Abstract
Introduction
As the most common cause of autosomal recessive early onset Parkinson’s disease (EOPD), parkin type Parkinson’s disease (PRKN-PD) may affect female patients in childbearing age. Accordingly, issues related to fertility must be adequately addressed. Here, we landscaped fertile life factors and pregnancy course of a PRKN-PD cohort, including both novel cases directly observed at our center and published ones.
Methods
Six patients with confirmed PRKN-PD were examined by a structured interview on reproductive factors and associated modifications of PD disturbances, including one case followed up throughout pregnancy which was described in greater detail. Six studies reporting fertile life factors of nine PRKN-PD patients were reviewed collecting homogeneous data on fertile life and pregnancy course.
Results
PRKN-PD female patients experienced motor fluctuations with the menstrual cycle, pregnancy, and puerperium, which suggests a role for sex hormones in PD clinical burden. In some cases, abortion and miscarriages occurred during the organogenesis phase in patients receiving oral antiparkinsonian therapy; however, levodopa/benserazide monotherapy resulted to be the safest choice in pregnancy.
Conclusion
Collectively these data disclose the importance of pre-conception counseling in childbearing age PRKN-PD patients and EOPD in general.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is a neurodegenerative disorder due to the loss of dopaminergic nigral cells and the brain accumulation of α-synuclein-positive Lewy bodies [1].
Although PD most commonly occurs in the elderly, in about 10% of cases, it affects subjects younger than fifty, presenting as “early-onset PD” (EOPD) [2,3,4,5].
PD impacts patients differently depending on their age at onset [2]. In particular, females with EOPD face peculiar challenges due to fertile life, including menstruation, pregnancy, and breastfeeding [6].
A genetic origin is almost frequent in EOPD [7]. Namely, bi-allelic mutations in the PRKN (Parkin) gene account for the most common autosomal recessive form of PD, representing about 15–20% of EOPD cases [8]. PRKN type PD (PRKN-PD) patients exhibit unique features compared to idiopathic EOPD patients, such as more prevalent dystonia at onset, sleep benefit, lower incidence of postural instability and falls, and better clinical course overall, including lower rate of cognitive impairment [9].
Because of the relative frequency of PRKN-PD among EOPD patients, issues related to fertile female life and pregnancy must be adequately and specifically addressed.
In this study, we examined fertile life factors and pregnancy courses in a cohort of PRKN-PD females, including six cases directly observed at our center and a group of previously described patients, to outline the PD course along the fertile life steps and identify helpful clues for clinical management.
Methods
Novel case series
Six confirmed PRKN-PD female patients from the Neurology Unit of the Tor Vergata University of Rome (Italy) were systematically assessed for fertile life history through a structured interview. One case followed up throughout pregnancy was described in greater detail. The questionnaire was structured into two parts: the first focused on general fertile life factors (age at menarche, regularity of menstruations, modification of symptoms during menstruations, number of pregnancies, type of births, number of abortions, age at menopause); the second, if applicable, focused on the pregnancy course after PD diagnosis (number of pregnancies, modification of symptoms and PD medications during pregnancies, type of births, number and type of abortions, information about breastfeeding). Informed consent was obtained from each participant. The study was conducted by the principles of the Helsinki Declarations and approved by the local ethical committee (protocol number 120/21).
Literature review
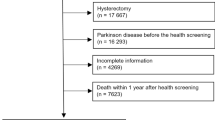
An in-depth literature search of the PubMed database using the Systematic Review Tool/Rayyan was performed to collect all patients with PRKN-PD previously described for fertile life factors [10]. The final reference list was generated after selecting all the manuscripts with key information regarding the selected topics: “Parkinson’s disease,” “PRKN,” “Parkin,” “PARK2” plus “pregnancy,” “menstruations,” “menstrual cycle,” “menses,” “breastfeeding.” A total of 192 articles were screened for relevant content (including duplicates). Of these, 22 were selected for further review. A final reference list of six articles, excluding duplicates, was finally included in this study, providing a description of fertile life factors and/or pregnancy courses in nine PRKN-PD patients [11,12,13,14,15,16]. As for the local cohort, we collected data on genetics, motor fluctuations during menstruation, pregnancy (including clinical course, therapies, and outcome of pregnancy), and breastfeeding.
Results
Novel case series
Case 1
A woman carrying a compound heterozygous mutation in the PRKN gene (exon 3 deletion in one allele and PRKN c1285 + 1G > A variant in the other allele) had been in our care since the age of 30 when she presented with asymmetrical bilateral lower limb dystonia, mild right upper limb bradykinesia, and rigidity, consistent with PD diagnosis (positive DAT-spect and ascertained levodopa 150 mg response). She was treated for a long time with pramipexole (0.52 mg/day), rasagiline (1 mg/day), and trihexyphenidyl (2 mg/day), reporting a full symptomatic control except for some motor and non-motor fluctuations (anxiety and depressed mood) during the menstrual cycle, with worsening a few days before menstruations and improvement afterward. After the patient expressed a desire for pregnancy at the age of 36, genetic counseling for the couple was performed. Because of the insufficient data on pregnancy safety, rasagiline, pramipexole, and trihexyphenidyl were discontinued, shifting to single therapy with levodopa/benserazide (300 mg/75 mg/day). The couple experienced difficulties conceiving due to gynecological troubles (a damaged tube) and the partner’s poor sperm motility. Accordingly, two cycles of medically assisted procreation (in vitro fertilization, IVF) were attempted, during which the patient did not report any modification in PD symptoms associated with exogenous hormonal treatment. At the age of 40, the patient had a first-trimester miscarriage due to an anembryonic pregnancy. Later, at the age of 41, she became pregnant again. This pregnancy had a normal course, and the levodopa/benserazide therapy was safely maintained at the same dosage (300 mg/75 mg/day). In the first trimester, the patient complained of fatigue and asthenia; then, both the motor disturbances and the general perception of well-being improved. At week 40 of gestation, the patient gave birth to a healthy baby girl through vaginal delivery. Immediately after delivery, the patient experienced a profound worsening of motor and non-motor symptoms. Breastfeeding was avoided to prevent drug passage, so safinamide was introduced (up to 100 mg/day) as an add-on, leading to stable clinical improvement. The baby, at the age of 6 months, was perfectly normally developing.
PRKN-PD local cohort
Table 1 summarizes the main fertile life and pregnancy features together with related PD issues of the six-PRKN-PD patient cohort observed at our center, including case 1 and the other five unpublished ones. The mean AAO was 35.2 ± 4.7 (30–40) years. Four patients (66.7%) reported worsening of both motor and non-motor disturbances a few days before menses. One of these noticed an amelioration of such menstrual cycle-related fluctuations after estrogen replacement therapy. Four patients got pregnant, for a total of ten pregnancies. Of these, seven resulted in live births (70%), two were electively terminated (20%), and one resulted in spontaneous abortion (case 1, 10%). Delivery was vaginal in four cases and by cesarean section (for reasons unrelated to PD) in three cases. Case 1, the only pregnant woman after the PD diagnosis and taking PD medications, reported motor fluctuations during pregnancy and worsening after delivery. Levodopa/benserazide treatment was kept unchanged during all the pregnancy course without complications. Of interest, case 2 experienced transient rigidity and pain in the left lower limb during both the first pregnancy (before PD diagnosis) and 2 years later (a few months after the second pregnancy), when she was diagnosed with PD. No cases of restless leg syndrome (RLS) were diagnosed. Case 1 avoided breastfeeding. Case 2 could not breastfeed for reasons unrelated to PD.
Literature review
Table 2 reports the main demographic and clinical features of patients. The onset of symptoms was defined in seven patients, with a mean AAO of 25.1 ± 9.9 (12–37) years. Three patients reported menstrual-related motor worsening, which improved in two cases with exogenous estrogenic treatment. Seven patients had a pregnancy history, for a total of 18 pregnancies. Seventeen pregnancies occurred after PD diagnosis, all in patients receiving oral antiparkinsonian therapy. Of those, 61.1% (n = 11) resulted in live births, 22.2% (n = 4) were electively terminated due to concerns about antiparkinsonian drugs, and 16.7% (n = 3) resulted in spontaneous abortion. The antiparkinsonian therapy was maintained during pregnancy in 15 cases, with 53.3% (n = 8) resulting in live births and the others resulting in spontaneous or voluntary abortion. Three patients became pregnant while on STN-DBS stimulation. Three of the seven pregnant patients (42.9%) complained of a worsening of their motor symptoms during pregnancy or soon after delivery; one patient (14.3%) ameliorated but had an early spontaneous abortion. No RLS cases were diagnosed. C-sections were performed in two patients because of the premature rupture of the membranes in a twin pregnancy in one case and because of the abnormal fetus position in the other. Two of the twelve newborns (16.7%) had a cardiac malformation. Three patients avoided breastfeeding, and two breastfed without taking any oral medication (one with STN-DBS). Lactation information was missing in the other cases.
Discussion
This study, combining data from both the local cohort and previously described cases, provided an unprecedented overview of issues related to fertile female life and pregnancy in PRKN-PD, a common form of EOPD.
First, we examined the impact of the menstrual cycle on the main PD disturbances and found that most PRKN-PD patients experienced a worsening of motor and non-motor symptoms immediately before menstruation [12], which is consistent with previous reports on idiopathic PD [17,18,19,20]. Of interest, the subjects by Sprenger et al. and one of our cases improved in menstruation-related fluctuations with the introduction of hormonal replacement therapy, suggesting that clinical deterioration before menses could result from the nadir of sex hormones [12]. However, other general factors due to the premenstrual global function and feeling of well-being might play a role [21].
Fertility issues are still poorly explored in PD female patients [22]. Our case 1 required medically assisted pregnancy because of the couple’s infertility due to gynecological factors (a damaged tube) rather than PD-related factors. The IVF was successful, as described in a previous case [23].
About 14% of the PRKN-PD patients’ pregnancies resulted in spontaneous abortion and about 20% in voluntary interruption. This abortion rate matches that of the general population (estimated to range from 10 to 24% [24]) but seems higher than that reported for idiopathic PD patients [17]. Two of the four miscarriages occurred in patients taking antiparkinsonian medications. As well, all cases of voluntary abortion were motivated by concerns about the teratogenic effects of PD medications. Finally, about 17% of the newborns, all exposed to antiparkinsonian medications during pregnancy, had a cardiac defect. Indeed, the effects of movement disorders medications on the fetus are largely unknown [25, 26]. Levodopa monotherapy has been reported as safe in pregnancy [24, 27], while data on dopamine agonists, MAO-B and COMT inhibitors, and anticholinergics are scarce [24]. Amantadine, instead, might have teratogenic effects [28]. Thus, pre-conception multidisciplinary counseling emerges as fundamental to providing education and maximizing pregnancy outcomes in all patients of childbearing age [29].
Eighteen pregnancies resulted in live births. Eleven pregnancies occurred after PD diagnosis, with nine patients taking oral medications. Five of eight patients (62.5%) who became pregnant after being diagnosed with PD reported fluctuations of motor features associated with pregnancy or puerperium, namely improvement during pregnancy in two cases (including our case 1), worsening during pregnancy in two cases, and worsening after delivery in two cases (including our case 1). Such fluctuations can be essentially related to hormonal changes, since estrogen and progesterone levels rise during pregnancy and dramatically drop with puerperium. While the neuroprotective and pro-dopaminergic effects of estradiol (E2) are well-known [30], the properties of estriol (E3), the dominant estrogen during pregnancy, and progesterone are not clear yet [17]. Apart from sex hormones, other factors, including altered pharmacokinetics, diet changes, and variations in intestinal absorption, as well as physical and psychosocial aspects, might also contribute to motor fluctuations during pregnancy [17]. The existing literature on pregnancy-related motor fluctuations is not univocal, although in most cases, a clinical worsening has been described either in pregnancy or in puerperium [17, 27], often due to medication reduction or withdrawal [3]. Indeed, the two patients who improved with pregnancy had been on the same oral medication since conceiving (levodopa monotherapy in one case, levodopa, pramipexole, and rasagiline in the other one). Patients who clinically deteriorated, on the other hand, had reduced or discontinued oral therapy, emphasizing the importance of the proper medication and dosage to ensure the patient’s well-being during such a critical phase.
It is interesting to notice that case 2 most likely experienced prodromal motor manifestations (as foot dystonia) during her first pregnancy and the puerperium of her second pregnancy, when an overt PD was recognized. Dystonia, indeed, may represent an onset sign of PD, especially in PRKN-PD [31, 32], although some cases of “dystonia gravidarum,” in which dystonia appears in pregnancy and rapidly resolves after delivery, have already been described [33, 34].
Of all live birth pregnancies reported, five resulted in a cesarean Sect. (5/18, 27.7%), reflecting the rates of C-sections of the general population (33.7% in Italy) [35] and, again, indicating no excess rates in this group population.
Breastfeeding was practiced only in two cases, both in the absence of oral medications. The benefits of breastfeeding either for the newborn or the mother are well established [36]; however, there is not sufficient evidence for antiparkinsonian agents’ safety in breastfeeding [28]. Levodopa, dopamine agonists, amantadine, and entacapone can indeed be detected in breast milk and may potentially affect the infant [28]. Nevertheless, some patients taking low doses of levodopa/carbidopa practiced breastfeeding without apparent harm on the infant [37].
Conclusion
The analysis of this small PRKN-PD cohort allowed us to highlight the impact of fertile female life on PD clinical course and, more in general, provide some insightful cues for the management of EOPD in women.
We reported how levodopa/benserazide monotherapy could assure a safe pregnancy (IVF-mediated) in PD without worsening of clinical impairment. Then, we noticed a rate of voluntary abortion and miscarriages during organogenesis in orally treated PRKN-PD patients, which raises the need for pre-conception counseling in young patients of childbearing age.
Finally, we observed that PRKN-PD presents with motor fluctuations concurring with the menstrual cycle, pregnancy, and puerperium, which definitely emphasizes the contribution of sex hormones in PD clinical burden, also paving the way for novel, potential therapeutic interventions [38].
Data availability
The datasets generated during analysis are available from the corresponding author upon reasonable request.
References
Poewe W, Seppi K, Tanner CM et al (2017) Parkinson disease. Nat Rev Dis Primers 3:1–21. https://doi.org/10.1038/nrdp.2017.13
Schrag A, Hovris A, Morley D et al (2003) Young- versus older-onset Parkinson’s disease: impact of disease and psychosocial consequences. Mov Disord. https://doi.org/10.1002/mds.10527
Mehanna R, Jankovic J (2019) Young-onset Parkinson’s disease: its unique features and their impact on quality of life. Parkinsonism Relat Disord. https://doi.org/10.1016/j.parkreldis.2019.06.001
Schirinzi T, Di Lazzaro G, Sancesario GM et al (2020) Young-onset and late-onset Parkinson’s disease exhibit a different profile of fluid biomarkers and clinical features. Neurobiol Aging. https://doi.org/10.1016/j.neurobiolaging.2020.02.012
Bovenzi R, Conti M, Degoli GR et al (2023) Shaping the course of early-onset Parkinson’s disease: insights from a longitudinal cohort. Neurol Sci. https://doi.org/10.1007/s10072-023-06826-5
Calne SM, Kumar A (2008) Young onset Parkinson’s disease. Practical management of medical issues. Parkinsonism Relat Disord. https://doi.org/10.1016/j.parkreldis.2007.07.007
Payami H, Zareparsi S, James D, Nutt J (2002) Familial aggregation of Parkinson disease: a comparative study of early-onset and late-onset disease. Arch Neurol. https://doi.org/10.1001/archneur.59.5.848
Lücking CB, Dürr A, Bonifati V, et al (2000) Association between early-onset Parkinson’s disease and mutations in the parkin gene. N Engl J Med 342:. https://doi.org/10.1056/nejm200005253422103
Marsili L, Vizcarra JA, Sturchio A et al (2021) When does postural instability appear in monogenic parkinsonisms? An individual-patient meta-analysis. J Neurol 268:3211
Johnson N, Phillips M (2018) Rayyan for systematic reviews. J Electron Resour Librariansh. https://doi.org/10.1080/1941126X.2018.1444339
Serikawa T, Shimohata T, Akashi M, et al (2011) Successful twin pregnancy in a patient with parkin-associated autosomal recessive juvenile parkinsonism. BMC Neurol 11:. https://doi.org/10.1186/1471-2377-11-72
Sprenger FS, Seppi K, Wolf E, Poewe W (2014) Perimenstrual fluctuations in two siblings with early-onset Parkinson’s disease. Mov Disord Clin Pract. https://doi.org/10.1002/mdc3.12036
Scelzo E, Mehrkens JH, Bötzel K, et al (2015) Deep brain stimulation during pregnancy and delivery: experience from a series of “DBS babies.” Front Neurol 6:. https://doi.org/10.3389/fneur.2015.00191
Sazci A, Idrisoglu HA (2019) Pregnancy in Parkinson’s disease with PARK2 mutations. Clin Park Relat Disord. https://doi.org/10.1016/j.prdoa.2019.08.003
Lim SY, Ahmad-Annuar A, Lohmann K, et al (2021) Clinical phenotype of Parkinson’s disease with a homozygous PRKN p.Cys441Arg mutation. Neurol Asia 26(1):161 – 166
Yoshii F, Aono K, Kumazawa R, Takahashi W (2021) PARK2 patient presenting with dopa-responsive dystonia. Case Rep Neurol 13:. https://doi.org/10.1159/000520436
Seier M, Hiller A (2017) Parkinson’s disease and pregnancy: an updated review. Parkinsonism Relat Disord. https://doi.org/10.1016/j.parkreldis.2017.05.007
Quinn NP, Marsden CD (1986) Menstrual-related fluctuations in Parkinson’s disease. Mov Disord. https://doi.org/10.1002/mds.870010112
Factor SA (1993) Acetazolamide therapy of menstrual-related fluctuations in Parkinson’s disease. Mov Disord. https://doi.org/10.1002/mds.870080231
Castrioto A, Hulliger S, Poon YY et al (2010) A survey on the impact of the menstrual cycle on movement disorders severity. Can J Neurol Sci. https://doi.org/10.1017/S0317167100010490
Kompoliti K, Comella CL, Jaglin JA et al (2000) Menstrual-related changes in motoric function in women with Parkinson’s disease. Neurology. https://doi.org/10.1212/wnl.55.10.1572
Rubin SM (2007) Parkinson’s disease in women. Dis Mon. https://doi.org/10.1016/j.disamonth.2007.02.002
Baxi A, Neema H, Pauranik A (2010) Successful birth of an IVF baby in a patient with Parkinson’s disease. J Hum Reprod Sci. https://doi.org/10.4103/0974-1208.63123
Young C, Phillips R, Ebenezer L, et al (2020) Management of Parkinson’s disease during pregnancy: literature review and multidisciplinary input. Mov Disord Clin Pract 7:. https://doi.org/10.1002/mdc3.12925
Bovenzi R, Schirinzi T, Pierantozzi M, et al (2020) Clinical course of paroxysmal dyskinesias throughout pregnancy. Parkinsonism Relat Disord. https://doi.org/10.1016/j.parkreldis.2020.09.017
Bovenzi R, Conti M, Schirinzi T (2023) Pharmacotherapy for Sydenham’s chorea: where are we and where do we need to be? Expert Opin Pharmacother 1–13. https://doi.org/10.1080/14656566.2023.2216380
Olivola S, Xodo S, Olivola E et al (2020) Parkinson’s disease in pregnancy: a case report and review of the literature. Front Neurol. https://doi.org/10.3389/fneur.2019.01349
García-Ramos R, Santos-García D, Alonso-Cánovas A, et al (2021) Management of Parkinson’s disease and other movement disorders in woman of childbearing age: part 1. Neurologia 36:. https://doi.org/10.1016/j.nrl.2020.05.010
(2019) Prepregnancy counseling: Committee Opinion No. 762. Fertil Steril 111:. https://doi.org/10.1016/j.fertnstert.2018.12.003
Bovenzi R, Sancesario GM, Conti M et al (2023) Sex hormones differentially contribute to Parkinson’s disease in males: a multimodal biomarker study. Eur J Neurol. https://doi.org/10.1111/ene.15801
Arevalo GG, Jorge R, Garcia S et al (1997) Clinical and pharmacological differences in early- versus late-onset Parkinson’s disease. Mov Disord. https://doi.org/10.1002/mds.870120303
Wickremaratchi MM, Ben-Shlomo Y, Morris HR (2009) The effect of onset age on the clinical features of Parkinson’s disease. Eur J Neurol. https://doi.org/10.1111/j.1468-1331.2008.02514.x
Fasano A, Elia AE, Guidubaldi A et al (2007) Dystonia gravidarum: a new case with a long follow-up. Mov Disord. https://doi.org/10.1002/mds.21310
Lim ECH, Seet RCS, Wilder-Smith E, Ong BKC (2006) Dystonia gravidarum: a new entity? Mov Disord. https://doi.org/10.1002/mds.20648
Masciullo L, Petruzziello L, Perrone G, et al (2020) Caesarean section on maternal request: an Italian comparative study on patients’ characteristics, pregnancy outcomes and guidelines overview. Int J Environ Res Public Health 17:. https://doi.org/10.3390/ijerph17134665
Eidelman AI, Schanler RJ (2012) Breastfeeding and the use of human milk. Pediatrics. https://doi.org/10.1542/peds.2004-2491
Bethesda (MD): National Institute of Child Health and Human Development (2006) Drugs and Lactation Database (LactMed®) [Internet]. Levodopa. Available from: https://www.ncbi.nlm.nih.gov/books/NBK501337/
Rodríguez-Navarro JA, Solano RM, Casarejos MJ et al (2008) Gender differences and estrogen effects in parkin null mice. J Neurochem. https://doi.org/10.1111/j.1471-4159.2008.05569.x
Funding
Open access funding provided by Università degli Studi di Roma Tor Vergata within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Roberta Bovenzi, Giulia Rebecca Degoli, Matteo Conti, Rocco Cerroni, and Carlo Alberto Artusi. The first draft of the manuscript was written by Roberta Bovenzi and all authors commented on previous versions of the manuscript. Alessandro Stefani, Mariangela Pierantozzi, Nicola Biagio Mercuri, and Tommaso Schirinzi supervised the study and provided a critical revision of the content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
The study was conducted in line with the ethical principles of the Declarations of Helsinki and approved by the local ethical committee (protocol number 120/21).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bovenzi, R., Conti, M., Degoli, G.R. et al. Pregnancy, fertile life factors, and associated clinical course in PRKN early-onset Parkinson’s disease. Neurol Sci 45, 591–599 (2024). https://doi.org/10.1007/s10072-023-07029-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-023-07029-8