Abstract
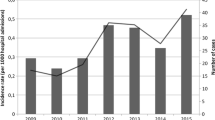
The aim of this study was to review fungal bloodstream infections at a large tertiary care hospital to evaluate the incidence of fungemia and the distribution of causative species during the period 2001–2005. Another aim was to assess the extent of antifungal resistance. A review of all episodes of fungemia at the University Hospitals of Leuven (Belgium) was conducted between January 2001 and December 2005. For the first yeast isolate collected from each non-mould fungemic episode during a 1-year period (June 2004–June 2005), susceptibility to seven antifungal agents was determined using Sensititre YeastOne plates (Trek Diagnostic Systems, East Grinstead, UK), and the antifungal therapy was reviewed. The annual incidence of fungemia ranged between 1.30 and 1.68 episodes per 10,000 patient-days (on a total of 2,680,932 patient-days), with a decreasing trend observed over the 5-year study period. The most common species were Candida albicans (59%), Candida glabrata (22%), Candida parapsilosis (10%), and Candida tropicalis (4%). Overall, fluconazole resistance was rare (1.6%) and was detected only in C. glabrata and C. krusei. Voriconazole and caspofungin inhibited 100% of the isolates at a concentration of ≤1 μg/ml. Fluconazole was used to treat 75% of fungemic patients. Caspofungin was the second most commonly used antifungal agent (used to treat 11.7% of patients). The incidence of fungemia was higher than usually reported in other European countries. The low proportion of resistance supports the use of fluconazole as the treatment of first choice for candidemia in patients not previously exposed to this drug.

Similar content being viewed by others
References
Zaoutis TE, Argon J, Chu J, Berlin JA, Walsh TJ, Feudtner C (2005) The epidemiology and attributable outcomes of candidemia in adults and children hospitalized in the United States: a propensity analysis. Clin Infect Dis 41:1232–1239
Chen S, Slavin M, Nguyen Q, Marriott D, Playford EG, Ellis D, Sorrell T (2006) Active surveillance for candidemia, Australia. Emerg Infect Dis 12:1508–1516
Banerjee SN, Emori TG, Culver DH, Gaynes RP, Jarvis WR, Horan T et al (1991) Secular trends in nosocomial primary bloodstream infections in the United States, 1980–1989. National Nosocomial Infections Surveillance System. Am J Med 91:86S–89S
Sobel JD (2006) The emergence of non-albicans Candida species as causes of invasive candidiasis and candidemia. Curr Infect Dis Rep 8:427–433
Trick WE, Fridkin SK, Edwards JR, Hajjeh RA, Gaynes RP (2002) Secular trend of hospital-acquired candidemia among intensive care unit patients in the United States during 1989–1999. Clin Infect Dis 35:627–630
Tortorano AM, Kibbler C, Peman J, Bernhardt H, Klingspor L, Grillot R (2006) Candidaemia in Europe: epidemiology and resistance. Int J Antimicrob Agents 27:359–366
Tortorano AM, Peman J, Bernhardt H, Klingspor L, Kibbler CC, Faure O et al (2004) Epidemiology of candidaemia in Europe: results of 28-month European Confederation of Medical Mycology (ECMM) hospital-based surveillance study. Eur J Clin Microbiol Infect Dis 23:317–322
Swinne D, Watelle M, Suetens C, Mertens K, Fonteyne PA, Nolard N (2004) A one-year survey of candidemia in Belgium in 2002. Epidemiol Infect 132:1175–1180
Clinical and Laboratory Standards Institute (2006) Quality control minimal inhibitory concentration (MIC) limits for broth microdilution and MIC interpretive breakpoints. Supplement M44-S1. CLSI, Wayne, PA
Hajjeh RA, Sofair AN, Harrison LH, Lyon GM, Arthington-Skaggs BA, Mirza SA et al (2004) Incidence of bloodstream infections due to Candida species and in vitro susceptibilities of isolates collected from 1998 to 2000 in a population-based active surveillance program. J Clin Microbiol 42:1519–1527
Marchetti O, Bille J, Fluckiger U, Eggimann P, Ruef C, Garbino J et al (2004) Epidemiology of candidemia in Swiss tertiary care hospitals: secular trends, 1991–2000. Clin Infect Dis 38:311–320
Richet H, Roux P, Des CC, Esnault Y, Andremont A (2002) Candidemia in French hospitals: incidence rates and characteristics. Clin Microbiol Infect 8:405–412
Bedini A, Venturelli C, Mussini C, Guaraldi G, Codeluppi M, Borghi V et al (2006) Epidemiology of candidaemia and antifungal susceptibility patterns in an Italian tertiary-care hospital. Clin Microbiol Infect 12:75–80
Almirante B, Rodriguez D, Park BJ, Cuenca-Estrella M, Planes AM, Almela M et al (2005) Epidemiology and predictors of mortality in cases of Candida bloodstream infection: results from population-based surveillance, Barcelona, Spain, from 2002 to 2003. J Clin Microbiol 43:1829–1835
Viscoli C, Girmenia C, Marinus A, Collette L, Martino P, Vandercam B et al (1999) Candidemia in cancer patients: a prospective, multicenter surveillance study by the Invasive Fungal Infection Group (IFIG) of the European Organization for Research and Treatment of Cancer (EORTC). Clin Infect Dis 28:1071–1079
Cuenca-Estrella M, Rodriguez D, Almirante B, Morgan J, Planes AM, Almela M et al (2005) In vitro susceptibilities of bloodstream isolates of Candida species to six antifungal agents: results from a population-based active surveillance programme, Barcelona, Spain, 2002–2003. J Antimicrob Chemother 55:194–199
Pfaller MA, Messer SA, Boyken L, Tendolkar S, Hollis RJ, Diekema DJ (2004) Geographic variation in the susceptibilities of invasive isolates of Candida glabrata to seven systemically active antifungal agents: a global assessment from the ARTEMIS Antifungal Surveillance Program conducted in 2001 and 2002. J Clin Microbiol 42:3142–3146
Swinne D, Watelle M, Van der Flaes FM, Nolard N (2004) In vitro activities of voriconazole (UK-109,496), fluconazole, itraconazole and amphotericin B against 132 non-albicans bloodstream yeast isolates (CANARI Study). Mycoses 47:177–183
Arendrup MC, Fuursted K, Gahrn-Hansen B, Jensen IM, Knudsen JD, Lundgren B et al (2005) Seminational surveillance of fungemia in Denmark: notably high rates of fungemia and numbers of isolates with reduced azole susceptibility. J Clin Microbiol 43:4434–4440
Fleck R, Dietz A, Hof H (2007) In vitro susceptibility of Candida species to five antifungal agents in a German university hospital assessed by the reference broth microdilution method and E test. J Antimicrob Chemother 59:767–771
Pfaller MA, Diekema DJ, Messer SA, Boyken L, Hollis RJ (2003) Activities of fluconazole and voriconazole against 1,586 recent clinical isolates of Candida species determined by broth microdilution, disk diffusion, and E test methods: report from the ARTEMIS Global Antifungal Susceptibility Program, 2001. J Clin Microbiol 41:1440–1446
Morace G, Amato G, Bistoni F, Fadda G, Marcone P, Montagna MT et al (2002) Multicenter comparative evaluation of six commercial systems and the National Committee for Clinical Laboratory Standards M27-A broth microdilution method for fluconazole susceptibility testing of Candida species. J Clin Microbiol 40:2953–2958
Davey KG, Szekely A, Johnson EM, Warnock DW (1998) Comparison of a new commercial colorimetric microdilution method with a standard method for in-vitro susceptibility testing of Candida spp. and Cryptococcus neoformans. J Antimicrob Chemother 42:439–444
Canton E, Peman J, Gobernado M, Alvarez E, Baquero F, Cisterna R et al (2005) Sensititre YeastOne caspofungin susceptibility testing of Candida clinical isolates: correlation with results of NCCLS M27-A2 multicenter study. Antimicrob Agents Chemother 49:1604–1607
Espinel-Ingroff A, Canton E, Gibbs D, Wang A (2007) Correlation of Neo-Sensitabs tablet diffusion assay on three media, with CLSI broth microdilution M27-A2 and disk diffusion M44-A methods for susceptibility testing of Candida spp. and Cryptococcus neoformans, with amphotericin B, caspofungin, fluconazole, itraconazole, and voriconazole. J Clin Microbiol 45:858–864
Park BJ, Arthington-Skaggs BA, Hajjeh RA, Iqbal N, Ciblak MA, Lee-Yang W et al (2006) Evaluation of amphotericin B interpretive breakpoints for Candida bloodstream isolates by correlation with therapeutic outcome. Antimicrob Agents Chemother 50:1287–1292
Boel A, Cartuyvels R, De Beenhouwer H, Frans J, Oris E, Vandecandelaere P et al (2006) Susceptibility of yeasts isolated from hemocultures in 7 Belgian hospitals. Program and abstracts of the 16th Congress of the International Society for Human and Animal Mycology, Paris, 2006, Abstract no. P-0454
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lagrou, K., Verhaegen, J., Peetermans, W.E. et al. Fungemia at a tertiary care hospital: incidence, therapy, and distribution and antifungal susceptibility of causative species. Eur J Clin Microbiol Infect Dis 26, 541–547 (2007). https://doi.org/10.1007/s10096-007-0339-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-007-0339-8