Abstract
Background
Hemorrhagic transformation (HT) is a common complication of acute ischemic stroke (AIS), and inflammation has been found to play an important role in the occurrence of HT. We aimed to investigate the impact of lymphocyte-to-monocyte ratio (LMR), a maker of inflammatory status, on HT in patients with AIS.
Methods
Consecutive AIS patients within 7 days from stroke onset were enrolled between January 2016 and October 2017. LMR was calculated according to lymphocyte and monocyte counts obtained within 24 h on admission. Patients were categorized into three groups according to LMR tertiles. HT was detected by follow-up computed tomography (CT) or magnetic resonance imaging (MRI) during hospitalization. The multivariate logistic analysis was used to evaluate the independent relationship between LMR and HT.
Results
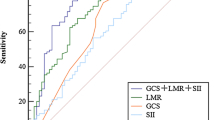
A total of 1005 patients were finally included. HT was observed in 99 (9.9%) patients, with 51 (5.1%) hemorrhagic infarction (HI) and 48 (4.8%) parenchymal hematoma (PH). After adjustment for potential confounders, the odds ratio (OR) of HT was 0.523 (95% confidence interval [CI] 0.293–0.936, P = 0.029) for the highest LMR tertile compared with the lowest tertile. Multiple-adjusted spline regression model showed a nonlinear approximately L-shaped relationship between LMR levels and HT (P for nonlinear trend = 0.030). There was no significant association of baseline LMR with PH (OR 0.562, 95% CI 0.249–1.268, P = 0.165).
Conclusion
Lower LMR was independently related to higher risk of HT in patients with AIS. Admission LMR may be used as one of the predictors for HT. Further prospective multicenter studies are needed to validate our findings.


Similar content being viewed by others
Change history
02 November 2020
We acknowledge that the published works [1, 2] were conducted using data from the Chengdu stroke registry database.
References
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O'Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner L, Wilkins JT, Wong SS, Virani SS, American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee (2019) Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation 139(10):e56–e66. https://doi.org/10.1161/CIR.0000000000000659
Dzialowski I, Pexman JH, Barber PA et al (2007) Asymptomatic hemorrhage after thrombolysis may not be benign: prognosis by hemorrhage type in the Canadian alteplase for stroke effectiveness study registry. Stroke 38(1):75–79. https://doi.org/10.1161/01.STR.0000251644.76546.62
Park JH, Ko Y, Kim WJ et al (2012) Is asymptomatic hemorrhagic transformation really innocuous? Neurology 78(6):421–426. https://doi.org/10.1212/WNL.0b013e318245d22c
Rao NM, Levine SR, Gornbein JA, Saver JL (2014) Defining clinically relevant cerebral hemorrhage after thrombolytic therapy for stroke: analysis of the National Institute of Neurological Disorders and Stroke tissue-type plasminogen activator trials. Stroke 45(9):2728–2733. https://doi.org/10.1161/STROKEAHA.114.005135
Jickling GC, Liu D, Stamova B et al (2014) Hemorrhagic transformation after ischemic stroke in animals and humans. J Cereb Blood Flow Metab 34(2):185–199. https://doi.org/10.1038/jcbfm.2013.203
Duan Z, Wang H, Wang Z, Hao Y, Zi W, Yang D, Zhou Z, Liu W, Lin M, Shi Z, Lv P, Wan Y, Xu G, Xiong Y, Zhu W, Liu X, ACTUAL Investigators (2018) Neutrophil-lymphocyte ratio predicts functional and safety outcomes after endovascular treatment for acute ischemic stroke. Cerebrovasc Dis 45(5–6):221–227. https://doi.org/10.1159/000489401
Guo Z, Yu S, Xiao L, Chen X, Ye R, Zheng P, Dai Q, Sun W, Zhou C, Wang S, Zhu W, Liu X (2016) Dynamic change of neutrophil to lymphocyte ratio and hemorrhagic transformation after thrombolysis in stroke. J Neuroinflammation 13(1):199. https://doi.org/10.1186/s12974-016-0680-x
Gu L, Jian Z, Stary C, Xiong X (2015) T cells and cerebral ischemic stroke. Neurochem Res 40(9):1786–1791. https://doi.org/10.1007/s11064-015-1676-0
Urra X, Villamor N, Amaro S, Gómez-Choco M, Obach V, Oleaga L, Planas AM, Chamorro A (2009) Monocyte subtypes predict clinical course and prognosis in human stroke. J Cereb Blood Flow Metab 29(5):994–1002. https://doi.org/10.1038/jcbfm.2009.25
Liesz A, Suri-Payer E, Veltkamp C, Doerr H, Sommer C, Rivest S, Giese T, Veltkamp R (2009) Regulatory T cells are key cerebroprotective immunomodulators in acute experimental stroke. Nat Med 15(2):192–199. https://doi.org/10.1038/nm.1927
Kim J, Song TJ, Park JH, Lee HS, Nam CM, Nam HS, Kim YD, Heo JH (2012) Different prognostic value of white blood cell subtypes in patients with acute cerebral infarction. Atherosclerosis 222(2):464–467. https://doi.org/10.1016/j.atherosclerosis.2012.02.042
Liesz A, Hu X, Kleinschnitz C, Offner H (2015) Functional role of regulatory lymphocytes in stroke: facts and controversies. Stroke 46(5):1422–1430. https://doi.org/10.1161/STROKEAHA.114.008608
Liberale L, Montecucco F, Bonaventura A, Casetta I, Seraceni S, Trentini A, Padroni M, Dallegri F, Fainardi E, Carbone F (2017) Monocyte count at onset predicts poststroke outcomes during a 90-day follow-up. Eur J Clin Investig 47(10):702–710. https://doi.org/10.1111/eci.12795
Enciu AM, Gherghiceanu M, Popescu BO (2013) Triggers and effectors of oxidative stress at blood-brain barrier level: relevance for brain ageing and neurodegeneration. Oxidative Med Cell Longev 2013:297512. https://doi.org/10.1155/2013/297512
Nishijima TF, Muss HB, Shachar SS, Tamura K, Takamatsu Y (2015) Prognostic value of lymphocyte-to-monocyte ratio in patients with solid tumors: a systematic review and meta-analysis. Cancer Treat Rev 41(10):971–978. https://doi.org/10.1016/j.ctrv.2015.10.003
Mano Y, Yoshizumi T, Yugawa K, Ohira M, Motomura T, Toshima T, Itoh S, Harada N, Ikegami T, Soejima Y, Maehara Y (2018) Lymphocyte-to-monocyte ratio is a predictor of survival after liver transplantation for hepatocellular carcinoma. Liver Transpl 24(11):1603–1611. https://doi.org/10.1002/lt.25204
Kwon BS, Jeong DH, Byun JM, Lee TH, Choi KU, Song YJ, Suh DS, Kim KH (2018) Prognostic value of preoperative lymphocyte-monocyte ratio in patients with ovarian clear cell carcinoma. J Cancer 9(7):1127–1134. https://doi.org/10.7150/jca.24057
Wang Q, Ma J, Jiang Z, Wu F, Ping J, Ming L (2017) Association of lymphocyte-to-monocyte ratio with in-hospital and long-term major adverse cardiac and cerebrovascular events in patients with ST-elevated myocardial infarction. Medicine (Baltimore) 96 (34):e7897. doi:https://doi.org/10.1097/MD.0000000000007897
Fan Z, Li Y, Ji H, Jian X (2018) Prognostic utility of the combination of monocyte-to-lymphocyte ratio and neutrophil-to-lymphocyte ratio in patients with NSTEMI after primary percutaneous coronary intervention: a retrospective cohort study. BMJ Open 8 (10):e023459. doi:https://doi.org/10.1136/bmjopen-2018-023459
Ren H, Liu X, Wang L, Gao Y (2017) Lymphocyte-to-monocyte ratio: a novel predictor of the prognosis of acute ischemic stroke. J Stroke Cerebrovasc Dis 26(11):2595–2602. https://doi.org/10.1016/j.jstrokecerebrovasdis.2017.06.019
Ren H, Han L, Liu H, Wang L, Liu X, Gao Y (2017) Decreased lymphocyte-to-monocyte ratio predicts poor prognosis of acute ischemic stroke treated with thrombolysis. Med Sci Monit 23:5826–5833
Park MG, Kim MK, Chae SH, Kim HK, Han J, Park KP (2018) Lymphocyte-to-monocyte ratio on day 7 is associated with outcomes in acute ischemic stroke. Neurol Sci 39(2):243–249. https://doi.org/10.1007/s10072-017-3163-7
Qi H, Wang D, Deng X, Pang X (2018) Lymphocyte-to-monocyte ratio is an independent predictor for neurological deterioration and 90-day mortality in spontaneous Intracerebral hemorrhage. Med Sci Monit 24:9282–9291. https://doi.org/10.12659/MSM.911645
Wang D, Liu M, Hao Z, Tao W, Lin S, Zhang S, Wu B, Ma Z, Dong W (2012) Features of acute ischemic stroke with rheumatic heart disease in a hospitalized Chinese population. Stroke 43(11):2853–2857. https://doi.org/10.1161/STROKEAHA.112.670893
Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, Strasser T (1980) Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ 58(1):113–130
Ott BR, Zamani A, Kleefield J, Funkenstein HH (1986) The clinical spectrum of hemorrhagic infarction. Stroke 17(4):630–637
Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, Larrue V, Lees KR, Medeghri Z, Machnig T, Schneider D, von Kummer R, Wahlgren N, Toni D, ECASS Investigators (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. New Engl J Med 359(13):1317–1329. https://doi.org/10.1056/NEJMoa0804656
Durrleman S, Simon R (1989) Flexible regression models with cubic splines. Stat Med 8(5):551–561
Paciaroni M, Agnelli G, Corea F et al (2008) Early hemorrhagic transformation of brain infarction: rate, predictive factors, and influence on clinical outcome: results of a prospective multicenter study. Stroke 39(8):2249–2256. https://doi.org/10.1161/STROKEAHA.107.510321
Deng Q-W, Liu Y-K, Zhang Y-Q et al (2019) Low triglyceride to high-density lipoprotein cholesterol ratio predicts hemorrhagic transformation in large atherosclerotic infarction of acute ischemic stroke. Aging-US 11(5):1589–1601
Terruso V, D'Amelio M, Di Benedetto N et al (2009) Frequency and determinants for hemorrhagic transformation of cerebral infarction. Neuroepidemiology 33(3):261–265. https://doi.org/10.1159/000229781
Wang L, Song Q, Wang C, Wu S, Deng L, Li Y, Zheng L, Liu M (2019) Neutrophil to lymphocyte ratio predicts poor outcomes after acute ischemic stroke: a cohort study and systematic review. J Neurol Sci 406:116445. https://doi.org/10.1016/j.jns.2019.116445
Wei CC, Zhang ST, Tan G, Zhang SH, Liu M (2018) Impact of anemia on in-hospital complications after ischemic stroke. Eur J Neurol 25(5):768–774. https://doi.org/10.1111/ene.13595
Tan G, Lei C, Hao Z et al (2016) Liver function may play an uneven role in haemorrhagic transformation for stroke subtypes after acute ischaemic stroke. Eur J Neurol 23(3):597–604. https://doi.org/10.1111/ene.12904
Li P, Mao L, Zhou G, Leak RK, Sun BL, Chen J, Hu X (2013) Adoptive regulatory T-cell therapy preserves systemic immune homeostasis after cerebral ischemia. Stroke 44(12):3509–3515. https://doi.org/10.1161/STROKEAHA.113.002637
Chiu NL, Kaiser B, Nguyen YV, Welbourne S, Lall C, Cramer SC (2016) The volume of the spleen and its correlates after acute stroke. J Stroke Cerebrovasc Dis 25(12):2958–2961. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.08.012
Yamamoto Y, Osanai T, Nishizaki F, Sukekawa T, Izumiyama K, Sagara S, Okumura K (2012) Matrix metalloprotein-9 activation under cell-to-cell interaction between endothelial cells and monocytes: possible role of hypoxia and tumor necrosis factor-alpha. Heart Vessel 27(6):624–633. https://doi.org/10.1007/s00380-011-0214-5
del Zoppo GJ, Frankowski H, Gu YH, Osada T, Kanazawa M, Milner R, Wang X, Hosomi N, Mabuchi T, Koziol JA (2012) Microglial cell activation is a source of metalloproteinase generation during hemorrhagic transformation. J Cereb Blood Flow Metab 32(5):919–932. https://doi.org/10.1038/jcbfm.2012.11
Garcia-Culebras A, Duran-Laforet V, Pena-Martinez C et al (2018) Myeloid cells as therapeutic targets in neuroinflammation after stroke: specific roles of neutrophils and neutrophil-platelet interactions. J Cereb Blood Flow Metab 38(12):2150–2164. https://doi.org/10.1177/0271678X18795789
Liesz A, Dalpke A, Mracsko E, Antoine DJ, Roth S, Zhou W, Yang H, Na SY, Akhisaroglu M, Fleming T, Eigenbrod T, Nawroth PP, Tracey KJ, Veltkamp R (2015) DAMP signaling is a key pathway inducing immune modulation after brain injury. J Neurosci 35(2):583–598. https://doi.org/10.1523/JNEUROSCI.2439-14.2015
Funding
This study was funded by the Key Research and Development Program, Science & Technology Department of Sichuan Province (Grant No. 2017SZ0007) and the Major International (Regional) Joint Research Project, National Natural Science Foundation of China (Grant No. 81620108009).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval
The study protocol was performed in accordance with the Declaration of Helsinki and approved by the Biomedical Research Ethics Committee of West China Hospital, Sichuan University. Informed consent was obtained from all patients or their legal guardians.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 55.2 kb)
Rights and permissions
About this article
Cite this article
Song, Q., Pan, R., Jin, Y. et al. Lymphocyte-to-monocyte ratio and risk of hemorrhagic transformation in patients with acute ischemic stroke. Neurol Sci 41, 2511–2520 (2020). https://doi.org/10.1007/s10072-020-04355-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-020-04355-z