Abstract
We sought to evaluate the safety and feasibility of inhaled aminoglycosides or colistin in cancer patients with ventilator-associated pneumonia (VAP) due to Gram-negative bacteria (GNB). A retrospective case-matched study was obtained after obtaining IRB approval in patients at the intensive care unit at our NCI-designated comprehensive cancer center between 1999 and 2005. Sixteen patients with GNB-VAP who received inhaled aminoglycosides or colistin were compared with 16 patients who had received these antibiotics intravenously alone. Eligible patients were required to have received at least six doses of inhaled therapy, or 3 or more days of intravenous therapy. Clinical Pulmonary Infection Scores were used to assess pneumonia severity. Standard ATS criteria were used to define VAP. Patients treated with inhaled antibiotics were less likely to have received corticosteroids (13% vs 50%; P < 0.02) and had a higher median baseline creatinine level (0.85 vs 0.6 mg/dL; P < 0.02) than patients treated intravenously. Pseudomonas aeruginosa (69%) was the most common cause of VAP. There were no serious adverse events associated with inhaled antibiotics. Patients who received these antibiotics intravenously developed renal dysfunction (31%); none of the patients treated with inhaled antibiotics developed nephrotoxicity (P ≤ 0.04). Patients treated with inhaled antibiotics were more likely to have complete resolution of clinical (81% vs 31% in the intravenous antibiotic group; P < 0.01) and microbiologic infection (77% vs 8% in the intravenous antibiotic group: P < 0.0006). In a multivariate analysis adjusted for corticosteroid use, inhaled antibiotic therapy was predictive of complete clinical resolution (odds ratio [OR], 6.3; 95% confidence interval [CI], 1.1, 37.6; P < 0.04) and eradication of causative organisms (OR 36.7; 95% CI, 3.3, 412.2; P < 0.003). In critically ill cancer patients with Gram-negative VAP, inhaled aminoglycosides were tolerated without serious toxicity and may lead to improved outcome.
Similar content being viewed by others
Introduction
Pneumonia is a serious complication in critically ill cancer patients receiving antineoplastic therapy [1]. Prolonged mechanical ventilation and the devices needed to maintain the patency of the upper respiratory tract significantly increase the risk of lower respiratory tract infection in critically ill patients. In fact, ventilator-associated pneumonias (VAPs) account for approximately half of all infections acquired during critical care unit stays and are associated with high mortality rates (20–50%) [2, 3]. Furthermore, owing to the prolonged use of multiple broad-spectrum antibiotics in many critically ill patients, drug-resistant bacteria are increasingly common pathogens in critical care units [4, 5]. The treatment of VAP in critical care unit patients thus poses several challenges:
-
1.
Infections are often due to drug-resistant bacteria such as methicillin-resistant Staphylococcus aureus, and non-fermentative Gram-negative bacteria (GNB), including Pseudomonas, Acinetobacter, Stenotrophomonas species
-
2.
Few drugs are effective against these organisms
-
3.
Drugs such as vancomycin and the aminoglycosides, which are effective against other types of drug-resistant infections, have poor lung tissue penetration in patients with serious pulmonary infections [6–8]
One way of overcoming the tissue penetration limitation would be to deliver drug concentrations directly to the site of infection. In fact, aerosolized drug delivery has transformed the quality of life in patients with cystic fibrosis; regular use of inhaled tobramycin by these patients reduces lower respiratory tract colonization and recurrent infection due to GNB [9]. In addition, tobramycin and colistin have also been successfully used in the treatment of nosocomial pneumonia due to drug-resistant GNB [10–12]. However, the safety and efficacy of inhaled aminoglycosides and colistin remain limited in critically immunosuppressed patients with VAP and underlying malignancy.
We sought to determine the safety and efficacy of aerosolized aminoglycosides and colistin in critically ill patients with VAP due to GNB (GNB-VAP) at our National Cancer Institute-designated comprehensive cancer center.
Materials and methods
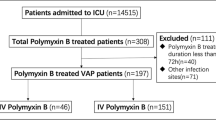
Study setting, patients, and design
This retrospective study was performed at The University of Texas M. D. Anderson Cancer Center after obtaining permission from the institutional review board. Patients with culture-documented GNB-VAP who had received inhaled or intravenous aminoglycosides or colistin between January 1999 and April 2006 were identified through a database search. Eligible patients were required to have received at least six doses of inhaled therapy or ≥ 3 days of intravenous therapy [13]. Patients were given inhaled antibiotic therapy mostly in consultation with Infectious Diseases if they were:
-
1.
Critically ill
-
2.
Had multicentric lung infection
-
3.
Had infection due to drug-resistant, Gram-negative bacteria
-
4.
Had a history of drug-induced or cancer-related renal damage and considered at high risk of aminoglycoside- or colistin-induced renal failure
Patients who had received inhaled and intravenous preparation of the same drug, concurrently or sequentially, were not included in the analysis.
Patient and laboratory data were retrieved from computerized medical records; in patients who had GNB-VAP prior to 2003, paper charts were also reviewed. The following clinical information was retrieved: demographics, underlying malignancy, duration of critical unit stay and of mechanical ventilatory assistance; neutropenia (defined as absolute neutrophil count < 500 neutrophils/mm3); comorbidities including chronic lung disease, diabetes mellitus, renal failure; splenectomy; ventilator dependency; use of systemic corticosteroids and antibiotics 1 week prior to and/or during the infection episode; duration and dose of GNB-VAP therapy; antineoplastic therapy; source of diagnostic culture; antimicrobial susceptibility; treatment-associated adverse events; and clinical and microbiologic outcome.
Clinical Pulmonary Infection Scores (CPIS) were used to assess the severity of pneumonia [14]. The CPIS were retrospectively calculated at the beginning of and after completion of therapy using the following parameters, as described elsewhere [14]: body temperature, peripheral blood leukocyte count, PaO2/FiO2 ratio, chest radiograph, and microbiologic culture results.
Drug-induced bronchospasm was determined by reviewing assessments by the respiratory therapist in charts before, during, and following administration of inhaled antibiotic therapy. Nurses’ and physicians’ progress notes were also assessed for the possibility of a delayed reaction to the inhaled antibiotics. Respiratory rates and fractional inspired oxygen concentration (FiO2) before and after inhaled therapy were reviewed for post-treatment changes.
Definitions
Pneumonia was considered to be ventilator-associated if onset occurred after receipt of mechanical ventilation for at least 48 h and the infection was judged not to have been incubating before the initiation of mechanical ventilation. Standard VAP diagnosis criteria were used [2, 15]. Pneumonia was diagnosed on the basis of a radiographic finding of a new and progressive pulmonary consolidation and at least two of the following clinical criteria: a body temperature > 38°C, leukocytosis (>10,000 cells/µL) or leukopenia (<4000 cells/µL), and clinical evidence suggestive of pneumonia such as purulent bronchial secretions and a decrease in oxygenation [2]. Isolates were regarded as multidrug-resistant if they had intermediate susceptibility or resistance to at least three drugs in the following classes: beta-lactams, carbapenems, aminoglycosides, and fluoroquinolones.
The response to treatment was assessed at the time of discharge from the critical care unit or at the end of antimicrobial GNB-VAP therapy, especially if the patient remained hospitalized for a non-GNB-VAP-related event. Clinical responses were classified as complete resolution of GNB-VAP; partial resolution, which included improved clinical parameters (fever defervescence, suctioning requirements, symptoms and signs of pneumonia), ventilator parameters and laboratory findings (improved blood gases, normalization of white blood cell count), and/or receding pulmonary infiltrates on a chest radiograph at the end of therapy; or failure, which was defined as worsening of the clinical and ventilator parameters and/or progression of contiguous or non-contiguous consolidation on radiography at the end of therapy. Microbiologic response was defined as eradication of causative organisms in patients in whom a follow-up culture was obtained at the end of therapy. Persistent infection was defined as continued isolation of the original disease-associated pathogen after 2 weeks of GNB-VAP therapy. VAP-associated death was defined as death attributed to progressive lung infection and/or secondary complications arising from uncontrolled infection such as lung abscess, empyema, complicated parapneumonic pleural effusion in the absence of known non-infection-associated terminal events such as severe myocardial infarction, intracranial bleeding, or gastrointestinal hemorrhage.
Renal dysfunction was defined as the doubling of serum creatinine in patients with pretreatment (baseline) creatinine clearance of ≥30 mL/min or an increase in creatinine by ≥1 mg/dL at the end of therapy in patients with pretreatment creatinine clearance < 30 mL/min.
Inhaled antimicrobials
When inhaled tobramycin was prescribed, FDA-approved preparation of inhaled tobramycin (Tobi®; Chiron, Emeryville, CA, USA; 300 mg per 5-mL container) was used. When another inhaled aminoglycoside or colistin was prescribed, the institutional pharmacy dispensed nebulized formulas made from commercially available intravenous preparations in the following strengths: amikacin (100 mg per 3-mL intravenous dose), gentamicin (40 mg per mL intravenous dose), and colistin (75 mg per 4-mL intravenous dose). Inhaled colistin was delivered at the dose of 100 mg every 8 h; tobramycin, 300 mg twice daily (b.i.d.); gentamicin, 100 mg three times daily (t.i.d.); and amikacin, 100 mg t.i.d. or 300 mg b.i.d. A jet nebulizer was adapted to the ventilatory circuit, and during antibiotic administration, the patient’s vital signs, oxygen saturation, ventilatory parameters were carefully monitored by a respiratory therapist and critical care unit nurse. Patients received inhaled beta-agonist bronchodilators before and after therapy.
Statistical analysis
The Chi-squared or Fisher’s exact test was used to assess differences in categorical variables, as appropriate. Differences in continuous variables were assessed by Student’s t test or Wilcoxon rank-sum test. All tests were two-sided, and statistical significance was set at P ≤ 0.05. Multivariate logistic regression analysis was used to assess the independent effect of therapy on each of the three outcomes: clinical resolution, microorganism eradication, and renal failure. All the statistical analyses were performed using SAS version 9.1 (SAS Institute, Cary, NC, USA).
Results
In cancer patients at our critical care unit the rate of VAP has declined considerably from 34.2 VAP/1,000 ventilator days in 1999 to 10.1 and 8.6 VAP/1,000 ventilator days in 2005 and 2006 respectively, after multifaceted infection control measures, including oral care policy, inline suction, respiratory care focus to reduce ventilator days, and a hand hygiene initiative were instituted. Gram-negative bacteria remain the most frequent (approximately 60%) cause of VAP in critically ill patients at our institution.
Patient and disease characteristics
Thirty-two patients who met the study criteria were identified. The patients who received inhaled aminoglycosides or colistin (n = 16) and those who received these antibiotics intravenously (n = 16) were similar, as shown in Table 1. However, patients in whom GNB-VAP was treated with inhaled antibiotics were significantly less likely to have received systemic corticosteroids within 1 week before or during therapy for GNB-VAP (13% vs 50%; P ≤ 0.02) and had a higher median serum creatinine level prior to GNB-VAP therapy (0.85 vs 0.6 mg/dL; P ≤ 0.02) than patients who received intravenous antibiotics. There were no differences in comorbidities or underlying malignancies between the two groups (Table 1). Only one patient with amyotrophic lateral sclerosis and ventilator dependency had a prior history of VAP.
Table 2 shows the causative organisms, treatment, and responses for the 32 patients. The most common organism associated with GNB-VAP was Pseudomonas aeruginosa (n = 22; 69%). Klebsiella pneumoniae was the second most common organism (n = 5; 16%). One patient (6%) in the inhaled group had concurrent P. aeruginosa bacteremia and in the intravenous treatment group, 2 patients (13%) were bacteremic with P. aeruginosa and K. Pneumoniae.
Fourteen patients received intravenous aminoglycosides, 13 patients received inhaled aminoglycosides, and 2 patients in each group received colistin. One patient with Pseudomonas aeruginosa was treated with a combination of inhaled colistin and tobramycin for 26 days; this patient also received systemic imipenem. The median duration of therapy was comparable in the two groups: a median of 9 ± 5 (range, 2–21) days in the intravenous therapy group vs 11 ± 6 (range, 3–26) days in the inhaled therapy group (P > 0.5).
Adverse events
No adverse events were associated with inhaled antibiotics therapy, notably no bronchoconstriction or apnea. However, 5 patients who received intravenous aminoglycosides developed drug-induced renal dysfunction (31% vs 0%; P ≤ 0.04). The median serum creatinine levels at the end of therapy in patients treated with intravenous aminoglycosides and colistin was 0.85 (range, 0.5–5.0) mg/dL and in patients who received inhaled antibiotics creatinine levels were 0.75 (range, 0.2–2.9) mg/dL.
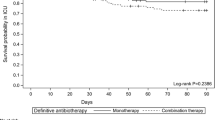
Response to therapy
A significantly greater percentage of patients treated with inhaled antibiotics had complete clinical resolution than patients treated with intravenous antibiotics (100% [n = 13 out of 13] vs 55% [n = 5 out of 9]; P < 0.01). Also, bacterial eradication in patients in whom follow-up lower respiratory tract cultures were available was significantly more frequent in patients who had been treated with inhaled antibiotics (77% [n = 10 out of 13] vs 8% [n = 1 out of 12] in those with intravenous therapy alone; P < 0.0006). In addition, the mean CPIS at the end of therapy was more favorable in patients treated with inhaled antibiotics (3 ± 1.7 vs 4 ± 2.6; P ≤ 0.04).
Logistic regression analysis
The logistic regression model used was adjusted for renal failure, concordant antibiotic use (concordant refers to intravenous antibiotics that were active against the GNB in both arms), corticosteroid use, lung cancer, radiation therapy, comorbidities, CPIS, Gram-negative rod species, and duration of critical care unit stay. The likelihood of a complete clinical resolution (odds ratio [OR], 6.3; 95% confidence interval [CI], 1.1, 37.6; P ≤ 0.04) and of eradication of the causative organisms (OR, 36.7; 95% CI, 3.3, 412.2; P ≤ 0.003) was significantly greater in patients treated with inhaled antibiotics.
Discussion
In this study, critically ill cancer patients with GNB-VAP treated with inhaled aminoglycosides and/or colistin had significantly better outcomes than patients who received these antibiotics intravenously. Furthermore, the inhaled antibiotics were tolerated without serious adverse events, such as sustained drug-induced bronchospasm, increased requirements for supplemental oxygen, or nephrotoxicity.
The concerns regarding the intravenous antimicrobial preparation used for aerosolized delivery includes optimal osmolality, alkalinity, and ionic strength of the preparation, which may lead to irritation of the respiratory mucosa [16]. In our patients, however, aerosolization of these intravenous antimicrobial preparations was tolerated without any serious adverse events.
Aerosolized drug delivery to the lungs has been extensively evaluated in patients with cystic fibrosis and recipients of heart-lung transplants [9]. Inhaled aminoglycosides lead to high drug concentrations in the lung tissue, especially in patients given treatments during mechanical ventilation; in contrast, serum drug concentrations in these individuals are negligible [17, 18]. Geller et al. found that 95% of patients with cystic fibrosis treated with inhaled tobramycin achieved 25 times the minimum inhibitory concentration (MIC) for Pseudomonas species in sputum samples, whereas serum tobramycin levels remained negligible [19]. The higher drug concentration in the bronchial space may further improve antimicrobial efficacy, especially for the antimicrobial agents that require high drug concentration for effective bacterial killing. Effective drug delivery to the bronchoalveolar space in patients with pulmonary infection may improve treatment response due to the following:
-
1.
A decrease in the volume of the tracheobronchial secretions
-
2.
A decline in the viable bacteria
-
3.
Reduction in proinflammatory cytokines such as interleukin-1β and tumor necrosis factor α from neutrophils, macrophages, and lymphocytes
-
4.
By promoting epithelial-derived soluble intercellular adhesion molecule-1 (sICAM-1) [17]
The increased sICAM-1 represents a decline in the proinflammatory, neutrophil-derived elastases. Besides providing selective bronchopulmonary delivery of high drug concentrations, aerosolized aminoglycoside therapy, especially in critically ill patients with pneumonia, may abrogate the host’s dysregulated inflammatory response by down-regulating macrophage-derived mediators of inflammation, which are crucial for neutrophil recruitment and activation at the site of infection.
The use of aerosolized antibiotics to prevent pneumonia in patients requiring prolonged mechanical ventilation was previously considered ineffective owing to poor tissue penetration [20, 21]. However, research in the 1990s challenged this belief and showed that aerosolized drugs, especially in mechanically ventilated patients, may lead to > 20% of the total inhaled drug concentration in lung tissue [17, 22]. In spontaneously breathing patients with cystic fibrosis, this deposition may range from 10 to 20% of the total aerosolized dose [23, 24]. The improved drug delivery critically depends on the size of aerosolized drug particles, as smaller particles may be exhaled, whereas the particles between 1 and 5 µm get deposited in the lower respiratory tract [16]. The jet nebulizer currently used in this study leads to delivery of particles within 1 to 5 µm in size.
Inhaled tobramycin is routinely used in cystic fibrosis patients with bronchiectasis and has been associated with a significant decline in infection-related hospitalization, attributed to a substantial reduction in lower respiratory tract bacterial colonization [25]. Similarly, the clinical experience with aerosolized colistin for the treatment of Pseudomonas aeruginosa and Acinetobacter baumannii in patients with VAP has also been encouraging [13, 26]. In patients without cystic fibrosis, such as those undergoing thoracic surgery for lung cancer, the mean lung concentration following inhaled 300 mg tobramycin ranges from 4 to 6 μg/g lung tissue [27]. The high drug concentration within lung tissue is achieved in the setting of negligible serum drug levels, and may improve bacterial elimination, even for less susceptible microorganisms with higher MICs [27].
Furthermore, inhaled aminoglycosides may disrupt bacterial biofilm formation [28, 29]. The biofilm that are formed on all foreign material such as endotracheal tubes within a few hours of insertion, serves as an important reservoir for microorganisms to evade the host’s immune surveillance and also as a barrier for antimicrobial killing.
Drug resistance following intermittent exposure to inhaled antibiotics has been a concern. Pseudomonas, Stenotrophomonas, and Acinetobacter species have a high potential for developing resistance spontaneously or after exposure to sub-therapeutic drug levels. This has, however, not been noted in patients treated with aerosolized antibiotic therapy for the prevention and/or treatment of GNB pneumonia [30]. Similarly, in cancer patients with GNB-VAP who were treated with aerosolized aminoglycosides or colistin, we did not encounter breakthrough infections due to multidrug-resistant bacteria.
In our study, treatment with aerosolized aminoglycosides and/or colistin in immunosuppressed cancer patients, even in those with reduced renal function, was well tolerated and none of the 16 patients who were treated with aerosolized, potentially nephrotoxic antimicrobials developed renal dysfunction, whereas nearly a third of patients treated with these drugs given intravenously developed renal failure. The limitation of a retrospective study apply to this observation, as selection of patients with VAP could not be standardized and potentially less serious adverse events may not have been captured and documented in patients’ electronic medical records.
In conclusion, inhalation therapy with aminoglycosides and/or colistin in cancer patients with GNB-VAP was associated with a favorable response and was tolerated without serious pulmonary or renal toxicity. Further studies are needed to evaluate this treatment approach in patients with difficult-to-treat lung infections.
References
Safdar A, Armstrong D (2001) Infectious morbidity in critically ill patients with cancer. Crit Care Clin 17:531–570
American Thoracic Society and Infectious Diseases Society of America (2005) Guidelines for the management of adults with hospital-acquired, ventilator-associated, and healthcare-associated pneumonia. Am J Respir Crit Care Med 171:388–416
National Nosocomial Infections Surveillance (NNIS) (1999) System report, data summary from January 1990–May 1999, issued June 1999. Am J Infect Control 27:520–532
Porzecanski I, Bowton DL (2006) Diagnosis and treatment of ventilator-associated pneumonia. Chest 130:597–604
Davis KA (2006) Ventilator-associated pneumonia: a review. J Intensive Care Med 21:211–216
Kiem S, Schentag JJ (2006) Relationship of minimal inhibitory concentration and bactericidal activity to efficacy of antibiotics for treatment of ventilator-associated pneumonia. Semin Respir Crit Care Med 27:51–67
Brun-Buisson C, Lemaire F (2001) Administration of antibiotics for pneumonia during respiratory failure: reaching the target. Am J Respir Crit Care Med 164:1554–1555
Schmidt-loanas M, de Roux A, Lode H (2005) New antibiotics for the treatment of severe staphylococcal infection in the critically ill patients. Curr Opin Crit Care 11:481–486
Canton R, Cobos N, de Gracia J, Baquero F, Honorato J, Gartner S et al (2005) Antimicrobial therapy for pulmonary pathogenic colonization and infection by Pseudomonas aeruginosa in cystic fibrosis patients. Clin Microbiol Infect 11:690–703
Brown RB, Kruse JA, Counts GW, Russell JA, Christou NV, Sands ML (2005) Double-blind study of endotracheal tobramycin in the treatment of gram-negative bacterial pneumonia. Antimicrob Agents Chemother 34:269–272
Kwa AL, Loh C, Low JG, Kurup A, Tam VH (2005) Nebulized colistin in the treatment of pneumonia due to multidrug-resistant Acinetobacter baumannii and Pseudomonas aeruginosa. Clin Infect Dis 41:754–757
Hamer DH (2000) Treatment of nosocomial pneumonia and tracheobronchitis caused by multidrug-resistant Pseudomonas aeruginosa with aerosolized colistin. Am J Respir Crit Care Med 162:328–330
Michalopoulos A, Kasiakou SK, Mastora Z, Rellos K, Kapaskelis AM, Falagas ME (2005) Aerosolized colistin for the treatment of nosocomial pneumonia due to multidrug-resistant gram-negative bacteria in patients without cystic fibrosis. Crit Care 9:R53–R59
Luna CM, Blanzaco D, Niederman MS, Matarucco W, Baredes NC, Desmery P et al (2003) Resolution of ventilator-associated pneumonia: prospective evaluation of the clinical pulmonary infection score as an early clinical predictor of outcome. Crit Care Med 31:676–682
Jarvis WR, Edwards JR, Culver DH, Hughes JM, Horan T, Emori TG et al (1991) Nosocomial infection rates in adult and pediatric intensive care units in the United States. National Nosocomial Infections Surveillance System. Am J Med 91:185–191
Conrad DJ (2003) The clinical use of aerosolized antibiotics. Clin Pulm Med 10:201–207
Palmer LB, Smaldone GC, Simon SR, O’Riordan TG, Cuccia A (1998) Aerosolized antibiotics in mechanically ventilated patients: delivery and response. Crit Care Med 26:31–39
Goldstein I, Chastre J, Rouby JJ (2006) Novel and innovative strategies to treat ventilator-associated pneumonia: optimizing the duration of therapy and nebulizing antimicrobial agents. Semin Respir Crit Care Med 27:82–91
Geller DE, Pitlick WH, Nardella PA, Tracewell WG, Ramsey BW (2002) Pharmacokinetics and bioavailability of aerosolized tobramycin in cystic fibrosis. Chest 122:219–226
Fuller HD, Dolovich MB, Posmituck G, Pack WW, Newhouse MT (1989) Pressurized aerosol versus jet aerosol delivery to mechanically ventilated patients. Am Rev Respir Dis 141:440–444
MacIntyre NR, Silver RM, Miller CW, Schuler F, Colman RE (1985) Aerosol delivery to intubated, mechanically ventilated patients. Crit Care Med 13:81–84
Palmer LB, Smaldone GC, Simon S, O’Riordan T, Morra L (1995) Tracheal aspirate in long-term mechanically ventilated patients. A human model of gram-negative infection and airway inflammation. Chest 108:1326–1332
Ilowite JS, Gorvoy JD, Smaldone GC (1987) Quantitative deposition of aerosolized gentamicin in cystic fibrosis. Am Rev Respir Dis 136:1445–1449
Smaldone GC, Fuhrer JT, Steigbigel RT, McPeck M (1991) Factors determining pulmonary deposition of aerosolized pentamidine in patients with human immunodeficiency virus infection. Am Rev Respir Dis 143:727–737
Drobnic ME, Sune P, Montoro JB, Ferrer A, Orriols R (2005) Inhaled tobramycin in non-cystic fibrosis patients with bronchiectasis and chronic bronchial infection with Pseudomonas aeruginosa. Ann Pharmacother 39:39–44
Linden P, Paterson DL (2006) Parenteral and inhaled colistin for treatment of ventilator-associated pneumonia. Clin Infect Dis 43:S89–S94
Le Conte P, Potel G, Peltier P, Horeau D, Caillon J, Juvin ME et al (1993) Lung distribution and pharmacokinetics of aerosolized tobramycin. Am Rev Respir Dis 147:1279–1282
Adair CG, Gorman SP, O’Neill FB, McClurg B, Goldsmith EC, Webb CH (1993) Selective decontamination of the digestive tract (SDD) does not prevent the formation of microbial biofilms on endotracheal tubes. J Antimicrob Chemother 31:689–697
Adair CG, Gorman SP, Byers LM, Jones DS, Feron B, Crowe M et al (2002) Eradication of endotracheal tube biofilm by nebulised gentamicin. Intensive Care Med 28:426–431
Lesho E (2005) Role of inhaled antibacterials in hospital-acquired and ventilator-associated pneumonia. Expert Rev Anti Infect Ther 3:445–451
Acknowledgments
This research was supported in part by the Cancer Center Support Grant CA16672 from the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ghannam, D.E., Rodriguez, G.H., Raad, I.I. et al. Inhaled aminoglycosides in cancer patients with ventilator-associated Gram-negative bacterial pneumonia: safety and feasibility in the era of escalating drug resistance. Eur J Clin Microbiol Infect Dis 28, 253–259 (2009). https://doi.org/10.1007/s10096-008-0620-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-008-0620-5