Abstract
Aim
To combine the current scientific literature evidence and elucidate the differences of lead (Pb) bioaccumulation in human tissues by comparing amyotrophic lateral sclerosis (ALS) patients and healthy controls.
Methods
We systematically searched for case–control studies on the association of Pb levels with ALS, in human cells, tissues, and body fluids (nervous tissue, muscle, blood, cerebrospinal fluid, urine, skin appendages). Then, we performed a meta-analysis for all the tissues in which at least five case–control studies were available: whole blood (9 studies), serum/plasma (5 studies), and cerebrospinal fluid (CSF) (6 studies). Differences between cases and controls were evaluated using standardized mean difference, and combined estimates were derived using random effect maximum likelihood (REML) meta-analyses.
Results
Among 1734 records, we identified 46 full-text studies, of which 14 case–control studies met the meta-analysis inclusion criteria. We found higher Pb levels in ALS cases than controls in blood (standardized mean difference (SMD) = 0.61; 95% confidence interval (CI) 0.20, 1.01; p = 0.003), plasma/serum (SMD = 0.27; 95% CI − 0.16, 0.70; p = 0.26), and CSF (SMD = 0.53; 95% CI − 0.09, 1.15; p = 0.09).
Conclusions
This work provides further evidence of the association between Pb bioaccumulation and ALS in body fluids. The lack of association studies in solid tissues did not allow a robust meta-analysis. Future prospective studies are needed to clarify the causality in the association of Pb bioaccumulation with ALS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Amyotrophic lateral sclerosis (ALS) is an incidence-increasing neurodegenerative disease in adulthood with no cure, which affects the whole compartment of cortical, bulbar, and spinal motor neurons, causing the irreversible collapse of the nervous system control of the voluntary muscle activity, muscular atrophy, and death [1, 2]. The onset and progression of ALS rely on a multifactorial etiology which includes multiple genetic and environmental factors and their mutual interactions, and both act either in familiar (fALS) or sporadic (sALS) forms of the pathology, albeit with different molecular mechanisms and patterns [3, 4].
Clinically, fALS and sALS patients undergo similar diagnostic procedures (i.e., El Escorial criteria) and pharmacological treatments. However, treatments cannot stop the disease progression, but they can only delay the worsening of the disease. On the other hand, the patients’ age of onset and diagnosis seems to be globally decreasing, with a difference of 5–10-year anticipation in fALS cases in relation to sALS patients, probably attributable to the effect of Mendelian ALS-related gene variants more frequent in fALS rather than in sALS, and not merely to ascertainment bias such the increasingly early diagnosis in healthy individuals with relatives affected by ALS [5]. Hence, the genetic burden plays a key role in fALS patients, accounting for 5–10% of the ALS population. Conversely, most ALS patients (90–95%) suffer from the sporadic form of disease dependent on unknown genetic variants and environmental factors, whose exact etiology and underlying pathogenic cellular and molecular mechanism are still to solve [4].
Along with the environmental factors responsible for sALS, chemicals, toxins (i.e., β-methylamino-L-alanine), viruses, and others have been counted [6], diminishing the environmental risk may lead to a decrease in ALS incidence and progression. These and other factors may influence ALS physiopathology, including sex, age, spinal vs bulbar onset, and tissue concentrations of persistent pollutants. Therefore, they are interpretable as risk factors and survival predictors [3]. Metals, particularly heavy metals, are persistent environmental factors supposed to be primarily involved in the etiology and pathogenic mechanism of sALS, but they also seem to play a role in fALS disease. Notably, heavy metal biomagnification in exposed living species and their food chains leads to high bioaccumulation in organisms, including humans, with health concerns for the most susceptible individuals. Most ALS associations have been found for lead (Pb), a lipophilic metal with no function in the human body which accumulates in tissues and organs following chronic and/or acute exposure, including the nervous system, due to its recognized high ability to cross the blood–brain barrier [7,8,9].
Recently, we critically reviewed the ALS–Pb relationship through a systematic review of the scientific literature of the last decade (2011–2020), giving a complete picture of the most recent epidemiological, clinical, and experimental evidence of the pathogenic role of Pb in ALS, reporting also a potential ALS pathogenic mechanism of Pb involving TAR DNA-binding protein misfolding and accumulation [10]. In that work, we retrieved and included only research articles in the manuscript, without referencing reviews, meta-analyses, and other types of manuscripts, categorized separately. From the last task, we noticed a lack of specific meta-analyses considering the Pb bioaccumulation and quantification in human matrices of ALS patients and healthy controls. Most meta-analyses combined Pb levels in human samples, mainly blood, with other indirect Pb–exposure parameters, such as personal questionnaires, environmental and occupational Pb levels, and others. However, the human metal biomonitoring through direct measurement of the effective Pb concentration in human biological tissues still represents the most powerful procedure to evaluate the current Pb exposure and body absorption. This is particularly relevant when there are discrepancies in Pb bioaccumulation, attributable to a different Pb genetic susceptibility among individuals living in a similar environment. Moreover, our recent systematic update (2011–2020) lacks meta-analyses since it did not include the scientific literature before 2011. For all these reasons, a critical revision of the clinical information on ALS derived from gold standard quantitative analysis of Pb bioaccumulation in human tissues is needed. Here, we critically performed a systematic review of case–control studies published at any time evaluating the Pb levels in any human matrix, such as isolated cells, solid tissues, and body fluids derived from ALS patients and healthy donors. We performed three different meta-analyses of Pb levels in ALS case–control studies considering eligible studies: on whole blood, serum/plasma, and cerebrospinal fluid (CSF), using a restricted maximum likelihood estimation of the random effects (REML) model in a frequentist framework.
Methods
Systematic review method
The research was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [11]. Preliminarily, four authors independently collected published studies on human ALS–Pb relationship, up to February 2022, in PubMed and Scopus databases. The search profile consisted of “lead AND amyotrophic AND lateral AND sclerosis” with 1405 preliminary results on PubMed and 3144 preliminary results on Scopus; and “metals AND amyotrophic AND lateral AND sclerosis” with 1329 preliminary results on PubMed and 764 preliminary results on Scopus.
The reference list of the main reviews on heavy metals and trace elements in ALS patients was also examined to identify additional papers that had been missed. This last task confirmed the lack of specific meta-analysis considering the presence of Pb in human tissues, which is the main aim of this work. Duplicate studies among databases were removed to obtain the first set of papers that focused on Pb and ALS. For search profiles, all titles of the first set of papers were examined and abstracts read of those may be being relevant.
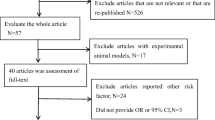
Eligible criteria were case–control studies with results on Pb levels, given as mean ± SD or median and interquartile range, measured in any type of tissue of patients with ALS and healthy donors (controls). The eligibility and final inclusion of each manuscript were assessed independently by two groups of authors, and disagreements were deeply discussed between groups to reach a common conclusion. Meta-analysis of selected tissues was performed as described in following paragraph (“Meta-analysis statistical method” section) if the number of studies for each tissue was ≥ 5. An overview of the selection process is depicted by the PRISMA flow diagram in Fig. 1.
Meta-analysis statistical method
Combined standardized mean differences between ALS cases and healthy controls and 95% CIs were calculated through a REML meta-analysis to avoid possible heterogeneity between studies [12]. Since, in some studies, the authors summarized the data by reporting the sample medians and one or both of (i) the minimum and maximum values and (ii) the first and third quartiles, without reporting the means or standard deviations, we have estimated means and standard deviations for ALS cases and healthy controls from medians and quartile values according to Weir and colleagues [13]. All the analyses were performed using the R software for statistical analyses, and the meta-analyses were performed using the R package metafor [14].
Results
After an in-depth systematic review of the literature, a total of nine studies with Pb measured in whole blood [15,16,17,18,19,20,21,22,23], five studies with Pb measured in plasma [18, 24, 25] or serum [15, 26], and six studies with Pb measured in CSF [18, 24, 26,27,28,29] met the inclusion criteria and were considered eligible for meta-analysis. Hence, we were able to perform a robust meta-analysis of Pb levels on a total of 409 ALS cases and 575 controls for whole blood, 64 ALS cases and 67 controls for plasma/serum, and 114 ALS cases and 130 controls for CSF. Other studies met the inclusion criteria for other tissues: bone (tibia and patella), urine, skeletal muscle, and nails. However, due to the low number of studies representative of these specific tissues, they were considered eligible for the systematic review but not included in the meta-analysis.
Blood Pb in ALS patients and healthy donors
Whole blood
The results of the meta-analysis on whole blood Pb are described in Fig. 2 via forest plot. We found significantly higher levels of Pb in the blood of ALS cases compared to controls. The average standardized difference was 0.61, with a 95% CI of [0.20, 1.01] and p value = 0.003.
Forest plot: meta-analysis of nine studies on blood samples. Each study is represented with a square centered at the point estimate of the standardized mean difference, with a horizontal line (whiskers) extending on either side of the square, representing the 95% confidence interval of the point estimate. The area of the square is proportional to the corresponding study weight. Combined estimate and 95% confidence interval is represented with a black diamond
We did not find evidence of heterogeneity in the effect among studies considering the Cochran’s Q (Q = 73.21, df = 8, p < 0.0001) and the I2 statistics (I2 = 84.4%) (Fig. 2).
Plasma and serum
Eligible studies on plasma and serum Pb levels were combined for meta-analysis after data standardization to obtain a combined estimate for the two matrices, referred here as plasma/serum. The results of the meta-analysis on plasma/serum are described in Fig. 3 via forest plot. We found higher levels of Pb in ALS cases, although the standardized mean difference was not statistically significant. The estimate standardized mean difference was 0.27 with a 95% CI of [− 0.16, 0.70] and p value = 0.21. Also, we found some evidence of study heterogeneity looking at the Cochran’s Q (Q = 5.33, df = 4, p = 0.26) and I2 statistics (I2 = 28.9%) (Fig. 3).
Forest plot: meta-analysis of five studies on plasma/serum samples. Each study is represented with a square centered at the point estimate of the standardized mean difference, with a horizontal line (whiskers) extending on either side of the square, representing the 95% confidence interval of the point estimate. The area of the square is proportional to the corresponding study weight. Combined estimate and 95% confidence interval is represented with a black diamond
Cerebrospinal fluid Pb in ALS patients and controls
The results of the meta-analysis on CSF Pb levels are described in Fig. 4 via forest plot. We found higher values of Pb in ALS cases compared to controls, although the standardized mean difference was borderline statistically significant. The estimate was 0.53 with a 95% CI of [− 0.09, 1.15] and p value = 0.09. No evidence of effect heterogeneity was found looking at the Cochran’s Q (Q = 18.5, df = 5, p < 0.0001) and the I2 statistics (I2 = 80.8%) (Fig. 4).
Forest plot: meta-analysis of six studies on CSF samples. Each study is represented with a square centered at the point estimate of the standardized mean difference, with a horizontal line (whiskers) extending on either side of the square, representing the 95% confidence interval of the point estimate. The area of the square is proportional to the corresponding study weight. Combined estimate and 95% confidence interval is represented with a black diamond
Publication bias and sensitivity analyses
We have investigated possible publication bias by the analysis of the funnel plot, Galbraith radial plot, and normal quantile–quantile (Q-Q) plot (Fig. 5).
The visual inspection of the funnel plots highlights some degree of asymmetric distribution around the central estimates for the analyses in blood and CSF indicating possible source of publication bias. Specifically, one study estimate in blood and one study estimate in CSF fall on the right side of the “funnel triangles” indicating overestimation of the differences between cases and controls. However, no evidence of publication bias can be observed looking at radial and Q-Q plots.
To avoid any doubt about the robustness of our results in blood, we run a leave-one-out sensitivity analysis, confirming the significant association in blood (Table 1).
Discussion
Amyotrophic lateral sclerosis is a neurodegenerative disease that affects motor neurons. Although it can be defined a rare disease, it leads to a significantly lower quality of life of patients and their families, causing progressive overtime immobility that requires total assistance, resolving with the death of the patients in a period that goes from about 24 to 50 months from diagnosis [30].
Despite the huge attention of research on this topic, much of its etiology is not yet known, suggesting that both environmental and genetic factors contribute to its onset and severity [3, 4]. Among the environmental factors, heavy metals have attracted the attention of researchers, in particular Pb, because of its demonstrated neurotoxicity [31,32,33,34].
Due to the reasons mentioned above, this meta-analysis work aims to clarify the association of Pb levels in human tissues with the onset of ALS, a link still not clarified despite the numerous publications on the subject. We conducted a systematic research of the works published until February 2022. The works that met our research criteria were fourteen case–control studies for concentrations of Pb in whole blood, plasma/serum, and CSF. Of these works, nine took whole blood samples, five plasma/serum, and six CSF (some are considering more than a tissue).
For all tissues analyzed, we observed a positive trend that shows an association between the concentrations of Pb and the presence of the disease. However, the only tissue that gave a statistically significant result was whole blood (SMD = 0.61; 95% CI 0.20, 1.01; p = 0.003).
Although the combined standardized difference between cases and controls was positive (higher in ALS cases) for all three tissues, we observed in serum/plasma two publications in which Pb concentration was lower in ALS cases than controls. The two articles [18, 24] reported the value as a median rather than as a mean and this made necessary their transformation into average values, in order to make them homogeneous and comparable with other articles. This conversion may have played a role in the presence of these anomalous data, in fact in the paper of Roos et al. [24] values which were expressed as a median showed higher values in ALS patients than the controls; however, in both values the difference is really low and without statistical significance.
We obtained significant association in whole blood only. This result can be explained by the small number of studies and patients in other matrices, highlighting the importance of further studies in the field. However, it is crucial to consider the distribution of this metal, showing a particular propensity for cellular structures, within which it tends to accumulate. In particular, Pb tends to accumulate inside the erythrocytes rather than into the plasma component [35,36,37]. One of the most targeted components in the erythrocytes is the d-aminolevulinic acid dehydratase (ALAD), an enzyme fundamental for the synthesis of heme groups [8, 36]. Another target is the pyrimidine 5′-nucleotidase 1, involved in the pyrimidine metabolism [38]. This could explain why the most consistent results were observed in whole blood compared to plasma/serum, indicating the former as a preferable matrix for this type of analysis. The same considerations apply to the CSF. In fact, this is also an acellular matrix, and several works show how the Pb tends to accumulate within the choroid plexus or to be seized by the glia, specifically in astrocytes, explaining why its concentrations in the CSF may be too low to allow discrimination between patients and controls. On the other hand, it must be considered that at the bone level, one of the main tissues of accumulation of Pb [39, 40], the latter tends to accumulate at the level of the extracellular matrix, thanks to its ability to replace the divalent ions, such as the Ca2+, important component for the formation of the bone matrix [41]. The bone tissue represents one of the longest-lived reserves of Pb in the human body, capable of mobilizing such reserves, for example, following periods of prolonged immobility. Such consideration is very important and in the interpretation of the results presented here, since, as described in Vinceti et al., the differences between ALS patients and controls could be linked to the long period of immobilization of patients and the consequent bone resorption followed by the mobilization of Pb reserves. This may introduce a bias in the analyses making the causal link between the blood concentrations of this metal and the onset of the disease difficult to interpret [19, 27].
In support of the eligibility of Pb as an etiological factor in ALS is its marked neurotoxic cytotoxicity, also on a charge of the motor neurons, it has been observed that chronic exposure to this metal is accompanied by gradual atrophy of skeletal muscles [24, 33]. Furthermore, it has been observed that at the origin of the neuropathy following the intoxication by Pb, finds its origin at the level of the anterior horn of the spinal cord [24]. Pb is able to overcome the blood–brain barrier, and its accumulation in choroidal plexuses can cause their alteration resulting in damage to these structures and to the brain, with consequent accumulation in the glia and neurons [7,8,9]. In addition, changes in the blood–brain membrane are detected in almost 50% of ALS patients [42,43,44]. At the intracellular level, the mechanisms of action of Pb are known, it exerts its cytotoxicity by altering the homeostasis of the essential elements of the organism and mimes divalent ions such as zinc (Zn2+) and Ca2+, also binds thiolate proteins (-SH), and as previously seen alters the production of heme groups and induces oxidative stress, also altering systems of protection against this phenomenon [45, 46]. From a molecular point of view, a recent study conducted in mice highlights the ability of Pb to induce the formation of aggregates and the inclusion of TAR DNA-binding protein (TDP-43), one of the main phenomena that occur in motor neurons during the ALS [47], data that although preliminary offer a possible scenario on the etiopathogenesis of Pb at the molecular level. In addition, Pb can alter neuronal transmission by acting on NMDR receptors, acetylcholine receptors, and voltage-dependent calcium channels [37].
Although the present work does not allow to assert a certain correlation between Pb levels in the body and ALS, it positively supports this hypothesis, showing a synergistic enhancement of the literature supporting this thesis and highlighting the usability of Pb levels in whole blood as a biomarker, probably in combination with other factors. Although further studies are necessary in order to increase the statistical power and to better clarify the possible cellular mechanisms underlying the possible role of Pb in the occurrence of ALS, this paper provide a further evidence favoring this hypothesis. Furthermore, as previously discussed, it is not clear if the accumulation of Pb in blood and other biological tissues is the cause or the consequence of the disease making it necessary to clarify this point. Additional epidemiological prospective studies are needed to reduce the risk of misinterpretation due to reverse causation. Besides, the recently developed Mendelian randomization (MR) approach can provide further evidence about causality in this association, as it has recently done to clarify the association of ALS with other traits [48]. As recently pointed out in the review by Julian et al., high-quality genome-wide association studies (GWAS) on lead levels and ALS risk are needed to identify robust instrumental variables for this purpose and avoid incorrect result interpretations [48].
References
Hardiman O, Al-Chalabi A, Chio A et al (2017) Amyotrophic lateral sclerosis. Nat Rev Dis Primers 3:1–18. https://doi.org/10.1038/nrdp.2017.71
Logroscino G, Piccininni M (2019) Amyotrophic lateral sclerosis descriptive epidemiology: the origin of geographic difference. Neuroepidemiology 52(1–2):3–103. https://doi.org/10.1159/000493386
Westeneng HJ, Debray TPA, Visser AE et al (2018) Prognosis for patients with amyotrophic lateral sclerosis: development and validation of a personalised prediction model. Lancet Neurol 17:423–433. https://doi.org/10.1016/S1474-4422(18)30089-9
Volk AE, Weishaupt JH, Andersen PM et al (2018) Current knowledge and recent insights into the genetic basis of amyotrophic lateral sclerosis. Medizinische Genetik 30:252–258. https://doi.org/10.1007/s11825-018-0185-3
Mehta PR, Jones AR, Opie-Martin S et al (2019) Younger age of onset in familial amyotrophic lateral sclerosis is a result of pathogenic gene variants, rather than ascertainment bias. J Neurol Neurosurg Psychiatry 90:268–271. https://doi.org/10.1136/jnnp-2018-319089
Ingre C, Roos PM, Piehl F et al (2015) Risk factors for amyotrophic lateral sclerosis. Clin Epidemiol 7:181–193. https://doi.org/10.2147/CLEP.S37505
Zheng W (2001) Neurotoxicology of the brain barrier system: new implications. J Toxicol-Clin Toxicol 39:711–719. https://doi.org/10.1081/CLT-100108512
Sanders T, Liu Y, Buchner V, Tchounwou PB (2009) Neurotoxic effects and biomarkers of lead exposure: a review. Rev Environ Health 24:15–45. https://doi.org/10.1515/REVEH.2009.24.1.15
Zheng W (2001) Toxicology of choroid plexus: special reference to metal-induced neurotoxicities. Microsc Res Tech 52:89–103. https://doi.org/10.1002/1097-0029(20010101)52:1<89::AID-JEMT11>3.0.CO;2-2
Farace C, Fenu G, Lintas S et al (2020) Amyotrophic lateral sclerosis and lead: a systematic update. NeuroToxicology 81:80–88. https://doi.org/10.1016/j.neuro.2020.09.003
Moher D, Liberati A, Tetzlaff J et al (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. https://doi.org/10.1371/journal.pmed.1000097
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR (2010) A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods 1:97–111. https://doi.org/10.1002/jrsm.12
Weir CJ, Butcher I, Assi V et al (2018) Dealing with missing standard deviation and mean values in meta-analysis of continuous outcomes: a systematic review. BMC Med Res Methodol 18:1–14. https://doi.org/10.1186/s12874-018-0483-0
Viechtbauer W (2010) Conducting meta-analyses in R with the metafor package. J Stat Softw 36:1–48. https://doi.org/10.18637/jss.v036.i03
De Benedetti S, Lucchini G, Del Bò C et al (2017) Blood trace metals in a sporadic amyotrophic lateral sclerosis geographical cluster. BioMetals 30:355–365. https://doi.org/10.1007/s10534-017-0011-4
Fang F, Kwee LC, Allen KD et al (2010) Association between blood lead and the risk of amyotrophic lateral sclerosis. Am J Epidemiol 171:1126–1133. https://doi.org/10.1093/aje/kwq063
Sienko DG, Davis JP, Taylor JA, Brooks BR (1990) Amyotrophic lateral sclerosis: a case-control study following detection of a cluster in a small wisconsin community. Arch Neurol 47:38–41. https://doi.org/10.1001/archneur.1990.00530010046017
Stober T, Stelte W, Kunze K (1983) Lead concentrations in blood, plasma, erythrocytes, and cerebrospinal fluid in amyotrophic lateral sclerosis. J Neurol Sci 61:21–26. https://doi.org/10.1016/0022-510X(83)90051-5
Vinceti M, Guidetti D, Bergomi M et al (1997) Lead, cadmium, and selenium in the blood of patients with sporadic amyotrophic lateral sclerosis. Ital J Neurol Sci 18:87–92. https://doi.org/10.1007/BF01999568
Garzillo EM, Lamberti M, Genovese G et al (2014) Blood lead, manganese, and aluminum levels in a regional Italian cohort of ALS patients does aluminum have an influence? J Occup Environ Med 56:1062–1066. https://doi.org/10.1097/JOM.0000000000000266
Oggiano R, Solinas G, Forte G et al (2018) Trace elements in ALS patients and their relationships with clinical severity. Chemosphere 197:457–466. https://doi.org/10.1016/j.chemosphere.2018.01.076
Qin X, Wu P, Wen T et al (2022) Comparative assessment of blood metal/metalloid levels, clinical heterogeneity, and disease severity in amyotrophic lateral sclerosis patients. Neurotoxicology 89:12–19. https://doi.org/10.1016/j.neuro.2022.01.003
Eum KD, Seals RM, Taylor KM et al (2015) Modification of the association between lead exposure and amyotrophic lateral sclerosis by iron and oxidative stress related gene polymorphisms. Amyotroph Lateral Scler Frontotemporal Degener 16:72–79. https://doi.org/10.3109/21678421.2014.964259
Roos PM, Vesterberg O, Syversen T et al (2013) Metal concentrations in cerebrospinal fluid and blood plasma from patients with amyotrophic lateral sclerosis. Biol Trace Elem Res 151:159–170. https://doi.org/10.1007/s12011-012-9547-x
Conradi S, Ronnevi LO, Vesterberg O (1978) Increased plasma levels of lead in patients with amyotrophic lateral sclerosis compared with control subjects as determined by flameless atomic absorption spectrophotometry. J Neurol Neurosurg Psychiatry 41:389–393. https://doi.org/10.1136/jnnp.41.5.389
Kapaki E, Segditsa J, Zournas C et al (1989) Determination of cerebrospinal fluid and serum lead levels in patients with amyotrophic lateral sclerosis and other neurological diseases. Experientia 45:1108–1110. https://doi.org/10.1007/BF01950171
Vinceti M, Filippini T, Mandrioli J et al (2017) Lead, cadmium and mercury in cerebrospinal fluid and risk of amyotrophic lateral sclerosis: a case-control study. J Trace Elem Med Biol 43:121–125. https://doi.org/10.1016/j.jtemb.2016.12.012
Cavalleri A, Minoia C, Ceroni M, Poloni M (1984) Lead in cerebrospinal fluid and its relationship to plasma lead in humans. J Appl Toxicol 4:63–65. https://doi.org/10.1002/jat.2550040202
Conradi S, Ronnevi LO, Nise G, Vesterberg O (1980) Abnormal distribution of lead in amyotrophic lateral sclerosis. Reestimation of lead in the cerebrospinal fluid. J Neurol Sci 48:413–418. https://doi.org/10.1016/0022-510X(80)90112-4
Radunovic A, Annane D, Rafiq MK et al (2017) Mechanical ventilation for amyotrophic lateral sclerosis/motor neuron disease. Cochrane Database Syst Rev 2017:CD004427. https://doi.org/10.1002/14651858.CD004427.pub4
Goel AD, Chowgule RV (2019) Outbreak investigation of lead neurotoxicity in children from artificial jewelry cottage industry. Environ Health Prev Med 24:1–5. https://doi.org/10.1186/s12199-019-0777-9
Rocha A, Trujillo KA (2019) Neurotoxicity of low-level lead exposure: history, mechanisms of action, and behavioral effects in humans and preclinical models. NeuroToxicology 73:58–80. https://doi.org/10.1016/j.neuro.2019.02.021
Mazliah J, Barron S, Bental E et al (1989) The effects of long-term lead intoxication on the nervous system of the chicken. Neurosci Lett 101:253–257. https://doi.org/10.1016/0304-3940(89)90541-7
Liu KS, Hao JH, Zeng Y et al (2013) Neurotoxicity and biomarkers of lead exposure: a review. Chin Med Sci J 28:178–188. https://doi.org/10.1016/S1001-9294(13)60045-0
Schütz A, Bergdahl IA, Ekholm A, Skerfving S (1996) Measurement by ICP-MS of lead in plasma and whole blood of lead workers and controls. Occup Environ Med 53:736–740. https://doi.org/10.1136/oem.53.11.736
Bergdahl IA, Grubb A, Schütz A et al (1997) Lead binding to δ-aminolevulinic acid dehydratase (ALAD) in human erythrocytes. Pharmacol Toxicol 81:153–158. https://doi.org/10.1111/j.1600-0773.1997.tb02061.x
de Souza ID, de Andrade AS, Dalmolin RJS (2018) Lead-interacting proteins and their implication in lead poisoning. Crit Rev Toxicol 48:375–386. https://doi.org/10.1080/10408444.2018.1429387
Paglia DE, Valentine WN, Dahlgren JG (1975) Effects of low level lead exposure on pyrimidine 5’ nucleotidase and other erythrocyte enzymes. Possible role of pyrimidine 5’ nucleotidase in the pathogenesis of lead induced anemia. J Clin Investig 56:1164–1169. https://doi.org/10.1172/JCI108192
Barry PSI (1981) Concentrations of lead in the tissues of children. Br J Ind Med 38:61–71. https://doi.org/10.1136/oem.38.1.61
Barry PSI (1975) A comparison of concentrations of lead in human tissues. Br J Ind Med 32:119–139. https://doi.org/10.1136/oem.32.2.119
Miyake M, Ishigaki K, Suzuki T (1986) Structure refinements of Pb2+ ion-exchanged apatites by X-ray powder pattern-fitting. J Solid State Chem 61:230–235. https://doi.org/10.1016/0022-4596(86)90026-5
Apostolski S, Nikolić J, Bugarski-Prokopljević C et al (1991) Serum and CSF immunological findings in ALS. Acta Neurol Scand 83:96–98. https://doi.org/10.1111/j.1600-0404.1991.tb04656.x
Tarasiuk J, Kułakowska A, Drozdowski W et al (2012) CSF markers in amyotrophic lateral sclerosis. J Neural Transm 119:747–757. https://doi.org/10.1007/s00702-012-0806-y
Vinceti M, Bottecchi I, Fan A et al (2012) Are environmental exposures to selenium, heavy metals, and pesticides risk factors for amyotrophic lateral sclerosis. Rev Environ Health 27:19–41. https://doi.org/10.1515/reveh-2012-0002
Dudev T, Grauffel C, Lim C (2018) How Pb2+ binds and modulates properties of Ca2+-signaling proteins. Inorg Chem 57:14798–14809. https://doi.org/10.1021/acs.inorgchem.8b02548
World Health Organization International Agency for Research on Cancer (2006) Inorganic and organic lead compounds. IARC monographs on the evaluation of carcinogenic risks to humans 87:1–471
Ash PEA, Dhawan U, Boudeau S et al (2019) Heavy metal neurotoxicants induce ALS-linked TDP-43 pathology. Toxicol Sci 167:105–115. https://doi.org/10.1093/toxsci/kfy267
Julian TH, Boddy S, Islam M et al (2022) A review of Mendelian randomization in amyotrophic lateral sclerosis. Brain 145:832–842. https://doi.org/10.1093/brain/awab420
Funding
Open access funding provided by Università degli Studi di Sassari within the CRUI-CARE Agreement. This work was supported from the University of Sassari (Founds FAR-2020, Prof. Roberto Madeddu and Prof. Giuliana Solinas).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval and Informed consent
This work is a work of meta-analysis, which uses data already present in the literature, does not directly involve testing on animals or people, does not require the approval of the ethics committee or informed consent.
Conflict of interest
We declare that none of the authors have conflict of interest with this publication.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Farace, C., Fiorito, G., Pisano, A. et al. Human tissue lead (Pb) levels and amyotrophic lateral sclerosis: a systematic review and meta-analysis of case–control studies. Neurol Sci 43, 5851–5859 (2022). https://doi.org/10.1007/s10072-022-06237-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-022-06237-y