Abstract
Tigecycline (TG) has been shown to be active in vitro against Acinetobacter baumannii, although data on the clinical efficacy of TG alone or in combination for the treatment of infections due to multidrug-resistant A. baumannii (MDRAB) remain limited. The purpose of this study was to investigate the clinical outcomes of patients with healthcare-associated infections (HAIs) caused by MDRAB who were treated with imipenem/cilastatin and sulbactam, and TG alone or in combination with other antibiotics. A total of 386 patients with HAIs caused by MDRAB were retrospectively analyzed and grouped into TG and non-TG groups, depending on whether they received TG treatment. Of the 266 patients in the TG group, 108 were treated with TG alone and 158 were treated with TG in combination with ceftazidime, ceftriaxone, piperacillin/tazobactam, or a carbapenem. All 120 patients in the non-TG group were treated with imipenem/cilastatin and sulbactam. The primary outcome measure was 30-day mortality after TG treatment and the secondary outcome was clinical outcome. There were no significant differences in survival rates between the two groups. However, the rate of unfavorable outcome was significantly lower (p < 0.05) among patients in the TG group than among patients in the non-TG group. The most significant predictor of unfavorable outcome was sepsis, whereas TG treatment and microbial eradication were the most significant predictors of favorable outcomes. Our study represents the largest study of patients with MDRAB infection treated with TG and expands our understanding of the role of TG therapy alone or in combination with other agents for the treatment of HAI caused by MDRAB.
Similar content being viewed by others
Introduction
Healthcare-associated infection (HAI), an important cause of morbidity and mortality in the hospital setting, has a negative impact on the cost of healthcare worldwide [1, 2]. The rapid increase in the occurrence of HAI, especially in intensive care units (ICUs) is due, in part, to the emergence of multidrug resistance [3]. Although the epidemiology of multidrug-resistant (MDR) organisms is complex, it is accepted that the excessive use of broad-spectrum antibiotics has contributed to this increasing problem [4]. Multidrug-resistant Acinetobacter baumannii (MDRAB) has emerged as one of the major challenges in the healthcare setting, and is known to cause nosocomial pneumonia, bacteremia, meningitis, urinary tract infections, and wound infections [5, 6]. Infection with MDRAB has been linked with poor clinical outcomes [7], increased morbidity, and prolonged duration of hospital stay [8].
Tigecycline (TG), part of a new class of antibiotics called glycylcyclines, has been shown to bind efficiently to bacterial ribosomes [9]. TG has been recently licensed to treat skin and soft tissue as well as intra-abdominal infections [10, 11] and is active against a broad spectrum of bacteria in vivo, including resistant aerobic and fermentative Gram-positive and Gram-negative bacteria and anaerobes [12–14]. Resistance to TG is not common, although TG has limited activity against Pseudomonas aeruginosa and Proteus species [15].
Data from a limited number of patients suggest that TG is effective for the treatment of infections caused by MDR Enterobacteriaceae [16]. TG has also been shown to be active in vitro against A. baumannii, although data on the clinical efficacy remains limited [14, 17]. However, the effect of TG on ventilator-associated pneumonia or bacteremia and bloodstream infection remains inconclusive [6, 18, 19]. In addition, studies on the effects of TG are often clouded by the effects of combination antibiotic therapy [18, 19].
In this study, our primary objective was to investigate the role of TG on the outcomes of patients treated with TG for serious HAIs caused by MDRAB. The secondary objective was to investigate the clinical outcomes of these patients.
Materials and methods
Patient recruitment
We retrospectively reviewed the records of patients admitted to the Chung Shan Medical University Hospital, Taiwan, from January 2007 to June 2011. All patients admitted to the hospital for more than 48 h were monitored for HAI, which was diagnosed based on the Centers for Disease Control and Prevention (CDC) definition of nosocomial infections [20, 21]. Study participants diagnosed with HAIs caused by MDRAB were divided into two treatment groups: (1) patients in the TG group were treated with TG alone (100 mg intravenous TG initially, followed by 50-mg doses intravenously administered twice daily, for at least 5 days) or TG plus a carbapenem or a third-generation cephalosporin (ceftazidime or ceftriaxone) or piperacillin/tazobactam; (2) patients in the non-TG group were treated with a carbapenem and sulbactam (imipenem/cilastatin 500 mg and sulbactam 1-g doses intravenously administered every 6 h daily, for at least 5 days). The study protocols were approved by the Institutional Review Board (IRB) of the Chung Shan Medical University Hospital and a waiver of informed consent was obtained from the IRB for this retrospective study (no. CS1105).
Inclusion criteria were: (1) age >20 years; (2) a confirmed diagnosis of HAI caused by MDRAB; (3) receipt of empirical treatment or concordant therapy with TG after microbiologic data had been obtained for cultures susceptible to TG in vitro; and (4) receipt of empirical treatment or concordant therapy with imipenem/cilastatin and sulbactam after microbiologic data had been identified for MDRAB isolates. Exclusion criteria were: (1) the presence of HAI caused by non-Gram-negative bacteria; (2) severe liver failure; (3) the presence of community-associated infections; or (4) the presence of HAI caused by Gram-negative bacteria which was not treated with TG or imipenem/cilastatin and sulbactam. In addition to data on patient characteristics, we also obtained laboratory data, Glasgow Coma Scale (GCS) scores [22], Acute Physiology and Chronic Health Evaluation (APACHE) II scores [23], and Sequential Organ Failure Assessment (SOFA) scores [24] prior to receiving TG. Other risk factors such as recent comorbidities in the 6 months prior to this infection during this hospital admission (underlying illness), sepsis [25], duration of hospitalization, duration of ICU stay, history of recent invasive procedures in the 6 months prior to this infection during this hospital admission, the presence of invasive devices, prior antimicrobial therapy, immunosuppressive drug use, and the presence of bacteremia due to MDRAB, or co-infection with fungus or Pseudomonas, were also collected from patient records.
Bacteriological identification and antimicrobial susceptibility testing
A. baumannii was identified using standard biochemistry testing [26] and confirmed using the Vitek 2 system (bioMérieux Inc., La Balme les Grottes, France) and API 20 E strips (bioMérieux). Antimicrobial susceptibility testing of A. baumannii isolates to antimicrobial agents, including TG, was performed using the Kirby–Bauer disk diffusion method and interpreted as recommended by the Clinical and Laboratory Standards Institute (CLSI) [27–29]. Escherichia coli ATCC 25922 and Pseudomonas aeruginosa ATCC 27853 were used as quality control strains. Susceptibility to colistin is not routinely evaluated in our clinical microbiology laboratory. MDRAB was defined as an A. baumannii isolate resistant to all currently available systemic antimicrobial agents, with the exception of colistin and TG, including cephalosporins (cefotaxime and ceftazidime), penicillins, piperacillin/tazobactam, aztreonam, carbapenems (imipenem and meropenem), aminoglycosides (gentamicin and amikacin), fluoroquinolones (ciprofloxacin and levofloxacin), and sulbactam [26].
Microbiological data collection
All microbiological data were collected from medical records. Clinical specimens evaluated included blood, sputum, urine, pleural effusion, ascites, synovial joint fluid, pus, and cerebral spinal fluid. All specimens were subjected to standard microbiological procedures in our hospital. Samples of sputum, bronchoalveolar lavage (BAL) fluid, and tracheal aspirate fluid were cultured and subjected to Gram staining to evaluate the presence of white blood cells (WBCs) and microorganisms. The causative pathogen was defined as: (1) a single microorganism with a bacterial density >104 colony-forming units (CFU)/mL in tracheal aspirates or BAL; (2) more than 25 polymorphonuclear cells and fewer than 10 epithelial cells per low-power field in sputum smears; (3) a single microorganism with a bacterial density >105 CFU/mL in wound cultures; or (4) a single microorganism with a bacterial density >105 CFU/mL and pyuria (>10 white blood cells/μL) in urine cultures. The definitions of complicated skin and soft tissue infections (cSSTIs) are based on CDC guidelines [21].
Primary bacteremia was defined as bacteremia associated with intravenous catheters, while secondary bacteremia was defined as bacteremia secondary to concomitant infections associated with urinary tract infection (UTI), cSSTI, complicated intra-abdominal infection (cIAI), or pneumonia [21]. Ventilator-associated pneumonia was diagnosed as healthcare-associated pneumonia based on CDC guidelines [21].
The primary outcome measure in this study was 30-day mortality after TG treatment. Differences in primary outcome were evaluated in patients with MDRAB-positive and in patients with negative blood cultures. The secondary outcome measure in this study was assessed as favorable and unfavorable responses. Favorable responses included: (1) a cure; (2) eradication of the causative pathogen; or (3) partial or complete improvement in clinical signs and symptoms. Unfavorable responses included a plateauing or deterioration in clinical signs and symptoms requiring a switch to other antimicrobials. Data on in-hospital mortality, 60-day mortality, and >60-day mortality were also collected.
Microbial eradication was defined as the absence of growth of the primary pathogen in 14-day surveillance cultures from the primary site of infection. Superinfections with bacteremia or fungemia were assessed during the period of or after TG treatment.
Statistical analysis
Continuous data are presented by the median and inter-quartile range (IQR), and categorical data are presented as count and percentage. Differences between the non-TG and TG groups in continuous data and categorical data were tested with the Mann–Whitney test and the Fisher’s exact test, respectively. We used Kaplan–Meier survival curves to show the cumulative survival rate of patients and the log-rank test to compare the survival rates of patients in the two groups. To further investigate the differences in 30-day mortality rate as well as clinical outcomes between the TG and non-TG groups while controlling for other clinical characteristics, the comparisons between the two groups were stratified by sepsis (no vs. yes), GCS (>9 vs. ≤9), SOFA (≤7 vs. >7), and APACHE II scores (≤21 vs. >21), respectively. Logistic regression analyses were performed to evaluate factors independently influencing unfavorable clinical outcomes (stationary or deterioration). Variables with a significant impact in the univariate logistic regression analyses and without severe multicollinearity were entered into a multivariate logistic regression model to identify factors independently influencing unfavorable clinical outcomes. The statistical hypothesis tests were two-sided and set at a significance level of 0.05. All statistical analyses were performed using the statistical software package SPSS (Version 15.0, SPSS Inc., Chicago, IL, USA).
Results
Patients
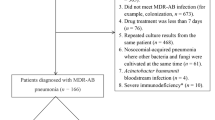
During the study period, a total of 496 patients with a diagnosis of HAI were recruited. Of these, 110 patients were excluded for the following reasons: one patient was younger than 18 years, 29 patients had non-Gram-negative bacteria infections, and 80 patients with infections not caused by MDRAB [including K. pneumoniae (n = 19), Escherichia coli (n = 17), extended-spectrum β-lactamase (ESBL)-producing K. pneumoniae (n = 14), Pseudomonas aeruginosa (n = 13), ESBL-producing E. coli (n = 2), Enterobacter aerogenes (n = 6), Stenotrophomonas maltophilia (n = 4), Proteus mirabilis (n = 3), and Sphingomonas paucimobilis (n = 2)] and were not treated with TG or imipenem/cilastatin and sulbactam. A total of 386 patients with HAIs due to MDRAB met the inclusion criteria and were included in the final analysis. These patients were stratified into two treatment groups (TG and non-TG), based on whether they received TG treatment. The TG group comprised 266 patients (108 were treated with TG alone and 158 were treated with TG in combination with ceftazidime, ceftriaxone, piperacillin/tazobactam, or a carbapenem). The non-TG group comprised 120 patients (all were treated with imipenem/cilastatin and sulbactam).
Clinical characteristics
There were no significant differences in age or gender between the non-TG and TG groups. Compared with the non-TG group, the TG group had a significantly higher rate of prior exposure to antibiotics (99.2 % vs. 93.3 %, p = 0.002) and a significantly lower incidence of Foley catheter insertion (64.7 % vs. 87.5 %, p < 0.001). The percentage of patients who required treatment in the ICU was significantly lower in the TG group (71.8 %) than in the non-TG group (87.5 %) (p < 0.001). In addition, the percentage of patients with fever was significantly lower in the TG group (16.5 %) than in the non-TG group (26.7 %) p = 0.027). Patients in the TG group also had significantly lower serum creatinine levels than patients in the non-TG group (1.4 mg/dL vs. 1.7 mg/dL, p = 0.02). Also, the TG group had a significantly lower percentage of patients with sepsis (42.5 % vs. 66.7 %, p < 0.001) and a significantly higher number of patients with heart disease (45.1 % vs. 33.3 %, p = 0.034) than the non-TG group. However, there were no significant differences in other laboratory data or disease severity measurements between the two groups (Table 1).
Microbiological analyses showed that the rate of concurrent infection was significantly higher in the TG group than in the non-TG group (13.2 % vs. 4.2 %, p = 0.006), but the rate of concurrent MDRAB infection and Candida infection was significantly lower in the TG group than in the non-TG group (65.4 % vs. 81.7 %, p < 0.001). We also found that the two groups differed significantly in the distribution of organisms isolated from the primary site of infection (Table 2). In addition, secondary bacteremia occurred in 40.8 % of patients who did not receive TG and in 19.5 % of patients who received TG (p < 0.001) (Table 2).
Patients in the TG group had a significantly shorter duration of antimicrobial use than patients in the non-TG group (8.0 days vs. 12.0 days, p < 0.001). Also, the percentage of patients in the TG group that switched to other antibiotics was significantly higher than that of patients in the non-TG group (53.8 % vs. 29.2 %, p < 0.001). Interestingly, the percentage of patients who showed evidence of microbial eradication was significantly lower in the TG group than in the non-TG group (1.1 % vs. 11.7 %, p < 0.001) (Table 3).
Evaluation of clinical outcomes
The percentage of patients with unfavorable outcome (stationary or deterioration) was significantly lower in the TG group than in the non-TG group (30.8 % vs. 50.0 %, p < 0.001). However, there were no significant differences in the number of infection-related deaths, length of hospital stay, or length of ICU stay between the two groups (Table 3). In addition, there were no significant differences in the survival rates between the TG and non-TG groups. In the TG group, the 3-month survival rate was 50.8 %, the 6-month survival rate was 45.9 %, and the 1-year survival rate was 42.4 %; the corresponding survival rates in the non-TG group were 47.3 %, 44.9 %, and 38.1 %, respectively.
Evaluation of factors influencing unfavorable clinical outcomes
The results of the univariate analysis showed that age, gender, comorbidities, fever, and infection sources did not have a significant impact on clinical outcome. However, the clinical outcome was significantly influenced by eight variables, including laboratory values of C-reactive protein and blood urea nitrogen, severity of sepsis, GCS and APACHE II scores, TG therapy, a switch to other antibiotics, and microbial eradication. These variables had no serious collinearity, and were used in our multivariate logistic regression model to determine factors independently influencing unfavorable clinical outcome. The results from the multivariate analysis showed that patients with sepsis were more likely to have unfavorable outcomes [odds ratio (OR) of 1.737] and that patients treated with TG were less likely to have unfavorable outcomes (ORs of 0.470 and 0.553 for patients treated with TG alone and TG plus other antibiotics, respectively). In addition, patients who switched to other antibiotics or had microbial eradication were less likely to have unfavorable outcomes (ORs of 0.468 and 0.155, respectively) (Table 4). We used logistic regression analyses to evaluate prior exposure to antibiotics as a risk factor for clinical outcome. We showed that 244 patients with prior antibiotic exposure in both groups had a favorable clinical outcome, while 142 patients had an unfavorable clinical outcome.
Patients with sepsis in the TG group were less likely to have unfavorable outcomes than patients with sepsis in the non-TG group (38.9 % vs. 57.5 %, p = 0.013). Patients in the TG group with a GCS score ≤9 were less likely to have unfavorable outcomes than patients with similar scores in the non-TG group (31.9 % vs. 56.2 %, p = 0.001). Also, patients in the TG group with a SOFA score >7 were less likely to have unfavorable outcomes than patients with similar SOFA scores in the non-TG group (33.9 % vs. 60.7 %, p = 0.002). Patients in the TG group with an APACHE II score >21 were also less likely to have unfavorable outcomes than patients with similar scores in the non-TG group (37.2 % vs. 59.7 %, p = 0.007).
Discussion
In this retrospective study, we evaluated the efficacy of TG (alone or in combination with other antimicrobial drugs) in patients with MDRAB HAIs. We showed that the TG and non-TG groups did not differ significantly in the number of infection-related deaths, length of hospital stay, or length of ICU stay. There were also no significant differences in the survival rates between the two groups. However, the percentage of patients with an unfavorable outcome was significantly lower in the TG group than in the non-TG group.
Different drug sensitivities in HAIs and community-acquired infections are dictated by differences in the genotypes and phenotypes of the pathogens involved [30]. Managing MDR pathogens is a growing challenge in the ICU setting, because of the especially vulnerable patient population and the high use of invasive procedures. The recent emergence of antimicrobial resistance in Acinetobacter spp. is an important problem in the ICU, because of its ability to survive in a hospital setting for prolonged periods of time. A. baumannii is thought to acquire antimicrobial resistance via a number of mechanisms, including the presence of antimicrobial-inactivating enzymes, reduced access to bacterial targets, and mutations altering bacterial targets [31], resulting in challenges in infection control as well as treatment. In this study, we determined the optimal treatment for patients with infections due to MDRAB, the efficacy of TG for treating MDRAB infections, and the efficacy of TG for treating seriously ill patients.
Glycylcyclines like TG are structurally similar to tetracyclines and inhibit the bacterial translation machinery [32]. There has been a recent focus on the use of TG for the treatment of HAI [33–36]. In this study, we demonstrated that the TG group had a significantly lower percentage of patients with unfavorable outcomes compared to the non-TG group (30.8 % vs. 50.0 %, p < 0.001). Previous studies have shown that, although TG alone is not superior to imipenem, TG in combination with ceftazidime is effective for patients with hospital-acquired pneumonia [37, 38]. TG monotherapy was also previously shown to be clinically ineffective for patients with MDRAB infections, although the rate of microbial eradication was high [39]. However, a larger case series study recently demonstrated a favorable clinical as well as microbiological response (73 % and 78 %, respectively) in patients with HAIs [33]. Our findings are consistent with those in this study, namely, that patients who received TG monotherapy and patients who received TG combination therapy had a significantly better clinical outcome than patients who did not receive TG treatment. It is important to note that our study enrolled a significantly higher proportion of seriously ill patients in the TG group who required ICU care prior to receiving TG treatment (71.8 %). In the present study, seriously ill patients with sepsis, high APACHE II scores, and high SOFA scores in the TG group were less likely to have unfavorable outcomes compared to patients in the non-TG group. Our findings are consistent with a previous study showing that seriously ill patients with APACHE II scores >21 who received TG for HAIs had a good clinical success rate (73 %) [33].
We found no significant difference in the survival rate between the two groups, possibly because the study participants in both groups were seriously ill patients with sepsis, high APACHE II scores, and high SOFA scores. In contrast, data from a previous meta-analyses study showed that TG treatment was associated with increased mortality [40]. These data suggest that it is important for clinicians to carefully consider when to administer TG to seriously ill patients with difficult-to-treat, resistant pathogens that are susceptible to TG in vitro [41].
Our multivariate analysis showed that sepsis and high APACHE II scores were risk factors for unfavorable outcome. However, patients in the TG group with sepsis, SOFA score >7, GCS score <9, and APACHE II score >21 were less likely to have unfavorable outcomes compared to patients with similar scores in the non-TG group. We suggest that this could be attributed to the pharmacokinetic (PK) and pharmacodynamic (PD) characteristics of TG. The lipophilic properties of TG play a role in the PK of TG, enabling rapid and extensive penetration into body tissue, and a high volume distribution (Vd) of approximately 7–10 L/kg [42]. Theoretically, plasma TG concentrations are unlikely to change when patients have increased Vd in a serious illness. In contrast, carbapenems are hydrophilic antibiotics with a low intracellular penetration, which would increase the Vd and decrease plasma concentrations in seriously ill patients [42]. Furthermore, the PD profile of TG has been shown to exhibit time-dependent bactericidal activity with a prolonged post-antibiotic effect that is likely to be correlated with its efficacy [42]. However, there is little information to support the concept of potentially altered PK/PD of TG in seriously ill patients.
Our data showed favorable microbiologic outcomes in the non-TG group compared to the TG group, and are consistent with a previous study that showed a poor correlation between microbiological clearance and clinical outcome in patients with MDRAB treated with TG [6]. Our data can be explained by the clinical characteristics of our study patients who presented with a higher proportion of pulmonary (64.7 %), bloodstream (18.0 %), and urinary tract (12.0 %) infections. Patients who are colonized or infected with A. baumannii can become a reservoir of infection. In fact, it has been shown that A. baumannii can colonize multiple body sites in hospitalized patients and can be isolated after more than 4 months from the patient’s respiratory tract [43]. The clinical use of TG for bloodstream infection remains controversial, since its rapid distribution from the bloodstream into tissues could result in TG serum concentrations which are sub-optimal for maximal antibacterial activity. Low concentrations of TG in urine also render it unsuitable to treat urinary tract infections [13, 14]. TG has been shown to be bacteriostatic against MDRAB, while imipenem has bactericidal activity against A. baumannii isolates [44]. However, the correlation between the microbiological clearance and in vitro antibacterial activity remains unclear with the limited amount of clinical data available.
In summary, we suggest that our data can be explained by: (1) the significantly shorter duration of antimicrobial use by patients in the TG group compared to patients in the non-TG group; (2) the high number of patients with pneumonia; and (3) the significantly higher percentage of patients in the TG group who switched to other antibiotics compared to the non-TG group.
While sulbactams and carbapenems continue to be the most widely used therapeutic options for patients with HAIs, tetracyclines, aminoglycosides, and polymyxins are also used either alone or in combination to combat A. baumannii infection [45]. A regimen of carbapenems plus sulbactam has previously demonstrated in vitro and in vivo activity against MDRAB and been used to treat MDRAB isolates [46, 47]. However, the increased use of carbapenem is associated with a risk of developing antimicrobial resistance in MDRAB and non-fermenters [48]. To the best of our knowledge, our study represents the largest study of patients with MDRAB infection treated with TG and imipenem plus sulbactam.
Our study design has a few important limitations. The retrospective nature of the study limited our ability to collect complete information on adverse events. A second limitation is that it is a single-center study. A third limitation of this study is that it was an observational study, thereby, precluding our ability to control the type of antimicrobial used prior to TG administration or the duration of TG treatment. However, our data have important clinical implications because of the limited number of therapeutic options for MDRAB isolates at present and the preliminary nature of evidence for the clinical use of these regimens [18, 33, 47, 49]. Although the overall clinical response rates in these previous reports appear favorable, the results are not conclusive because of the small sample sizes [13, 18, 19, 39, 47, 49]. Additionally, in vitro susceptibility to TG is often taken as in vivo efficacy in patients with MDRAB infections where TG is used off-label [18].
Treatment for MDRAB remains controversial. In spite of challenges with colistin, such as pharmacokinetics, renal toxicity, emergence of drug resistance, and a low concentration in the lungs, in vitro susceptibility data suggest that the only two drugs which can be used for MDRAB treatment are colistin (polymyxin B) and TG (this study). Other than clinical studies of TG conducted before entering the market, we believe that, among all the post-marketing surveillance studies, this study is the only controlled study with a large cohort. Based on our data, clinicians may still choose to use TG off-label for the treatment of MDRAB in critically ill patients who are in the ICU.
In conclusion, our data expand our understanding of the role of TG therapy in HAI. Since the treatment for A. baumannii has not been optimized, the treatment of HAIs caused by MDRAB is determined by in vitro susceptibility testing and by the susceptibility patterns of the MDRAB strains present in a given region. However, there is an imperative need for future studies to focus on large, well-controlled clinical trials for MDRAB infections, development of new antimicrobials regimens, and prevention of healthcare-associated MDRAB infections. MDRAB strains remain generally susceptible to polymyxins (colistin and polymyxin B), and there has been a recent focus on combination therapy to treat MDRAB infections [50, 51]. It will be interesting to review our data in the context of other novel antimicrobials against A. baumannii that are in the pipeline or in the experimental phase [52].
References
Gignon M, Farcy S, Schmit JL, Ganry O (2012) Prevention of healthcare-associated infections in general practice: current practice and drivers for change in a French study. Indian J Med Microbiol 30:69–75
Lee NY, Lee HC, Ko NY, Chang CM, Shih HI, Wu CJ, Ko WC (2007) Clinical and economic impact of multidrug resistance in nosocomial Acinetobacter baumannii bacteremia. Infect Control Hosp Epidemiol 28:713–719
Salgado CD, O’Grady N, Farr BM (2005) Prevention and control of antimicrobial-resistant infections in intensive care patients. Crit Care Med 33:2373–2382
Brusselaers N, Vogelaers D, Blot S (2011) The rising problem of antimicrobial resistance in the intensive care unit. Ann Intensive Care 1:47
Fournier PE, Richet H (2006) The epidemiology and control of Acinetobacter baumannii in health care facilities. Clin Infect Dis 42:692–699
Gordon NC, Wareham DW (2009) A review of clinical and microbiological outcomes following treatment of infections involving multidrug-resistant Acinetobacter baumannii with tigecycline. J Antimicrob Chemother 63:775–780
Sunenshine RH, Wright MO, Maragakis LL, Harris AD, Song X, Hebden J, Cosgrove SE, Anderson A, Carnell J, Jernigan DB, Kleinbaum DG, Perl TM, Standiford HC, Srinivasan A (2007) Multidrug-resistant Acinetobacter infection mortality rate and length of hospitalization. Emerg Infect Dis 13:97–103
Maragakis LL, Perl TM (2008) Acinetobacter baumannii: epidemiology, antimicrobial resistance, and treatment options. Clin Infect Dis 46:1254–1263
Chopra I, Roberts M (2001) Tetracycline antibiotics: mode of action, applications, molecular biology, and epidemiology of bacterial resistance. Microbiol Mol Biol Rev 65:232–260, second page, table of contents
Ellis-Grosse EJ, Babinchak T, Dartois N, Rose G, Loh E; Tigecycline 300 cSSSI Study Group; Tigecycline 305 cSSSI Study Group (2005) The efficacy and safety of tigecycline in the treatment of skin and skin-structure infections: results of 2 double-blind phase 3 comparison studies with vancomycin–aztreonam. Clin Infect Dis 41:S341–S353
Oliva ME, Rekha A, Yellin A, Pasternak J, Campos M, Rose GM, Babinchak T, Ellis-Grosse EJ, Loh E; 301 Study Group (2005) A multicenter trial of the efficacy and safety of tigecycline versus imipenem/cilastatin in patients with complicated intra-abdominal infections [Study ID Numbers: 3074A1-301-WW; ClinicalTrials.gov Identifier: NCT00081744]. BMC Infect Dis 5:88
Bouchillon SK, Hoban DJ, Johnson BM, Johnson JL, Hsiung A, Dowzicky MJ; Tigecycline Evaluation and Surveillance Trial (TEST) Group (2005) In vitro activity of tigecycline against 3989 Gram-negative and Gram-positive clinical isolates from the United States Tigecycline Evaluation and Surveillance Trial (TEST Program; 2004). Diagn Microbiol Infect Dis 52:173–179
Peleg AY, Potoski BA, Rea R, Adams J, Sethi J, Capitano B, Husain S, Kwak EJ, Bhat SV, Paterson DL (2007) Acinetobacter baumannii bloodstream infection while receiving tigecycline: a cautionary report. J Antimicrob Chemother 59(1):128–131
Peleg AY, Hooper DC (2010) Hospital-acquired infections due to gram-negative bacteria. N Engl J Med 362:1804–1813
Vasilev K, Reshedko G, Orasan R, Sanchez M, Teras J, Babinchak T, Dukart G, Cooper A, Dartois N, Gandjini H, Orrico R, Ellis-Grosse E; 309 Study Group (2008) A Phase 3, open-label, non-comparative study of tigecycline in the treatment of patients with selected serious infections due to resistant Gram-negative organisms including Enterobacter species, Acinetobacter baumannii and Klebsiella pneumoniae. J Antimicrob Chemother 62:i29–i40
Kelesidis T, Karageorgopoulos DE, Kelesidis I, Falagas ME (2008) Tigecycline for the treatment of multidrug-resistant Enterobacteriaceae: a systematic review of the evidence from microbiological and clinical studies. J Antimicrob Chemother 62:895–904
Garnacho-Montero J, Sa-Borges M, Sole-Violan J, Barcenilla F, Escoresca-Ortega A, Ochoa M, Cayuela A, Rello J (2007) Optimal management therapy for Pseudomonas aeruginosa ventilator-associated pneumonia: an observational, multicenter study comparing monotherapy with combination antibiotic therapy. Crit Care Med 35:1888–1895
Karageorgopoulos DE, Kelesidis T, Kelesidis I, Falagas ME (2008) Tigecycline for the treatment of multidrug-resistant (including carbapenem-resistant) Acinetobacter infections: a review of the scientific evidence. J Antimicrob Chemother 62:45–55
Fishbain J, Peleg AY (2010) Treatment of Acinetobacter infections. Clin Infect Dis 51:79–84
Garner JS, Jarvis WR, Emori TG, Horan TC, Hughes JM (1988) CDC definitions for nosocomial infections, 1988. Am J Infect Control 16:128–140
Horan TC, Andrus M, Dudeck MA (2008) CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control 36:309–332
Teasdale G, Jennett B (1974) Assessment of coma and impaired consciousness. A practical scale. Lancet 2(7872):81–84
Knaus WA, Zimmerman JE, Wagner DP, Draper EA, Lawrence DE (1981) APACHE—acute physiology and chronic health evaluation: a physiologically based classification system. Crit Care Med 9:591–597
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, Reinhart CK, Suter PM, Thijs LG (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med 22:707–710
[No authors listed] (1992) American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Peleg AY, Seifert H, Paterson DL (2008) Acinetobacter baumannii: emergence of a successful pathogen. Clin Microbiol Rev 21:538–582
Clinical and Laboratory Standards Institute (CLSI) (2006) Performance standards for antimicrobial disk susceptibility tests; Approved standard—9th edition. CLSI document M2-A9, . CLSI, Wayne, PA
Clinical and Laboratory Standards Institute (CLSI) (2011) Performance standards for antimicrobial susceptibility testing; Twenty-first informational supplement. CLSI document M100-S21. CLSI, Wayne, PA
Chen YH, Lu PL, Huang CH, Liao CH, Lu CT, Chuang YC, Tsao SM, Chen YS, Liu YC, Chen WY, Jang TN, Lin HC, Chen CM, Shi ZY, Pan SC, Yang JL, Kung HC, Liu CE, Cheng YJ, Liu JW, Sun W, Wang LS, Ko WC, Yu KW, Chiang PC, Lee MH, Lee CM, Hsu GJ, Hsueh PR (2012) Trends in the susceptibility of clinically important resistant bacteria to tigecycline: results from the Tigecycline In Vitro Surveillance in Taiwan study, 2006–2010. Antimicrob Agents Chemother 56:1452–1457
Dryden MS (2010) Complicated skin and soft tissue infection. J Antimicrob Chemother 65:iii35–iii44
Manchanda V, Sanchaita S, Singh N (2010) Multidrug resistant Acinetobacter. J Glob Infect Dis 2:291–304
Yahav D, Lador A, Paul M, Leibovici L (2011) Efficacy and safety of tigecycline: a systematic review and meta-analysis. J Antimicrob Chemother 66:1963–1971
Bassetti M, Nicolini L, Repetto E, Righi E, Del Bono V, Viscoli C (2010) Tigecycline use in serious nosocomial infections: a drug use evaluation. BMC Infect Dis 10:287
Napolitano LM (2008) Early appropriate parenteral antimicrobial treatment of complicated skin and soft tissue infections caused by methicillin-resistant Staphylococcus aureus. Surg Infect (Larchmt) 9:s17–s27
Bhattacharya M, Parakh A, Narang M (2009) Tigecycline. J Postgrad Med 55:65–68
Guner R, Hasanoglu I, Keske S, Kalem AK, Tasyaran MA (2011) Outcomes in patients infected with carbapenem-resistant Acinetobacter baumannii and treated with tigecycline alone or in combination therapy. Infection 39(6):515–518
Kuti JL, Dowzicky M, Nicolau DP (2008) A pharmacodynamic simulation to assess tigecycline efficacy for hospital-acquired pneumonia compared with other common intravenous antibiotics. J Chemother 20:69–76
Freire AT, Melnyk V, Kim MJ, Datsenko O, Dzyublik O, Glumcher F, Chuang YC, Maroko RT, Dukart G, Cooper CA, Korth-Bradley JM, Dartois N, Gandjini H; 311 Study Group (2010) Comparison of tigecycline with imipenem/cilastatin for the treatment of hospital-acquired pneumonia. Diagn Microbiol Infect Dis 68:140–151
Shin JA, Chang YS, Kim HJ, Kim SK, Chang J, Ahn CM, Byun MK (2012) Clinical outcomes of tigecycline in the treatment of multidrug-resistant Acinetobacter baumannii infection. Yonsei Med J 53:974–984
Prasad P, Sun J, Danner RL, Natanson C (2012) Excess deaths associated with tigecycline after approval based on noninferiority trials. Clin Infect Dis 54:1699–1709
Powers JH (2012) Editorial commentary: asking the right questions: morbidity, mortality, and measuring what’s important in unbiased evaluations of antimicrobials. Clin Infect Dis 54:1710–1713
Roberts JA, Lipman J (2009) Pharmacokinetic issues for antibiotics in the critically ill patient. Crit Care Med 37:840–851
Marchaim D, Navon-Venezia S, Schwartz D, Tarabeia J, Fefer I, Schwaber MJ, Carmeli Y (2007) Surveillance cultures and duration of carriage of multidrug-resistant Acinetobacter baumannii. J Clin Microbiol 45:1551–1555
Pachón-Ibáñez ME, Jiménez-Mejías ME, Pichardo C, Llanos AC, Pachón J (2004) Activity of tigecycline (GAR-936) against Acinetobacter baumannii strains, including those resistant to imipenem. Antimicrob Agents Chemother 48:4479–4481
Rodríguez-Hernández M-J, Cuberos L, Pichardo C, Caballero FJ, Moreno I, Jiménez-Mejías ME, García-Curiel A, Pachón J (2001) Sulbactam efficacy in experimental models caused by susceptible and intermediate Acinetobacter baumannii strains. J Antimicrob Chemother 47:479–482
Ko WC, Lee HC, Chiang SR, Yan JJ, Wu JJ, Lu CL, Chuang YC (2004) In vitro and in vivo activity of meropenem and sulbactam against a multidrug-resistant Acinetobacter baumannii strain. J Antimicrob Chemother 53:393–395
Wood GC, Hanes SD, Croce MA, Fabian TC, Boucher BA (2002) Comparison of ampicillin–sulbactam and imipenem–cilastatin for the treatment of Acinetobacter ventilator-associated pneumonia. Clin Infect Dis 34:1425–1430
Goel N, Wattal C, Oberoi JK, Raveendran R, Datta S, Prasad KJ (2011) Trend analysis of antimicrobial consumption and development of resistance in non-fermenters in a tertiary care hospital in Delhi, India. J Antimicrob Chemother 66:1625–1630
Gallagher JC, Rouse HM (2008) Tigecycline for the treatment of Acinetobacter infections: a case series. Ann Pharmacother 42:1188–1194
Lee CH, Tang YF, Su LH, Chien CC, Liu JW (2008) Antimicrobial effects of varied combinations of meropenem, sulbactam, and colistin on a multidrug-resistant Acinetobacter baumannii isolate that caused meningitis and bacteremia. Microb Drug Resist 14:233–237
Perez F, Hujer AM, Hujer KM, Decker BK, Rather PN, Bonomo RA (2007) Global challenge of multidrug-resistant Acinetobacter baumannii. Antimicrob Agents Chemother 51:3471–3484
Dijkshoorn L, Brouwer CP, Bogaards SJ, Nemec A, van den Broek PJ, Nibbering PH (2004) The synthetic N-terminal peptide of human lactoferrin, hLF(1-11), is highly effective against experimental infection caused by multidrug-resistant Acinetobacter baumannii. Antimicrob Agents Chemother 48:4919–4921
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, YT., Tsao, SM. & Hsueh, PR. Clinical outcomes of tigecycline alone or in combination with other antimicrobial agents for the treatment of patients with healthcare-associated multidrug-resistant Acinetobacter baumannii infections. Eur J Clin Microbiol Infect Dis 32, 1211–1220 (2013). https://doi.org/10.1007/s10096-013-1870-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-013-1870-4