibit penicillin-binding proteins (PBPs) that catalyze cell wall biosynthesis. However, soon after their introduction, the efficacy of β-lactams was altered by S. aureus strains producing a β-lactamase enzyme or by horizontal acquisition of mecA, encoding the penicillin-binding protein PBP2a. PBP2a is not inhibited by β-lactams and can consequently catalyze DD-transpeptidation and cooperate with the PBP2 transglycosylase in peptidoglycan biosynthesis [3, 4].
Ceftaroline is a novel β-lactam broad-spectrum cephalosporin, capable of inhibiting PBP2a. Its anti-MRSA activity shows an MIC90 of around 1–2 μg/ml and has been approved for the treatment of complicated skin and soft tissue infections and community-acquired pneumonia [5–7]. Several studies have shown decreased susceptibility of MRSA to ceftaroline (EUCAST MIC values of > 1 μg/ml or CLSI MIC ≥ 4 μg/ml) in sporadic cases and limited to specific sequence types (STs) [8–12]. Recently, high-level ceftaroline resistance (MIC > 32 μg/ml) was observed during sustained MRSA bacteremia treated with ceftaroline [13]. Low-level resistance to ceftaroline is associated with mutations in PBP2a found in both the allosteric domain (N146K, E150K, N204K, E239K, G246E) or the transpeptidase domain (H351N, Y446N, E447) [3, 8, 13–17].
While high-level ceftaroline resistance can be explained by mutations in the transpeptidase domain that alter the active site geometry, low-level resistance associated with mutations within the allosteric site was explained by a novel allosteric modulation of the active site [15, 18–20]. Ceftaroline binds to the PBP2a allosteric site at therapeutic concentrations and triggers the opening and acylation of the active site by a second ceftaroline molecule [7, 20]. Mutations within the PBP2a allosteric domain alter the triggering mechanism and possibly affect protein–protein interactions needed for peptidoglycan biosynthesis [7, 14, 19, 21–23]. Additional factors contributing to ceftaroline resistance remain to be analyzed [24]. Surprisingly, reduced susceptibility has been described in clinical S. aureus isolates predating the commercial introduction of ceftaroline [8, 25] and in countries where ceftaroline is not commercially available [17].
Our previous study showed that decreased ceftaroline susceptibility was linked to circulating clonotypes ST228 and ST247 carrying mutations in the allosteric domain of PBP2a [8]. Since there has been a major change in MRSA epidemiology at our institution during the last 5 years [26], the analysis of ceftaroline susceptibility and mutations in PBP2a of contemporary circulating MRSA isolates in our institution was undertaken. MRSA isolates from 2013 to 2014 causing either soft tissue infections or bloodstream infections were examined.
Materials and methods
Bacterial strains and susceptibility testing
A collection of 96 independent MRSA strains archived from 2013 to 2014 and representing bloodstream, deep tissue, and superficial infection samples were tested. The methicillin-susceptible S. aureus (MSSA) and ceftaroline-susceptible strain ATCC29213, MIC 0.25 μg/ml, was used as the EUCAST standard quality control strain. Standardized procedures were as previously described [8] and determined according to EUCAST recommendations.
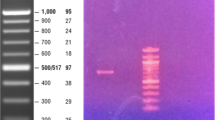
mecA gene sequencing
Genomic DNA (gDNA) was prepared as previously described [27] and mecA was amplified by polymerase chain reaction (PCR) (3 Kb) using specific primers: seq_meclocus-F 5′ TAAGGGAGAAGTAACAGCAC 3′ and seq_meclocus-R 5′ ATCGCCCAAAGCTTCTTTAG 3′. PCR fragments were sequenced using appropriate primers within mecA. Sequence alignments were performed using Clustal Omega and mecA reference sequences from N315 (SA0038) and COL (SACOL0033).
MLVA genotyping
Each tested MRSA was analyzed by a rapid genotyping assay (MLVA) [28]. The genotype of each strain was deduced by comparison with profiles obtained with well-characterized standard isolates.
Results
Determination of ceftaroline susceptibility in the MRSA strain collection (2013–2014) of Geneva University Hospitals
A previous study from our laboratory found a high rate of ceftaroline non-susceptibility in a collection of MRSA strains recovered from bloodstream infections during the period 1994–2003 [8]. To determine if ceftaroline resistance was still prevalent in our institution, we examined the ceftaroline susceptibility of 96 MRSA isolates archived in 2013–2014, using both disk diffusion and microdilution MIC methods. The specimen sources included 37 deep wound infections (38.5 %), 37 superficial (skin or wound) infections (38.5 %), and 22 bloodstream infection (23 %) isolates. Using ceftaroline 5 μg disks, our strain collection showed mean diameters ranging from 10 to 30 mm (Table 1), with a majority (79 %) of isolates (76/96) showing diameters ≥20 mm, but 21 % of isolates (20/96) showing a diameter <20 mm in at least three independent measurements (EUCAST breakpoints S ≥ 20 and R < 20 mm).
MIC determinations are required to confirm the susceptibility of strains showing disk diameters between 19 and 21 mm, according to the EUCAST guidelines. All strains were tested by the microdilution assay by three independent measurements (Table 1). For all strains tested, the disk diffusion results were in agreement with the MIC microdilution assays. The isolates with diameters 19 or 20 mm were all confirmed to be resistant by MIC microdilution, while those showing diameters of 21 mm were all confirmed as susceptible.
Overall, this strain set showed a ceftaroline MIC range between 0.25 and 2 μg/ml and 0.25 and 4 μg/ml at 24 and 48 h of incubation, respectively (Table 1). The frequency of MIC distribution for ceftaroline was 8.3, 52.1, 15.6, and 24 % for isolates showing an MIC of 0.25, 0.5, 1, and 2 μg/ml, respectively. A large proportion (73/96; 76 %) of isolates showed susceptibility to ceftaroline (EUCAST microdilution breakpoints S ≤ 1 and R > 1 μg/ml), with the majority (50/96) showing an MIC value of 0.5 μg/ml. Nevertheless, we still observed an elevated proportion (23/96; 24 %) of isolates showing an MIC of 2 μg/ml (at 24 h), thus considered resistant (Table 1).
PBP2a allosteric site mutations correlate with reduced ceftaroline susceptibility
The previously published ceftaroline-resistant strains from our hospital (the 1994–2003 collection) principally belong to clonotypes ST228 and ST247 [8]. The most plausible hypothesis to explain the presence of resistant strains in our 2013–2014 collection is that they represent bacterial clones belonging to the ST228 or ST247 typing family and carrying PBP2a mutations [8, 25]. Accordingly, MRSA isolates were subjected to MLST determination and PBP2a (mecA) sequence analysis. Isolates were first subjected to multiple-locus variable-number tandem repeat analysis (MLVA), a rapid genotyping assay allowing assessment of genomic content and assignment of MLST type [28, 29]. The STs of all strains are presented in Table 1.
PBP2a (mecA) sequence analysis was next performed (Table 2). PBP2a sequences from our strain collection were compared to the previously published Greek strain sequences and amino acid changes were annotated [16] (Table 2). Interestingly, and consistent with our hypothesis, all resistant strains (MIC = 2 μg/ml) were unambiguously assigned to ST228 and carried the PBP2a N146K mutation. In contrast, the majority of susceptible strains were all assigned to other STs (ST1, ST5, ST8, ST30, ST80, ST93, ST105, and ST125). Of note, two isolates from the 25 ST228 isolates show ceftaroline susceptibility, but also carry the N146K mutation, suggesting that this mutation alone might not be sufficient to generate ceftaroline resistance in certain circumstances. We found no other PBP2a mutation in our ceftaroline-resistant subset. In the ceftaroline-susceptible non-ST228 isolates, the only PBP2a mutations identified were G246E, found in four isolates (3 out of 10 mecA sequenced isolates). No G246E mutation was found in ceftaroline-resistant isolates. This corroborates other studies where no influence on the ceftaroline susceptibility of this mutation could be associated with ceftaroline susceptibility profiles [15, 17].
Analysis by sample type
We found ceftaroline-resistant isolates irrespective of the anatomical specimen source. The resistance analysis by sample type reveals that 31.8 % (7/22) of resistant bacteria were isolated from bloodstream infections, 29.7 % (11/37) from deep infections, and 13.5 % (5/37) from superficial soft tissue/wound infections. Comparing isolates from superficial infections with a resistance rate of 13.5 % (5/37) to more invasive isolates with a resistance rate of 30.5 % (18/59), it might be inferred that more severe infections are correlated to higher resistance levels. This result is linked to the higher prevalence of the ST228 clonotype in deep wounds and bloodstream infection than in superficial wound specimens. Thus, interestingly, the ST228 hospital-acquired MRSA strain is more frequent in bloodstream infections and deep wound infections than in community-acquired infections, such as skin and superficial wound infection.
Discussion
Ceftaroline-resistant strains (MIC of 2 μg/ml) were previously reported and identified in a few clonotypes, including ST228, ST247, and ST239 [8, 15, 21, 25, 30]. In 2015, we reported a high percentage (66 %) of ceftaroline resistance in an HUG bacterial collection first assembled to monitor the emergence of intermediate glycopeptide resistance [8, 31]. The detection of ceftaroline resistance among ST228 and ST247 clonotypes in this archived set prompted us to examine contemporary MRSA strains from our institution, not biased by prior screening for intermediate glycopeptide resistance. To what extent recent ST228 strains display reduced susceptibility to ceftaroline is an important consideration. Our current study was further motivated by the fact that ST228 has been endemic since 1998 in our institution, but epidemiological changes have been observed over the last 5–8 years, with gradual decline of ST228 and replacement by other clonotypes [14, 32] and, furthermore, by the potential use in clinical practice of this drug licensed in Switzerland in 2013, but which has not been used in our hospital to date.
The majority of 2013–2014 MRSA tested in the present study were found to be susceptible to ceftaroline, showing a modal MIC of 0.5 μg/ml; however, we observed 24 % resistant isolates (MIC = 2 μg/ml). The percentage of resistance we report in both studies is subject to cautious interpretation, since the current strain set may not be representative of an unbiased sampling since only certain infection types were analyzed. A second explanation for the lower percentage of resistant strains in the 2013–2014 compared to the 1994–2003 strain set can be the fact that resistance appears to be strongly linked with ST228, a clonotype gradually declining in recent years in our hospital [14, 32].
Although the majority of tested 2013–2014 HUG strains were found to be susceptible to ceftaroline, it is noteworthy that all resistant isolates were ST228. Ceftaroline-resistant HUG ST228 strains are strongly correlated with the N146K mutation present in the PBP2a allosteric domain. Together with E150K and E239K, the N146K mutation is one of the most prevalent mutations in isolates exhibiting a ceftaroline MIC of 2 μg/ml (including Italy, Hungary, Russia, Spain, and Turkey) [15, 22]. This mutation was previously detected in the ST228 bacterial strains collected in the interval 1998–2003 in our hospital and through 2003–2008 in the University Hospital of Lausanne [8]. It is unknown how the South German clone present in our hospital acquired PBP2a mutation. Whether some MRSA clonotypes, such as ST228, are more amenable to genetic variation is unknown. Since different missense mutations in PBP2a are found in several ST228 strains, it is probable that independent events occurred to produce this observed PBP2a allotype variation [8, 15]. ST228, even if diminishing in prevalence over the last decade in Switzerland, was still responsible for a large part of the non-community-acquired MRSA infections in the 2013–2014 period, which represents a significant concern.
Mutations in the allosteric domain of PBP2a are thought to confer low-level ceftaroline resistance by gating the active site channel [19]. In some cases, genotypic analysis revealed mutation within mecA, but the strain, nevertheless, displayed susceptibility to ceftaroline [8]. An important consideration is that proper transcriptional expression of mecA, together with PBP2a’s posttranslational export, maturation, and positioning, are crucial steps that govern PBP2a function. Whereas the transcriptional regulation of mecA is clearly multifactorial [4], only recently have reports highlighted the importance of additional factors such as PrsA that affect PBP2a maturation [33, 34]. Taken in this light, the presence of certain mutations within the PBP2a allosteric domain may not evoke resistance because of expression constraints. Alternatively, some strains showing a ceftaroline MIC of 2 μg/ml show wild-type PBP2a sequence, raising the possibility that additional factors can influence ceftaroline susceptibility. Notably, mutations in clpX, stp1, and prsA, as well as the pbp4 promoter, appear to be associated with ceftaroline resistance [24, 34]. Further genetic studies must identify genes implicated in ceftaroline resistance and define how particularly allosteric domain mutations differentially impact the expression of ceftaroline resistance.
References
Von Dach E, Diene SM, Fankhauser C, Schrenzel J, Harbarth S, François P (2016) Comparative genomics of community-associated methicillin-resistant Staphylococcus aureus shows the emergence of clone ST8-USA300 in Geneva, Switzerland. J Infect Dis 213(9):1370–1379. doi:10.1093/infdis/jiv489
Harbarth S, von Dach E, Pagani L, Macedo-Vinas M, Huttner B, Olearo F, Emonet S, Uçkay I (2015) Randomized non-inferiority trial to compare trimethoprim/sulfamethoxazole plus rifampicin versus linezolid for the treatment of MRSA infection. J Antimicrob Chemother 70(1):264–272. doi:10.1093/jac/dku352
Harrison EM, Ba X, Blane B, Ellington MJ, Loeffler A, Hill RL, Holmes MA, Peacock SJ (2016) PBP2a substitutions linked to ceftaroline resistance in MRSA isolates from the UK. J Antimicrob Chemother 71(1):268–269. doi:10.1093/jac/dkv317
Peacock SJ, Paterson GK (2015) Mechanisms of methicillin resistance in Staphylococcus aureus. Annu Rev Biochem 84:577–601. doi:10.1146/annurev-biochem-060614-034516
Zhong NS, Sun T, Zhuo C, D’Souza G, Lee SH, Lan NH, Chiang CH, Wilson D, Sun F, Iaconis J, Melnick D (2015) Ceftaroline fosamil versus ceftriaxone for the treatment of Asian patients with community-acquired pneumonia: a randomised, controlled, double-blind, phase 3, non-inferiority with nested superiority trial. Lancet Infect Dis 15(2):161–171. doi:10.1016/S1473-3099(14)71018-7
Sader HS, Farrell DJ, Flamm RK, Jones RN (2016) Antimicrobial activity of ceftaroline tested against Staphylococcus aureus from surgical skin and skin structure infections in US medical centers. Surg Infect 17(4):443–447. doi:10.1089/sur.2015.209
Fishovitz J, Rojas-Altuve A, Otero LH, Dawley M, Carrasco-López C, Chang M, Hermoso JA, Mobashery S (2014) Disruption of allosteric response as an unprecedented mechanism of resistance to antibiotics. J Am Chem Soc 136(28):9814–9817. doi:10.1021/ja5030657
Kelley WL, Jousselin A, Barras C, Lelong E, Renzoni A (2015) Missense mutations in PBP2A Affecting ceftaroline susceptibility detected in epidemic hospital-acquired methicillin-resistant Staphylococcus aureus clonotypes ST228 and ST247 in Western Switzerland archived since 1998. Antimicrob Agents Chemother 59(4):1922–1930. doi:10.1128/AAC.04068-14
Sader HS, Flamm RK, Jones RN (2013) Antimicrobial activity of ceftaroline and comparator agents tested against bacterial isolates causing skin and soft tissue infections and community-acquired respiratory tract infections isolated from the Asia-Pacific region and South Africa (2010). Diagn Microbiol Infect Dis 76(1):61–68. doi:10.1016/j.diagmicrobio.2013.01.005
Biedenbach DJ, Alm RA, Lahiri SD, Reiszner E, Hoban DJ, Sahm DF, Bouchillon SK, Ambler JE (2015) In vitro activity of ceftaroline against Staphylococcus aureus isolated in 2012 from Asia-Pacific countries as part of the AWARE Surveillance Program. Antimicrob Agents Chemother 60(1):343–347. doi:10.1128/AAC.01867-15
Karlowsky JA, Biedenbach DJ, Bouchillon SK, Iaconis JP, Reiszner E, Sahm DF (2016) In vitro activity of ceftaroline against bacterial pathogens isolated from skin and soft tissue infections in Europe, Russia and Turkey in 2012: results from the Assessing Worldwide Antimicrobial Resistance Evaluation (AWARE) surveillance programme. J Antimicrob Chemother 71(1):162–169. doi:10.1093/jac/dkv311
Zhang H, Xiao M, Kong F, O’Sullivan MV, Mao LL, Zhao HR, Zhao Y, Wang H, Xu YC (2015) A multicentre study of meticillin-resistant Staphylococcus aureus in acute bacterial skin and skin-structure infections in China: susceptibility to ceftaroline and molecular epidemiology. Int J Antimicrob Agents 45(4):347–350. doi:10.1016/j.ijantimicag.2014.12.014
Long SW, Olsen RJ, Mehta SC, Palzkill T, Cernoch PL, Perez KK, Musick WL, Rosato AE, Musser JM (2014) PBP2a mutations causing high-level Ceftaroline resistance in clinical methicillin-resistant Staphylococcus aureus isolates. Antimicrob Agents Chemother 58(11):6668–6674. doi:10.1128/AAC.03622-14
Banerjee R, Gretes M, Basuino L, Strynadka N, Chambers HF (2008) In vitro selection and characterization of ceftobiprole-resistant methicillin-resistant Staphylococcus aureus. Antimicrob Agents Chemother 52(6):2089–2096. doi:10.1128/AAC.01403-07
Alm RA, McLaughlin RE, Kos VN, Sader HS, Iaconis JP, Lahiri SD (2014) Analysis of Staphylococcus aureus clinical isolates with reduced susceptibility to ceftaroline: an epidemiological and structural perspective. J Antimicrob Chemother 69(8):2065–2075. doi:10.1093/jac/dku114
Mendes RE, Tsakris A, Sader HS, Jones RN, Biek D, McGhee P, Appelbaum PC, Kosowska-Shick K (2012) Characterization of methicillin-resistant Staphylococcus aureus displaying increased MICs of ceftaroline. J Antimicrob Chemother 67(6):1321–1324. doi:10.1093/jac/dks069
Schaumburg F, Peters G, Alabi A, Becker K, Idelevich EA (2016) Missense mutations of PBP2a are associated with reduced susceptibility to ceftaroline and ceftobiprole in African MRSA. J Antimicrob Chemother 71(1):41–44. doi:10.1093/jac/dkv325
Otero LH, Rojas-Altuve A, Llarrull LI, Carrasco-López C, Kumarasiri M, Lastochkin E, Fishovitz J, Dawley M, Hesek D, Lee M, Johnson JW, Fisher JF, Chang M, Mobashery S, Hermoso JA (2013) How allosteric control of Staphylococcus aureus penicillin binding protein 2a enables methicillin resistance and physiological function. Proc Natl Acad Sci U S A 110(42):16808–16813. doi:10.1073/pnas.1300118110
Fishovitz J, Hermoso JA, Chang M, Mobashery S (2014) Penicillin-binding protein 2a of methicillin-resistant Staphylococcus aureus. IUBMB Life 66(8):572–577. doi:10.1002/iub.1289
Fishovitz J, Taghizadeh N, Fisher JF, Chang M, Mobashery S (2015) The Tipper–Strominger hypothesis and triggering of allostery in penicillin-binding protein 2a of methicillin-resistant Staphylococcus aureus (MRSA). J Am Chem Soc 137(20):6500–6505. doi:10.1021/jacs.5b01374
Lahiri SD, Alm RA (2016) Potential of Staphylococcus aureus isolates carrying different PBP2a alleles to develop resistance to ceftaroline. J Antimicrob Chemother 71(1):34–40. doi:10.1093/jac/dkv329
Lahiri SD, McLaughlin RE, Whiteaker JD, Ambler JE, Alm RA (2015) Molecular characterization of MRSA isolates bracketing the current EUCAST ceftaroline-susceptible breakpoint for Staphylococcus aureus: the role of PBP2a in the activity of ceftaroline. J Antimicrob Chemother 70(9):2488–2498. doi:10.1093/jac/dkv131
Fernandez R, Paz LI, Rosato RR, Rosato AE (2014) Ceftaroline is active against heteroresistant methicillin-resistant Staphylococcus aureus clinical strains despite associated mutational mechanisms and intermediate levels of resistance. Antimicrob Agents Chemother 58(10):5736–5746. doi:10.1128/AAC.03019-14
Greninger AL, Chatterjee SS, Chan LC, Hamilton SM, Chambers HF, Chiu CY (2016) Whole-genome sequencing of methicillin-resistant Staphylococcus aureus resistant to fifth-generation cephalosporins reveals potential non-mecA mechanisms of resistance. PLoS One 11(2), e0149541. doi:10.1371/journal.pone.0149541
Strommenger B, Layer F, Klare I, Werner G (2015) Pre-use susceptibility to ceftaroline in clinical Staphylococcus aureus isolates from Germany: is there a non-susceptible pool to be selected? PLoS One 10(5), e0125864. doi:10.1371/journal.pone.0125864
Fankhauser C, Schrenzel J, Francois P, Pittet D, Harbarth S (2015) Secular trends of methicillin-resistant Staphylococcus aureus (MRSA) at Geneva University Hospitals (HUG) over a 14-year period. In: Antimicrobial Resistance and Infection Control: Abstracts from the 3rd International Conference on Prevention and Infection Control (ICPIC 2015), Geneva, Switzerland, June 2015. Abstract 09
Renzoni A, Huggler E, Kelley WL, Lew D, Vaudaux P (2009) Increased uptake and improved intracellular survival of a teicoplanin-resistant mutant of methicillin-resistant Staphylococcus aureus in non-professional phagocytes. Chemotherapy 55(3):183–188. doi:10.1159/000215304
Francois P, Huyghe A, Charbonnier Y, Bento M, Herzig S, Topolski I, Fleury B, Lew D, Vaudaux P, Harbarth S, van Leeuwen W, van Belkum A, Blanc DS, Pittet D, Schrenzel J (2005) Use of an automated multiple-locus, variable-number tandem repeat-based method for rapid and high-throughput genotyping of Staphylococcus aureus isolates. J Clin Microbiol 43(7):3346–3355. doi:10.1128/JCM.43.7.3346-3355.2005
Koessler T, Francois P, Charbonnier Y, Huyghe A, Bento M, Dharan S, Renzi G, Lew D, Harbarth S, Pittet D, Schrenzel J (2006) Use of oligoarrays for characterization of community-onset methicillin-resistant Staphylococcus aureus. J Clin Microbiol 44(3):1040–1048. doi:10.1128/JCM.44.3.1040-1048.2006
Campanile F, Bongiorno D, Borbone S, Stefani S (2009) Hospital-associated methicillin-resistant Staphylococcus aureus (HA-MRSA) in Italy. Ann Clin Microbiol Antimicrob 8:22. doi:10.1186/1476-0711-8-22
Vaudaux P, Huggler E, Bernard L, Ferry T, Renzoni A, Lew DP (2010) Underestimation of vancomycin and teicoplanin MICs by broth microdilution leads to underdetection of glycopeptide-intermediate isolates of Staphylococcus aureus. Antimicrob Agents Chemother 54(9):3861–3870. doi:10.1128/AAC.00269-10
Francois P, Harbarth S, Huyghe A, Renzi G, Bento M, Gervaix A, Pittet D, Schrenzel J (2008) Methicillin-resistant Staphylococcus aureus, Geneva, Switzerland, 1993–2005. Emerg Infect Dis 14(2):304–307. doi:10.3201/eid1402.070229
Jousselin A, Renzoni A, Andrey DO, Monod A, Lew DP, Kelley WL (2012) The posttranslocational chaperone lipoprotein PrsA is involved in both glycopeptide and oxacillin resistance in Staphylococcus aureus. Antimicrob Agents Chemother 56(7):3629–3640. doi:10.1128/AAC.06264-11
Jousselin A, Manzano C, Biette A, Reed P, Pinho MG, Rosato AE, Kelley WL, Renzoni A (2015) The Staphylococcus aureus chaperone PrsA is a new auxiliary factor of oxacillin resistance affecting penicillin-binding protein 2A. Antimicrob Agents Chemother 60(3):1656–1666. doi:10.1128/AAC.02333-15
Acknowledgments
The authors thank Pierre Vaudaux for his critical comments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by an AstraZeneca investigator-initiated grant (no. 2793), the Fondation Privée des HUG (AR-S27), the Swiss National Science Foundation grants (AR 310030-149762, WLK 10030-146540, PF 31003A-153474/1), and a Novartis Foundation grant (no. 15A040). SH received support from the Innovative Medicines Initiative Joint Undertaking under the Combatting Bacterial Resistance in Europe (COMBACTE) grant agreement no. 115523, resources of which are composed of financial contribution from the EU’s Seventh Framework Programme (FP7/2007–2013) and the European Federation of Pharmaceutical Industries and Associations (EFPIA) companies’ in-kind contribution. The funders had no role in the study design, data collection, interpretation, or the decision to submit the work for publication.
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Andrey, D.O., François, P., Manzano, C. et al. Antimicrobial activity of ceftaroline against methicillin-resistant Staphylococcus aureus (MRSA) isolates collected in 2013–2014 at the Geneva University Hospitals. Eur J Clin Microbiol Infect Dis 36, 343–350 (2017). https://doi.org/10.1007/s10096-016-2807-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-016-2807-5