Abstract
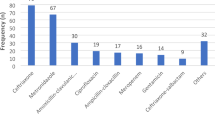
Extended and continuous infusions with beta-lactam antibiotics have been suggested as a means of pharmacokinetic and pharmacodynamic optimisation of antimicrobial therapy. Vancomycin is also frequently administered in continuous infusion, although more for practical reasons. A survey was undertaken to investigate the recommendations by the local antibiotic management teams (AMTs) in Belgian acute hospitals concerning the administration (intermittent, extended or continuous infusion) and therapeutic drug monitoring of four beta-lactam antibiotics (ceftazidime, cefepime, piperacillin–tazobactam, meropenem) and vancomycin for adult patients with a normal kidney function. A structured questionnaire survey comprising three domains was developed and approved by the members of the Belgian Antibiotic Policy Coordination Committee (BAPCOC). The questionnaire was sent by e-mail to the official AMT correspondents of 105 Belgian hospitals, followed by two reminders. The response rate was 32 %, with 94 %, 59 %, 100 %, 100 % and 100 % of the participating Belgian hospitals using ceftazidime, cefepime, piperacillin–tazobactam, meropenem and vancomycin, respectively. Comparing intensive care unit (ICU) with non-ICU wards showed a higher implementation of extended or continuous infusions for ceftazidime (81 % vs. 41 %), cefepime (35 % vs. 10 %), piperacillin–tazobactam (38 % vs. 12 %), meropenem (68 % vs. 35 %) and vancomycin (79 % vs. 44 %) on the ICU wards. A majority of the hospitals recommended a loading dose prior to the first dose. For vancomycin, the loading dose and the trough target concentration were too low based on the current literature. This survey shows that extended and continuous infusions with beta-lactams and vancomycin are widely implemented in Belgian hospitals.
Similar content being viewed by others
Notes
The Belgian law provides that an AMT must be operating in each Belgian hospital where infectious diseases treatments are undertaken. AMTs have a mandatory role in the setting of hospital formularia and must intervene in the setting of local guidelines and analysis of local epidemiology.
References
Craig WA (2003) Basic pharmacodynamics of antibacterials with clinical applications to the use of beta-lactams, glycopeptides, and linezolid. Infect Dis Clin North Am 17:479–501
Roberts JA, Webb S, Paterson D, Ho KM, Lipman J (2009) A systematic review on clinical benefits of continuous administration of beta-lactam antibiotics. Crit Care Med 37:2071–2078
Cataldo MA, Tacconelli E, Grilli E, Pea F, Petrosillo N (2012) Continuous versus intermittent infusion of vancomycin for the treatment of Gram-positive infections: systematic review and meta-analysis. J Antimicrob Chemother 67:17–24
Wysocki M, Delatour F, Faurisson F, Rauss A, Pean Y, Misset B, Thomas F, Timsit JF, Similowski T, Mentec H, Mier L, Dreyfuss D (2001) Continuous versus intermittent infusion of vancomycin in severe staphylococcal infections: prospective multicenter randomized study. Antimicrob Agents Chemother 45:2460–2467
Van Gastel E, Costers M, Peetermans WE, Struelens MJ; Hospital Medicine Working Group of the Belgian Antibiotic Policy Coordination Committee (2010) Nationwide implementation of antibiotic management teams in Belgian hospitals: a self-reporting survey. J Antimicrob Chemother 65:576–580
Claus B, Buyle F, Robays H, Vogelaers D (2010) Importance of infusion volume and pump characteristics in extended administration of β-lactam antibiotics. Antimicrob Agents Chemother 54:4950
Geggie D, Moore D (2007) Peripheral line dead space: an unrecognised phenomenon? Emerg Med J 24:558–559
Sanford JP, Gilbert D, Chambers H, Eliopoulos GM, Moellering R, Saag M (2010) The Sanford guide to antimicrobial therapy, 2010–2011, 22nd edn. Belgian/Luxembourg version. Belgian/Luxembourg Working Party on Antimicrobial Therapy. ISBN 978-1-930808-63-3
Federal Agency for Medicines and Health Products (FAMHP) Summary of product characteristics (SPC) for vancocin. Available online at: http://bijsluiters.fagg-afmps.be/. Accessed 1 Oct 2012
Federal Agency for Medicines and Health Products (FAMHP) Summary of product characteristics (SPC) for glazidim. Available online at: http://bijsluiters.fagg-afmps.be/. Accessed 1 Oct 2012
Van Herendael B, Jeurissen A, Tulkens PM, Vlieghe E, Verbrugghe W, Jorens PG, Ieven M (2012) Continuous infusion of antibiotics in the critically ill: the new holy grail for beta-lactams and vancomycin? Ann Intensive Care 2:22
Mouton JW, Vinks AA (2007) Continuous infusion of beta-lactams. Curr Opin Crit Care 13:598–606
Roberts JA, Kirkpatrick CM, Roberts MS, Dalley AJ, Lipman J (2010) First-dose and steady-state population pharmacokinetics and pharmacodynamics of piperacillin by continuous or intermittent dosing in critically ill patients with sepsis. Int J Antimicrob Agents 35:156–163
Ocampos-Martinez E, Penaccini L, Scolletta S, Abdelhadii A, Devigili A, Cianferoni S, de Backer D, Jacobs F, Cotton F, Vincent JL, Taccone FS (2012) Determinants of early inadequate vancomycin concentrations during continuous infusion in septic patients. Int J Antimicrob Agents 39:332–337
Truong J, Levkovich BJ, Padiglione AA (2012) Simple approach to improving vancomycin dosing in intensive care: a standardised loading dose results in earlier therapeutic levels. Intern Med J 42:23–29
Li J, Udy AA, Kirkpatrick CM, Lipman J, Roberts JA (2012) Improving vancomycin prescription in critical illness through a drug use evaluation process: a weight-based dosing intervention study. Int J Antimicrob Agents 39:69–72
Rybak M, Lomaestro B, Rotschafer JC, Moellering R Jr, Craig W, Billeter M, Dalovisio JR, Levine DP (2009) Therapeutic monitoring of vancomycin in adult patients: a consensus review of the American Society of Health-System Pharmacists, the Infectious Diseases Society of America, and the Society of Infectious Diseases Pharmacists. Am J Health Syst Pharm 66:82–98
Taccone FS, Laterre PF, Dugernier T, Spapen H, Delattre I, Wittebole X, De Backer D, Layeux B, Wallemacq P, Vincent JL, Jacobs F (2010) Insufficient β-lactam concentrations in the early phase of severe sepsis and septic shock. Crit Care 14:R126
Roberts JA, Ulldemolins M, Roberts MS, McWhinney B, Ungerer J, Paterson DL, Lipman J (2010) Therapeutic drug monitoring of beta-lactams in critically ill patients: proof of concept. Int J Antimicrob Agents 36:332–339
Udy AA, Varghese JM, Altukroni M, Briscoe S, McWhinney BC, Ungerer JP, Lipman J, Roberts JA (2012) Subtherapeutic initial beta-lactam concentrations in select critically ill patients: association between augmented renal clearance and low trough drug concentrations. Chest 142:30–39
Pea F, Furlanut M, Negri C, Pavan F, Crapis M, Cristini F, Viale P (2009) Prospectively validated dosing nomograms for maximizing the pharmacodynamics of vancomycin administered by continuous infusion in critically ill patients. Antimicrob Agents Chemother 53:1863–1867
Carricajo A, Forgeot A, Morel J, Auboyer C, Zeni F, Aubert G (2010) Dosage adjustment of vancomycin in continuous infusion in critically-ill patients. Ann Fr Anesth Reanim 29:55–57
Spapen HD, Janssen van Doorn K, Diltoer M, Verbrugghe W, Jacobs R, Dobbeleir N, Honoré PM, Jorens PG (2011) Retrospective evaluation of possible renal toxicity associated with continuous infusion of vancomycin in critically ill patients. Ann Intensive Care 19:26
Ingram PR, Lye DC, Tambyah PA, Goh WP, Tam VH, Fisher DA (2008) Risk factors for nephrotoxicity associated with continuous vancomycin infusion in outpatient parenteral antibiotic therapy. J Antimicrob Chemother 62:168–171
Gupta A, Biyani M, Khaira A (2011) Vancomycin nephrotoxicity: myths and facts. Neth J Med 69:379–383
Baririan N, Chanteux H, Viaene E, Servais H, Tulkens PM (2003) Stability and compatibility study of cefepime in comparison with ceftazidime for potential administration by continuous infusion under conditions pertinent to ambulatory treatment of cystic fibrosis patients and to administration in intensive care units. J Antimicrob Chemother 51:651–658
Kuti JL, Nightingale CH, Knauft RF, Nicolau DP (2004) Pharmacokinetic properties and stability of continuous-infusion meropenem in adults with cystic fibrosis. Clin Ther 26:493–501
Berthoin K, Le Duff CS, Marchand-Brynaert J, Carryn S, Tulkens PM (2010) Stability of meropenem and doripenem solutions for administration by continuous infusion. J Antimicrob Chemother 65:1073–1075
Acknowledgements
We thank the members of the Hospital Medicine Working Group of the Belgian Antibiotic Policy Coordination Committee (BAPCOC) for revising the content of the questionnaire and for providing the e-mail addresses of the official contact persons of the antibiotic management teams (AMTs) in Belgian hospitals.
We thank our colleagues from the AMTs in the participating hospitals for completing the questionnaire.
Funding
None.
Conflict of interest
The authors declare that they have no conflict of interest.
Transparency declarations
None to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Buyle, F.M., Decruyenaere, J., De Waele, J. et al. A survey of beta-lactam antibiotics and vancomycin dosing strategies in intensive care units and general wards in Belgian hospitals. Eur J Clin Microbiol Infect Dis 32, 763–768 (2013). https://doi.org/10.1007/s10096-012-1803-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-012-1803-7