Abstract
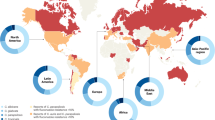
In a randomized study, caspofungin was compared with amphotericin B for the treatment of invasive candidiasis in a total of 239 adults from 56 sites in 20 countries. This study provided a unique opportunity to assess the frequency and outcome of invasive candidiasis caused by different Candida species worldwide, and the results are presented here. Efficacy was primarily assessed at the end of intravenous therapy using a modified intent-to-treat (MITT) analysis. This analysis was performed on 224 of the 239 patients enrolled in the study. Attempts were made to collect baseline Candida isolates from all patients for species identification at a central laboratory. Yeasts were identified to the species level using two commercial systems and microscopic examination. Viable baseline isolates were recovered from 210 of the 224 (94%) patients included in the MITT analysis. Candida albicans was the most frequently isolated species in all regions and was responsible for 45% of cases overall. Nevertheless, the majority of cases of infection were caused by non-albicans Candida species. In the USA and Canada, Candida glabrata was the second most commonly isolated pathogen (18%). In contrast, Candida parapsilosis and Candida tropicalis accounted for 55% of cases in Latin America. Outcomes were comparable for patients treated with caspofungin (74% overall; 64% and 80% for infections due to Candida albicans and non-albicans species) and amphotericin B (62% overall; 58% and 68% for infections due to Candida albicans and non-albicans species), and were generally similar across continents. The distribution of Candida species isolated from patients enrolled in a clinical trial may not be representative of pathogens causing invasive candidiasis in the general population. Nevertheless, our findings may affect the regional choice of empirical antifungal therapy for seriously ill patients with suspected or documented invasive candidiasis since different Candida species have varying susceptibility to conventional antifungal drugs.
Similar content being viewed by others
References
Asmundsdottir LR, Erlendsdottir H, Gottfredsson M (2002) Increasing incidence of candidemia: results from a 20-year nationwide study in Iceland. J Clin Microbiol 40:3489–3492
Diekema DJ, Messer SA, Brueggemann AB, Coffman SL, Doern GV, Herwaldt LA, Pfaller MA (2002) Epidemiology of candidemia: 3-year results from the emerging infections and the epidemiology of Iowa organisms study. J Clin Microbiol 40:1298–1302
Doczi I, Dosa E, Hajdu E, Nagy E (2002) Aetiology and antifungal susceptibility of yeast bloodstream infections in a Hungarian university hospital between 1996 and 2000. J Med Microbiol 51:677–681
Krcmery V, Laho L, Huttova M, Ondrusova A, Kralinsky K, Pevalova L, Dluholucky S, Pisarcikova M, Hanzen J, Filka J, Sejnova D, Liskova A, Purgelova A, Szovenyova Z, Koren P (2002) Aetiology, antifungal susceptibility, risk factors and outcome in 201 fungaemic children: data from a 12-year prospective national study from Slovakia. J Med Microbiol 51:110–116
Macphail GL, Taylor GD, Buchanan-Chell M, Ross C, Wilson S, Kureishi A (2002) Epidemiology, treatment and outcome of candidemia: a five-year review at three Canadian hospitals. Mycoses 45:141–145
Marriott D, Laxton M, Harkness J (2001) Candida dubliniensis candidemia in Australia. Emerg Infect Dis 7:479
Mathews MS, Samuel PR, Suresh M (2001) Emergence of Candida tropicalis as the major cause of fungaemia in India. Mycoses 44:278–280
McMullan R, McClurg R, Xu J, Moore J, Millar B, Crowe M, Hedderwick S (2002) Trends in the epidemiology of Candida bloodstream infections in Northern Ireland between January 1984 and December 2000. J Infect 45:25
Moosa MY, Sobel JD (2002) Non-albicans Candida infections in patients with hematologic malignancies. Semin Respir Infect 17:91–108
Richet H, Roux P, Des CC, Esnault Y, Andremont A (2002) Candidemia in French hospitals: incidence rates and characteristics. Clin Microbiol Infect 8:405–412
Slavin MA (2002) The epidemiology of candidaemia and mould infections in Australia. J Antimicrob Chemother 49 (Suppl 1):3–6
Wu S, Liao W, Guo N (2001) Epidemiological study of pathogenic fungi in China: 1986 and 1996. Chin Med J (Engl) 114:294–296
Alves SH, Milan EP, Branchini ML, Nishimura K, Fukushima K, Oliveira LO, Costa JM, Colombo AL (2001) First isolation of Candida dubliniensis in Rio Grande do Sul, Brazil. Diagn Microbiol Infect Dis 39:165–168
Fairchild KD, Tomkoria S, Sharp EC, Mena FV (2002) Neonatal Candida glabrata sepsis: clinical and laboratory features compared with other Candida species. Pediatr Infect Dis J 21:39–43
Hope W, Morton A, Eisen DP (2002) Increase in prevalence of nosocomial non-Candida albicans candidaemia and the association of Candida krusei with fluconazole use. J Hosp Infect 50:56–65
Pfaller MA, Jones RN, Doern GV, Sader HS, Hollis RJ, Messer SA (1998) International surveillance of bloodstream infections due to Candida species: frequency of occurrence and antifungal susceptibilities of isolates collected in 1997 in the United States, Canada, and South America for the SENTRY Program. The SENTRY Participant Group. J Clin Microbiol 36:1886–1889
Pfaller MA, Jones RN, Doern GV, Fluit AC, Verhoef J, Sader HS, Messer SA, Houston A, Coffman S, Hollis RJ (1999) International surveillance of blood stream infections due to Candida species in the European SENTRY Program: species distribution and antifungal susceptibility including the investigational triazole and echinocandin agents. SENTRY Participant Group (Europe). Diagn Microbiol Infect Dis 35:19–25
Pfaller MA, Jones RN, Doern GV, Sader HS, Messer SA, Houston A, Coffman S, Hollis RJ (2000) Bloodstream infections due to Candida species: SENTRY antimicrobial surveillance program in North America and Latin America, 1997–1998. Antimicrob Agents Chemother 44:747–751
Pfaller MA, Diekema DJ, Jones RN, Sader HS, Fluit AC, Hollis RJ, Messer SA (2001) International surveillance of bloodstream infections due to Candida species: frequency of occurrence and in vitro susceptibilities to fluconazole, ravuconazole, and voriconazole of isolates collected from 1997 through 1999 in the SENTRY antimicrobial surveillance program. J Clin Microbiol 39:3254–3259
Bodey GP, Mardani M, Hanna HA, Boktour M, Abbas J, Girgawy E, Hachem RY, Kontoyiannis DP, Raad II (2002) The epidemiology of Candida glabrata and Candida albicans fungemia in immunocompromised patients with cancer. Am J Med 112:380–385
Chryssanthou E (2001) Trends in antifungal susceptibility among Swedish Candida species bloodstream isolates from 1994 to 1998: comparison of the E-test and the Sensititre YeastOne Colorimetric Antifungal Panel with the NCCLS M27-A reference method. J Clin Microbiol 39:4181–4183
Kovacicova G, Krupova Y, Lovaszova M, Roidova A, Trupl J, Liskova A, Hanzen J, Milosovic P, Lamosova M, Macekova L, Szovenyiova Z, Purgelova A, Obertik T, Bille J, Krcmery V (2000) Antifungal susceptibility of 262 bloodstream yeast isolates from a mixed cancer and non-cancer patient population: is there a correlation between in-vitro resistance to fluconazole and the outcome of fungemia? J Infect Chemother 6:216–221
Krcmery V, Barnes AJ (2002) Non-albicans Candida spp. causing fungaemia: pathogenicity and antifungal resistance. J Hosp Infect 50:243–260
Leung AY, Chim CS, Ho PL, Cheng VC, Yuen KY, Lie AK, Au WY, Liang R, Kwong YL (2002) Candida tropicalis fungaemia in adult patients with haematological malignancies: clinical features and risk factors. J Hosp Infect 50:316–319
Saiman L, Ludington E, Dawson JD, Patterson JE, Rangel-Frausto S, Wiblin RT, Blumberg HM, Pfaller M, Rinaldi M, Edwards JE, Wenzel RP, Jarvis W (2001) Risk factors for Candida species colonization of neonatal intensive care unit patients. Pediatr Infect Dis J 20:1119–1124
Trick WE, Fridkin SK, Edwards JR, Hajjeh RA, Gaynes RP (2002) Secular trend of hospital-acquired candidemia among intensive care unit patients in the United States during 1989–1999. Clin Infect Dis 35:627–630
Viscoli C, Girmenia C, Marinus A Viscoli C, Collette L, Martino P, Vandercam B, Doyen C, Lebeau B, Spence D, Krcmery V, De Pauw B, Meunier F (1999) Candidemia in cancer patients: a prospective, multicenter surveillance study by the Invasive Fungal Infection Group (IFIG) of the European Organization for Research and Treatment of Cancer (EORTC). Clin Infect Dis 28:1071–1079
Mora-Duarte J, Betts R, Rotstein C, Colombo AL, Thompson-Moya L, Smietana J, Lupinacci R, Sable C, Kartsonis N, Perfect J (2002) Comparison of caspofungin and amphotericin B for invasive candidiasis. New Engl J Med 347:2020–2029
Silva CL da, Santos RM dos, Colombo AL (2001) Cluster of Candida parapsilosis primary bloodstream infection in a neonatal intensive care unit. Braz J Infect Dis 5:32–36
Levy I, Rubin LG, Vasishtha S, Tucci V, Sood SK (1998) Emergence of Candida parapsilosis as the predominant species causing candidemia in children. Clin Infect Dis 26:1086–1088
Colombo AL, Nucci M, Salomao R, Branchini ML, Richtmann R, Derossi A, Wey SB (1999) High rate of non-albicans candidemia in Brazilian tertiary care hospitals. Diagn Microbiol Infect Dis 34:281–286
Lupetti A, Tavanti A, Davini P, Ghelardi E, Corsini V, Merusi I, Boldrini A, Campa M, Senesi S (2002) Horizontal transmission of Candida parapsilosis candidemia in a neonatal intensive care unit. J Clin Microbiol 40:2363–2369
Nucci M, Anaissie E (2002) Should vascular catheters be removed from all patients with candidemia? An evidence-based review. Clin Infect Dis 34:591–599
Sypula WT, Kale-Pradhan PB (2002) Therapeutic dilemma of fluconazole prophylaxis in intensive care. Ann Pharmacother 36:155–159
Marr KA (2000) The changing spectrum of candidemia in oncology patients: therapeutic implications. Curr Opin Infect Dis 13:615–620
Kataoka S, Kashiwa M, Saku K, Handa N, Akiyama H (1995) Candidemia in non-neutropenic patients with an intravenous hyperalimentation catheter: good prognosis of Candida parapsilosis infection. Kansenshogaku Zasshi 69:969–974
Collin B, Clancy CJ, Nguyen MH (1999) Antifungal resistance in non-albicans Candida species. Drug Resist Updat 2:9–14
Edwards JE Jr, Bodey GP, Bowden RA, Buchner T, Pauw BE de, Filler SG, Ghannoum MA, Glauser M, Herbrecht R, Kauffman CA, Kohno S, Martino P, Meunier F, Mori T, Pfaller MA, Rex JH, Rogers TR, Rubin RH, Solomkin J, Viscoli C, Walsh TJ, White M (1997) International conference for the development of a consensus on the management and prevention of severe candidal infections. Clin Infect Dis 25:43–59
Kam LW, Lin JD (2002) Management of systemic candidal infections in the intensive care unit. Am J Health Syst Pharm 59:33–41
Rogers TR (2001) Optimal use of existing and new antifungal drugs. Curr Opin Crit Care 7:238–241
Singh N (2001) Changing spectrum of invasive candidiasis and its therapeutic implications. Clin Microbiol Infect 7 (Suppl 2):1–7
Sable CA, Nguyen BY, Chodakewitz JA, DiNubile MJ (2002) Safety and tolerability of caspofungin acetate in the treatment of fungal infections. Transpl Infect Dis 4:25–30
Kuhn DM, George T, Chandra J, Mukherjee PK, Ghannoum MA (2002) Antifungal susceptibility of Candida biofilms: unique efficacy of amphotericin B lipid formulations and echinocandins. Antimicrob Agents Chemother 46:1773–1780
Hoffman HL, Rathbun RC (2002) Review of the safety and efficacy of voriconazole. Expert Opin Investig Drugs 11:409–429
Roilides E, Kadiltsoglou I, Zahides D, Bibashi E (1997) Invasive candidosis in pediatric patients. Clin Microbiol Infect 3:192–197
Groll AH, Walsh TJ (2001) Caspofungin: pharmacology, safety and therapeutic potential in superficial and invasive fungal infections. Expert Opin Investig Drugs 10:1545–1558
Marr KA (2002) Empirical antifungal therapy—new options, new tradeoffs. N Engl J Med 346:278–280
Acknowledgements
This study was funded by Merck Research Laboratories, West Point, PA, USA. The protocol was approved by Institutional Review Boards at each participating center and all patients gave written informed consent.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Colombo, A.L., Perfect, J., DiNubile, M. et al. Global Distribution and Outcomes for Candida Species Causing Invasive Candidiasis: Results from an International Randomized Double-Blind Study of Caspofungin Versus Amphotericin B for the Treatment of Invasive Candidiasis. Eur J Clin Microbiol Infect Dis 22, 470–474 (2003). https://doi.org/10.1007/s10096-003-0973-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10096-003-0973-8