Abstract
Q fever is a worldwide zoonosis caused by Coxiella burnetii bacterium. Two clinical forms are present: acute Q fever and chronic disease, including endocarditis. Currently, the diagnosis of Q fever endocarditis is based on the detection of anti-phase I antibodies. The objective of the study was to identify candidate proteins for the serological diagnosis of endocarditis due to C. burnetii. The immunoreactivities of sera from 12 patients with C. burnetii infections, including the sera from patients with endocarditis and with the acute clinical form of Q fever, were compared with those of three control subjects who did not have Q fever. We identified 29 candidate antigenic proteins by mass spectrometry. Two proteins, arginine repressor and OmpH, were recognised exclusively by the sera of patients with Q fever endocarditis. These proteins are promising candidates for the development of serodiagnostic assays for Q fever endocarditis.
Similar content being viewed by others
Introduction
Coxiella burnetii is a strict intracellular bacterium responsible for Q fever in humans, livestock and other vertebrates. Reservoirs of infection include both wild and domestic mammals, birds and arthropods [1]. Cattle, goats and sheep are considered to be the primary reservoirs from which human infections originate [2]. In humans, the disease is generally acquired via the respiratory route by the inhalation of infectious aerosols and may be present in two forms: acute and chronic [1].
The most common acute form of Q fever is manifested in humans as atypical pneumoniae, self-limited febrile illnesses or granulomatous hepatitides. Infection can also be asymptomatic. The clinical expression of acute Q fever has already been described [3].
Persistent C. burnetii infection may lead to a chronic form of the disease with endocarditis, osteomyelitis or infected aortic aneurysms [4, 5]. Q fever endocarditis is often a severe disease associated with a long diagnostic delay. The positive blood culture is a gold standard for Q fever endocarditis diagnosis. However, sterile blood cultures are noted in one third of patients with infectious endocarditis [6]. Most often, the antibiotics treatment precedes blood culture; this holds true in 45–60% of cases of culture-negative endocarditis (CNE) [7]. The diagnosis is most often based upon the detection of vegetation on the cardiac valves using echography [8]. It has been shown that the sensitivity of C. burnetii endocarditis detection is possible in only 13% of Q fever cases [6, 9]. The lack of systematic serological testing for C. burnetii in CNE is the important limiting factor in the aetiological diagnosis of CNE in patients with infectious endocarditis reported in the literature [9, 10]. Many serological methods have been used to rapidly diagnose infection with C. burnetii; however, ambiguous results are frequently obtained [6, 8]. The diagnosis based on serum antibody response to C. burnetii phase I and II is carried out only by specialised laboratories. In such situations, the diagnosis of Q fever endocarditis remains a diagnostic challenge.
The most reliable and commonly used methods are indirect immunofluorescence [11] and complement fixation [12]. Both C. burnetii Nine-Mile strain phase I and phase II are used as antigens. Antibodies to phase I and phase II have been detected in the IgG, IgM and IgA classes. Q fever endocarditis has been associated with very high titres of anti-phase I IgG antibodies. Cross-reactions however, may be a source of confusion when interpreting serological results [13]. The molecular detection of C. burnetii in blood and sera during illness is also performed [14].
The development of useful recombinant antigens could prove to be a step towards the development of novel approaches for detecting C. burnetii in clinical samples, and also for detecting new targets for serodiagnostics and vaccine development. Immunoproteomics is one method to identify such candidate proteins. Several proteomic studies have been reported recently, but none clearly addresses proteins for the diagnosis of Q fever endocarditis [15, 16]. A recent study reported efforts to identify specific protein markers for three clinical isolates of C. burnetii using a matrix-assisted laser desorption/ionisation time-of-flight (MALDI-TOF) mass spectrometry [17]. Furthermore, an immunoproteomic approach [15] has been undertaken to characterise specific proteins from the developmental forms of small-cell variants/large-cell variants (SCV/LCV) of C. burnetii involved in protective immunity. A biphasic developmental cycle whereby highly resistant SCVs are generated from LCVs is considered to be fundamental to the virulence of C. burnetii. The identification of cell-form specific and common antigens provided new information for the development of subunit vaccines and new diagnostic tests.
In the present study, we focussed on the identification of serological markers for diagnosing Q fever endocarditis using an immunoproteomic approach combined with mass spectrometry.
Methods
Sera
Diagnosis of Q fever-positive patients and the selection of human sera
The diagnosis of patients with Q fever was achieved by serology [11]. The diagnosis of infective endocarditis (IE) was performed using modified Duke’s criteria [18]. The sera from five patients suffering from acute Q fever, seven patients suffering from Q fever endocarditis and three healthy blood donors were selected for subsequent studies. They are all listed in Table 1 and the profiles of antibody response (IgG, IgM, IgA, phase I and phase II) for each patient is shown in Fig. 1.
Bacterial culture and purification
Strain Nine Mile RSA 493 (C. burnetii, COXBU, 227377, genus Coxiella) from the American Type Culture Collection (ATCC, USA) was propagated on Vero cell monolayers (ATCC CRL 1587). Minimal essential medium (MEM) (Invitrogen, Cergy-Pontoise, France) supplemented with 4% foetal bovine serum (Invitrogen, Cergy-Pontoise, France) and 1% L-glutamine (Invitrogen, Cergy-Pontoise, France) was used for cultivation. Infected cells were maintained in a 5% CO2 atmosphere at 35°C. C. burnetii cells were harvested, pelletted, resuspended in MEM and purified on a discontinuous renographin gradient as described previously [19]. Purified bacteria were washed in PBS (at 10,000g, 10 min) and stored at –80°C until use. All purification steps were monitored by Gimenez staining [20].
Preparation of crude extracts for 2-D gel electrophoresis
We applied the methods earlier described by Renesto et al. [21], with some modifications. The C. burnetii pellet was resuspended in 5 ml of 5 mM Tris-HCl buffer (pH 7.6) and lysed by two passages through a Constant Cell Disruption System (2 kBar). Cell debris and unbroken cells were discarded following a centrifugation cycle at 5,600g for 20 min at 4°C. The supernatant was transferred into a new tube and ultracentrifuged (100,000g for 2 h at 4°C in a Beckman MLS-50 rotor). After washing in 5 mM Tris-HCl, pH 7.6, the membrane-enriched pellet was resuspended in rehydration solution (7 M urea, 2 M thiourea, 4% (w/v) CHAPS) and stored at –80°C. Proteins were precipitated using the PlusOne 2-D Clean-Up Kit (GE Healthcare, Chalfont St. Giles, UK) and suspended again in rehydration solution. To conserve the restricted amounts of proteins, we used Immobiline™ DryStrips, pH 3–10 (GE Healthcare, Chalfont St. Giles, UK) of two different lengths, 7 or 18 cm, depending on the subsequent application. Immunoblotting was performed on 7-cm strips, while spots on 18-cm strips were identified by mass spectrometry. Strips were rehydrated overnight with the 20 µg/7-cm strip and the 150 ug/18-cm strip of proteins in rehydration solution supplemented with 0.5% (v/v) IPG buffer (pH 4–7) (GE Healthcare, Chalfont St. Giles, UK). The isoelectric focussing (IEF) was carried out according to the manufacturer’s instructions (Ettan IPGphor II, GE Healthcare, Chalfont St. Giles, UK). Prior to gel electrophoresis in the second dimension, the strips were equilibrated as previously described [21]. The strips were then embedded in 0.5% agarose and the proteins were resolved by electrophoresis through a 10% acrylamide gel (Ettan™ DALT, GE Healthcare, Chalfont St. Giles, UK) for the 18-cm strips and an 11.25% acrylamide gel for the 7-cm strips (Bio-Rad Protean Mini xi chamber), as described by the manufacturer. Electrophoresis was performed until the bromophenol blue dye front reached the bottom of the gel. For protein identification following electrophoresis, the gels were silver-stained [22] and digitised by transmission scanning (ImageScanner, GE Healthcare, Chalfont St. Giles, UK).
Immunoblot assay
For Western blotting, the polyacrylamide 2-D gels were transferred onto a nitrocellulose membrane in a transblot cell (Bio-Rad) at 100 V for 1 h 30 min in an ice bath. Membranes were then blocked in TBST (Tris-HCl 50 mM (Invitrogen Cergy-Pontoise, France), NaCl 250 mM supplemented with 0.5% Triton X-100) and 5% non-fat dried milk overnight. Then, they were incubated with the human sera as described in Table 1 in solution TBST and 5% non-fat dried milk (dilution of 1:500). Following 1 h incubation, the membranes were washed three times in TBST, incubated with peroxidase-conjugated immunoglobulin (goat anti-human Ig (H + L) 1:1000 (Southern Biotechnology, Birmingham, Alabama, USA). Each membrane was treated with the secondary antibody and washed three times, as previously described. Detection was carried out using a commercially available chemiluminescence kit (ECL™ Western Blotting Analysis System, GE Healthcare). The membranes were exposed to Hyperfilm™ ECL (GE Healthcare, Chalfont St. Giles, UK) and subsequently developed using an automated film processor (Hyperprocessor™, GE Healthcare, Chalfont St. Giles, UK).
Standard software was used for the analyses of the stained 2-D gels and blot images (ImageMaster™ 2D Platinum version 6.0, GE Healthcare, Chalfont St. Giles, UK). For 2-D gels, these analyses included spot detection, matching and the estimation of isoelectric point (pI) and molecular weight (Mr). For each individual, immunoblots were performed at least twice. Immune profiles of the spots were analysed when two independent assays had produced identical patterns. We superimposed the immunoblot images over those on gels using the subset of spots (CBU_0937), which were recognised by the majority of the subjects and, consequently, was used for internal calibration. Thus, this approach permits the direct determination of the position for prominent spots on the 2D silver-stained gel and manually excised for consequent MALDI-TOF mass spectrometry analysis.
Digestion of proteins and MALDI-TOF mass spectrometry analysis
Protein spots excised from silver-stained gels were destained and subjected to in-gel digestion with trypsin (sequencing-grade modified porcine trypsin, Promega, Madison, WI, USA) [23]. Tryptic peptides were then extracted from the gel by successive treatment with 80% acetonitrile in 0.2% trifluoroacetic acid (TFA). Extracts were dried at ambient room temperature. Peptides were co-crystallised onto the MALDI target with a matrix solution of α-cyano-4-hydroxycinnamic acid in water/acetonitrile (1:1) with 0.5% TFA deposed two times with a volume of 0.5 µl. Mass analyses were performed with a MALDI-TOF/TOF Bruker Ultraflex II spectrometer (Bruker Daltonics, Wissembourg, France). The mass spectra were internally calibrated using autolytic peptides from trypsin.
To identify the proteins, the peptide mass lists were matched against databases proposed by the search engine Mascot (Matrix Science Ltd., London, UK), which is available at http://www.matrixscience.com/. In general, proteins with the highest sequence coverage and Mascot score were selected as candidate antigens [24].
Bioinformatics
We used HMMTOP 2.0, which is freely available at http://www.enzim.hu/hmmtop, to predict both the localisation of helical transmembrane segments and the topology of the identified proteins [25]. We classified the identified proteins into clusters of orthologous groups (COGs) functional categories according to the public database (http://www.ncbi.nlm.nih.gov/COG/). These are shown in Table 2.
Results
Western blot
The purification procedure for C. burnetii allowed the resolution of 250 proteins as determined by the software (ImageMaster™ 2D Platinium version 6.0, GE Healthcare, Chalfont St. Giles, UK). Spots of varying intensities with molecular masses ranging from 10 to 100 kDa were visualised on 7- and/or 18-cm gels, within a pH range from 3 to 10 (Fig. 2), respectively. Most of the proteins clustered within an acidic pH range of 4–7.
Two-dimensional reference map of the whole-cell extract from C. burnetii. The proteins of C. burnetii (strain Nine Mile) were resolved by isoelectric focussing (IEF) and separated across the pH range 3–10 (18 cm), 10% acrylamide. The protein spots were visualised with silver nitrate staining. The numbered arrows indicate “discriminate antigens” of C. burnetii. The protein spots identified by matrix-assisted laser desorption/ionisation time-of-flight (MALDI-TOF) are annotated (e.g. Cb1) and listed in Table 2. The magnified region on the right side of the gel shows the most discriminate spots for Q fever endocarditis patients, i.e. Cb10 identified as arginine repressor and Cb 31 identified as OmpH. The molecular weight marker is indicated on the left side of the gel
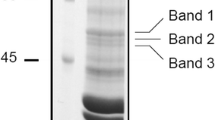
As illustrated in the shown examples of immunoblot of 2-D gel-separated antigens with human sera (Fig. 3), the antigenic recognition profiles obtained with the serum of patients with acute Q fever (A, B, C) differed from those with endocarditis (E, F, G). The main distinction observed was the recognition of a significant antigenic protein spot in a low molecular weight range (17-, 18-kDa and pI about 10) that was not detected by the reaction with the sera of patients with the acute form of Q fever. The antigenic proteins were identified from the corresponding silver-stained gel. All reactive spots were identified (Table 2).
Example of 2-D immunoblots profile obtained with the sera from C. burnetii-infected patients and healthy blood donors. The 2-D immunoblots probed with: (A, B, C) sera from the patients with acute Q fever; (E, F, G) sera from the patients with Q fever endocarditis; (D, H) sera from healthy blood donors. The human sera were diluted 1:500. All spots were subjected to MALDI-TOF identification. The arrows indicate the corresponding antigenic spots identified by MALDI-TOF: CBU_0937 used for internal calibration, and spots of interest: CBU_0480, CBU_0612 recognised by sera with Q fever endocarditis, CBU_0910 recognised by both sera with acute and chronic Q fever
The immunoblots obtained with the sera of healthy blood donors (D, H), included in this study as a control group, have shown no cross-reactivity to C. burnetii proteins.
Identification of antigenic C. burnetii proteins
The most intense antigenic protein spots detected after silver staining were excised from seven different gels (five pH 3–10, 7-cm gels, and two pH 3–10, 18-cm gels), and were subject to analysis by MALDI-TOF mass spectrometry (Fig. 2). Twenty-nine proteins were successfully identified. Eight of them are potential transmembrane proteins. All proteins labelled in the gel (Fig. 2) and listed in Table 2 were repeatedly identified based on eight independent sets of data mapping to the same ORF. Two protein spots, nos. 14 and 26, were only identified in one gel, and, therefore, have been excluded from the table. The two spots that made a visible difference between the two major clinical manifestations of Q fever (Fig. 2, magnified square) were identified as an outer membrane protein, OmpH, and arginine repressor (Table 2). Several spots resulted in the same protein being identified, suggesting the presence of numerous isoforms: e.g. chaperonin, 60 kDa, CBU_1718; conserved hypothetical protein, CBU_0937; translation elongation factor Tu, CBU_0223.
The other identified proteins belonged to various COG categories (Table 2).
Discussion
The aim of this study was to find antigenic candidates for the development of serodiagnostic tests for Q fever endocarditis. We have successfully identified two protein candidates, namely, arginine repressor and OmpH. They were found to be exclusively antigenic with the sera obtained from patients suffering from chronic Q fever endocarditis.
These data have raised an interesting possibility of using these antigens to develop a serological test for the diagnosis of Q fever endocarditis. Most of the 27 remaining proteins identified in this study were antigenic with both sets of sera, acute and chronic. However, they might enable the serodiagnosis of both acute and chronic Q fever.
We are aware of several technical limitations in this study. The first involves matching protein spots with immunoblots following 2-D electrophoresis. Slight gel-to-gel variations were sometimes observed, but rigorous spot selection was applied and several gels were used for identification by MS. The second is related to the superior detection provided by the ECL reaction compared with silver staining. As a result of this, certain spots appeared as clustered on Western blots compared with silver-stained gels (Figs. 2 and 3). The last limitation results from the small cohort of patients included in this study.
The role of arginine repressor in transcriptional regulation in C. burnetii has yet to be completely elucidated. It a major component of biosynthetic pathways [26, 27] that regulates the initiation of transcription [28].
The genetic control of arginine-metabolising enzymes in many bacteria is achieved through the arginine repressor (ArgR) [29–33], which responds to intracellular levels of L-arginine. A content of arginine is influenced by arginine repressor. Bioinformatics analysis has revealed putative homologues of ArgR in many species [34–36]. Existence of the two types of argR alleles in natural population and the selective advantage of each type under different conditions was described and provided evidence for the evolutionary history of argR regulation by Escherichia coli [37]. The strategy of regulation may depend on the nature of the environment. However, the role of argR in the pathogenesis of endocarditis is not known.
OmpH, a cell wall/membrane/envelope biogenesis-associated protein, is an outer membrane protein widely studied in other bacteria and is known to be an excellent target for human antibodies [38, 39]. It may be an important factor for adhesion to host cells, with chaperonin-like activity, a protein important for the biosynthesis of the outer membrane. Antibody specificity for the corresponding antigen was already found in a comparable study for Chlamydia pneumoniae [40]. OmpH has been suggested as a potential candidate for vaccine development [40].
Some of the proteins identified in this study belong to the same cluster of orthologous groups as the two main proteins of interest to us (Table 2, COG K and/or M). They have been found to be discriminative in other immunoproteomic studies [41, 42], such as N utilisation transmembrane substance protein A (NusA) (Cb 18, CBU_1433) and DNA-directed RNA polymerase alpha subunit (Cb 6, CBU_0263). Both are able to modulate transcription [43]. We have identified the protein 3-deoxy-D-manno-octulosonate cytidylyltransferase protein (CMP-KDO synthase) as being antigenic (Cb 29, CBU_0479). CMP/KDO synthase inhibitors were described as a crucial factor for reducing the virulence of Gram-negative bacteria. Attempts have been made to find a potent inhibitor of 3-deoxy-D-manno-octulosonate cytidylyltransferase (CMP-KDO synthase) capable of inhibiting the growth of Gram-negative bacteria by interfering with the biosynthesis of lipopolysaccharide (LPS) [44]. The interaction of the bacterial agent with dendritic cells (DC) is dependent on the length of the LPS; the virulent form of C. burnetii Nine Mile is associated with full-length LPS, whereas the truncated form is associated with the avirulent form [45]. This LPS length-dependence has been postulated as a critical component of both innate and adaptive immunity of this bacteria [46, 47].
We assigned the proteins identified using the data we obtained into several functional categories (Table 2). Many of the proteins identified are known to be involved in C. burnetii developmental processing. Some of the identified proteins have been detected in previous studies using proteomic approaches [17, 48, 49]. We found several protein candidates that match those from these previous studies (Table 2), such as N utilisation substance protein A (Cb 18), which is able to modulate transcription; ribosomal protein S1 (Cb 28), which belongs to the large order of ribosomal proteins and plays an important role in translation system; hypothetical protein (Cb 16); heat shock proteins HtpG (Cb 8) and GroEL (Cb 20) destined for translocation through biological membranes; or elongation factor-Tu (Cb 5), one of the major proteins of C. burnetii, an essential component of the translational machinery of the cell. Com1 outer membrane protein (Cb 24), which is known to be preferentially exposed on the surface of C. burnetii, and the gene encoding this protein, has been through trials as a genetic marker to distinguish among isolates [50]. These were all immunorecognised by the human sera in our study, except the hypothetical protein (Cb 16).
However, the objective of all of these proteomic studies was not exactly in line with the aim of our study. We were mostly interested in protein spots associated exclusively with chronic Q fever. We have successfully identified two targets which we believe to be the most suitable for developing Q fever endocarditis serodiagnostic assays, namely, arginine repressor (Cb 10, CBU_0480) and/or outer membrane protein OmpH (Cb 31, CBU_0612). Indeed, the development of endocarditis in patients with previous valvular lesions and suffering from Q fever is a major issue [51]. As a matter of fact, 30 to 50% of such patients will develop a chronic infection if untreated [52]. On the other hand, the duration of preventive treatment is long (one year), and may be hampered by adverse effects. Currently, repeating serology is the only possible strategy to detect an early valvular fixation [53]. Therefore, the raising of antibodies to these protein candidates may prove to be an efficient tool to detect an evolution towards chronic infection.
Conclusion
The combination of 2-D gel electrophoresis, immunoblotting and matrix-assisted laser desorption/ionisation time-of-flight (MALDI-TOF) mass spectrometry allowed us to identify 29 candidate proteins for Q fever serology development. Two of them, OmpH and arginine repressor, were specifically associated with Q fever endocarditis. The next step will be to express these proteins in order to design a test that may be useful for detecting the evolution of chronic infection due to Coxiella burnetii.
Abbreviations
- IEF:
-
Isoelectric focussing
- COG:
-
Cluster of orthologous groups
- IE:
-
Infective endocarditis
References
Maurin M, Raoult D (1999) Q fever. Clin Microbiol Rev 12:518–553
Kovácová E, Kazár J (2002) Q fever—still a query and underestimated infectious disease. Acta Virol 46:193–210
Raoult D, Tissot-Dupont H, Foucault C, Gouvernet J, Fournier PE, Bernit E, Stein A, Nesri M, Harle JR, Weiller PJ (2000) Q fever 1985–1998. Clinical and epidemiologic features of 1,383 infections. Medicine (Baltimore) 79:109–123
Karakousis PC, Trucksis M, Dumler JS (2006) Chronic Q fever in the United States. J Clin Microbiol 44:2283–2287
Botelho-Nevers E, Fournier PE, Richet H, Fenollar F, Lepidi H, Foucault C, Branchereau A, Piquet P, Maurin M, Raoult D (2007) Coxiella burnetii infection of aortic aneurysms or vascular grafts: report of 30 new cases and evaluation of outcome. Eur J Clin Microbiol Infect Dis 26:635–640
Brouqui P, Raoult D (2006) New insight into the diagnosis of fastidious bacterial endocarditis. FEMS Immunol Med Microbiol 47:1–13
Lamas CC, Eykyn SJ (1997) Suggested modifications to the Duke criteria for the clinical diagnosis of native valve and prosthetic valve endocarditis: analysis of 118 pathologically proven cases. Clin Infect Dis 25:713–719
Eykyn SJ (2001) Endocarditis: basics. Heart 86:476–480
Fenollar F, Thuny F, Xeridat B, Lepidi H, Raoult D (2006) Endocarditis after acute Q fever in patients with previously undiagnosed valvulopathies. Clin Infect Dis 42:818–821
Werner M, Fournier PE, Andersson R, Hogevik H, Raoult D (2003) Bartonella and Coxiella antibodies in 334 prospectively studied episodes of infective endocarditis in Sweden. Scand J Infect Dis 35:724–727
Peacock MG, Philip RN, Williams JC, Faulkner RS (1983) Serological evaluation of O fever in humans: enhanced phase I titers of immunoglobulins G and A are diagnostic for Q fever endocarditis. Infect Immun 41:1089–1098
Houpikian P, Raoult D (2003) Diagnostic methods. Current best practices and guidelines for identification of difficult-to-culture pathogens in infective endocarditis. Cardiol Clin 21:207–217
Dupont HT, Thirion X, Raoult D (1994) Q fever serology: cutoff determination for microimmunofluorescence. Clin Diagn Lab Immunol 1:189–196
Rolain JM, Raoult D (2005) Molecular detection of Coxiella burnetii in blood and sera during Q fever. QJM 98:615–617
Coleman SA, Fischer ER, Cockrell DC, Voth DE, Howe D, Mead DJ, Samuel JE, Heinzen RA (2007) Proteome and antigen profiling of Coxiella burnetii developmental forms. Infect Immun 75:290–298
Samoilis G, Psaroulaki A, Vougas K, Tselentis Y, Tsiotis G (2007) Analysis of whole cell lysate from the intercellular bacterium Coxiella burnetii using two gel-based protein separation techniques. J Proteome Res 6:3032–3041
Skultéty L, Hernychová L, Beregházyová E, Slabá K, Toman R (2007) Detection of specific spectral markers of Coxiella burnetii isolates by MALDI-TOF mass spectrometry. Acta Virol 51:55–58
Li JS, Sexton DJ, Mick N, Nettles R, Fowler VG Jr, Ryan T, Bashore T, Corey GR (2000) Proposed modifications to the Duke criteria for the diagnosis of infective endocarditis. Clin Infect Dis 30:633–638
Fournier PE, Marrie TJ, Raoult D (1998) Diagnosis of Q fever. J Clin Microbiol 36:1823–1834
Gimenez DF (1964) Staining rickettsiae in yolk-sac cultures. Stain Technol 39:135–140
Renesto P, Azza S, Dolla A, Fourquet P, Vestris G, Gorvel JP, Raoult D (2005) Proteome analysis of Rickettsia conorii by two-dimensional gel electrophoresis coupled with mass spectrometry. FEMS Microbiol Lett 245:231–238
Nesterenko MV, Tilley M, Upton SJ (1994) A simple modification of Blum’s silver stain method allows for 30 minute detection of proteins in polyacrylamide gels. J Biochem Biophys Methods 28:239–242
Shevchenko A, Wilm M, Vorm O, Mann M (1996) Mass spectrometric sequencing of proteins silver-stained polyacrylamide gels. Anal Chem 68:850–858
Perkins DN, Pappin DJ, Creasy DM, Cottrell JS (1999) Probability-based protein identification by searching sequence databases using mass spectrometry data. Electrophoresis 20:3551–3567
Tusnády GE, Simon I (2001) The HMMTOP transmembrane topology prediction server. Bioinformatics 17:849–850
Fujiwara K, Tsubouchi T, Kuzuyama T, Nishiyama M (2006) Involvement of the arginine repressor in lysine biosynthesis of Thermus thermophilus. Microbiology 152:3585–3594
Caldara M, Charlier D, Cunin R (2006) The arginine regulon of Escherichia coli: whole-system transcriptome analysis discovers new genes and provides an integrated view of arginine regulation. Microbiology 152:3343–3354
Maas WK (1994) The arginine repressor of Escherichia coli. Microbiol Rev 58:631–640
Mountain A, Baumberg S (1980) Map locations of some mutations conferring resistance to arginine hydroxamate in Bacillus subtilis 168. Mol Gen Genet 178:691–701
Mountain A, Mann NH, Munton RN, Baumberg S (1984) Cloning of a Bacillus subtilis restriction fragment complementing auxotrophic mutants of eight Escherichia coli genes of arginine biosynthesis. Mol Gen Genet 197:82–89
Lim DB, Oppenheim JD, Eckhardt T, Maas WK (1987) Nucleotide sequence of the argR gene of Escherichia coli K-12 and isolation of its product, the arginine repressor. Proc Natl Acad Sci USA 84:6697–6701
North AK, Smith MC, Baumberg S (1989) Nucleotide sequence of a Bacillus subtilis arginine regulatory gene and homology of its product to the Escherichia coli arginine repressor. Gene 80:29–38
Garnett JA, Marincs F, Baumberg S, Stockley PG, Phillips SE (2008) Structure and function of the arginine repressor-operator complex from Bacillus subtilis. J Mol Biol 379:284–298
Fleischmann RD, Adams MD, White O, Clayton RA, Kirkness EF, Kerlavage AR, Bult CJ, Tomb JF, Dougherty BA, Merrick JM (1995) Whole-genome random sequencing and assembly of Haemophilus influenzae Rd. Science 269:496–512
Rodríguez-García A, Ludovice M, Martín JF, Liras P (1997) Arginine boxes and the argR gene in Streptomyces clavuligerus: evidence for a clear regulation of the arginine pathway. Mol Microbiol 25:219–228
Cole ST, Brosch R, Parkhill J, Garnier T, Churcher C, Harris D, Gordon SV, Eiglmeier K, Gas S, Barry CE 3rd, Tekaia F, Badcock K, Basham D, Brown D, Chillingworth T, Connor R, Davies R, Devlin K, Feltwell T, Gentles S, Hamlin N, Holroyd S, Hornsby T, Jagels K, Krogh A, McLean J, Moule S, Murphy L, Oliver K, Osborne J, Quail MA, Rajandream MA, Rogers J, Rutter S, Seeger K, Skelton J, Squares R, Squares S, Sulston JE, Taylor K, Whitehead S, Barrell BG (1998) Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature 393:537–544
Maas WK (2007) The potential for the formation of the arginine biosynthetic enzymes and its masking during evolution. Bioessays 29:484–488
Davies RL, MacCorquodale R, Caffrey B (2003) Diversity of avian Pasteurella multocida strains based on capsular PCR typing and variation of the OmpA and OmpH outer membrane proteins. Vet Microbiol 91:169–182
Dumetz F, Duchaud E, LaPatra SE, Le Marrec C, Claverol S, Urdaci MC, Le Hénaff M (2006) A protective immune response is generated in rainbow trout by an OmpH-like surface antigen (P18) of Flavobacterium psychrophilum. Appl Environ Microbiol 72:4845–4852
Finco O, Bonci A, Agnusdei M, Scarselli M, Petracca R, Norais N, Ferrari G, Garaguso I, Donati M, Sambri V, Cevenini R, Ratti G, Grandi G (2005) Identification of new potential vaccine candidates against Chlamydia pneumoniae by multiple screenings. Vaccine 23:1178–1188
Sanchez-Campillo M, Bini L, Comanducci M, Raggiaschi R, Marzocchi B, Pallini V, Ratti G (1999) Identification of immunoreactive proteins of Chlamydia trachomatis by Western blot analysis of a two-dimensional electrophoresis map with patient sera. Electrophoresis 20:2269–2279
Havlasová J, Hernychová L, Halada P, Pellantová V, Krejsek J, Stulík J, Macela A, Jungblut PR, Larsson P, Forsman M (2002) Mapping of immunoreactive antigens of Francisella tularensis live vaccine strain. Proteomics 2:857–867
Verma S, Xiong Y, Mayer MU, Squier TC (2007) Remodeling of the bacterial RNA polymerase supramolecular complex in response to environmental conditions. Biochemistry 46:3023–3035
Norbeck DW, Rosenbrook W, Kramer JB, Grampovnik DJ, Lartey PA (1989) A novel prodrug of an impermeant inhibitor of 3-deoxy-D-manno-2-octulosonate cytidylyltransferase has antibacterial activity. J Med Chem 32:625–629
Toman R, Hussein A, Slabá K, Skultéty E (2003) Further structural characteristics of the lipopolysaccharide from Coxiella burnetii strain nine mile in low virulent phase II. Acta Virol 47:129–130
Honstettre A, Ghigo E, Moynault A, Capo C, Toman R, Akira S, Takeuchi O, Lepidi H, Raoult D, Mege JL (2004) Lipopolysaccharide from Coxiella burnetii is involved in bacterial phagocytosis, filamentous actin reorganization, and inflammatory responses through Toll-like receptor 4. J Immunol 172:3695–3703
Shannon JG, Howe D, Heinzen RA (2005) Lack of dendritic cell maturation following infection by Coxiella burnetii synthesizing different lipopolysaccharide chemotypes. Ann N Y Acad Sci 1063:154–160
Skultéty L, Hernychová L, Toman R, Kroca M, Stulík J, Macela A (2004) Initial peptide mass fingerprinting analysis of proteins obtained by lysis of Coxiella burnetii cells. Acta Virol 48:29–33
Skultéty L, Hernychová L, Toman R, Hubalek M, Slabá K, Zechovska J, Stofanikova V, Lenco J, Stulík J, Macela A (2005) Coxiella burnetii whole cell lysate protein identification by mass spectrometry and tandem mass spectrometry. Ann N Y Acad Sci 1063:115–122
Zhang G, Kiss K, Seshadri R, Hendrix LR, Samuel JE (2004) Identification and cloning of immunodominant antigens of Coxiella burnetii. Infect Immun 72:844–852
Fenollar F, Lepidi H, Raoult D (2001) Whipple’s endocarditis: review of the literature and comparisons with Q fever, Bartonella infection, and blood culture-positive endocarditis. Clin Infect Dis 33:1309–1316
Fenollar F, Fournier PE, Raoult D (2004) Molecular detection of Coxiella burnetii in the sera of patients with Q fever endocarditis or vascular infection. J Clin Microbiol 42:4919–4924
Landais C, Fenollar F, Constantin A, Cazorla C, Guilyardi C, Lepidi H, Stein A, Rolain JM, Raoult D (2007) Q fever osteoarticular infection: four new cases and a review of the literature. Eur J Clin Microbiol Infect Dis 26:341–347
Acknowledgements
This work was partly supported by VEGA grant nos. 2/5053/5, 2/6151/26 and 2/0016/08 from the Slovak Academy of Sciences, Bratislava, Slovakia.
Conflicts of interest
We declare that the authors have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sekeyová, Z., Kowalczewska, M., Decloquement, P. et al. Identification of protein candidates for the serodiagnosis of Q fever endocarditis by an immunoproteomic approach. Eur J Clin Microbiol Infect Dis 28, 287–295 (2009). https://doi.org/10.1007/s10096-008-0621-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-008-0621-4