Abstract
Background and purpose
Various types of cerebral small vessel diseases (CSVD) are commonly coexisting and the clinical outcome possibly is determined by their combined effect. The present study was designed to explore the possible relationship between the global burden of CSVD and clinical outcomes after recombinant tissue plasminogen activator (rt-PA) treatment of ischemic stroke.
Methods
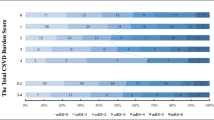
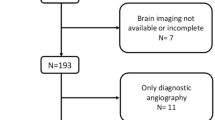
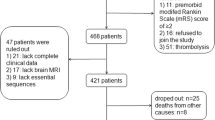
We enrolled patients with acute ischemic stroke (AIS) after IV rt-PA treatment between August 2016 and July 2018. According to the total burden rating scale of CSVD, we calculated the total CSVD score for white matter hyperintensities, lacunar infarction, cerebral microbleeds, and perivascular spaces. All patients were assessed on the basis of the National Institutes of Health Stroke Scale (NIHSS) score and the modified Rankin Scale (mRS) score at 90 days after stroke. We used multivariate logistic regression analysis to examine the associations between global burden of CSVD and degree of neurological deficit and clinical outcomes. ROC curve analysis was used to determine cut-off values of the total CSVD score in predicting poor outcomes.
Results
The results showed that the total CSVD score was independently associated with moderate to severe stroke (OR 2.187, 95%CI 1.495–3.119, P < 0.001). Initial NIHSS (OR 1.23, 95%CI 1.144–1.330, P < 0.001), OTT (OR 1.007, 95%CI 1.000–1.014, P = 0.037), and CSVD score (OR 3.157, 95%CI 2.120–4.703, P < 0.001) was significantly related to poor functional outcome at 3 months. The total CVSD score cut-off value of 1.5 was determined at best to distinguish between good prognosis and poor outcome (AUC 0.7534 [95%CI 0.6883–0.8185]).
Conclusions
The global burden of CSVD was independently associated with neurological deficit severity and clinical outcomes of AIS after IV rt-PA treatment. The total CVSD score is a reliable predictor for poor outcomes of AIS after IV rt-PA treatment.




Similar content being viewed by others
References
Khoshnam SE, Winlow W, Farzaneh M, Farbood Y, Moghaddam HF (2017) Pathogenic mechanisms following ischemic stroke. Neurol Sci 38(7):1167–1186. https://doi.org/10.1007/s10072-017-2938-1
Tejada-Meza H, Modrego PJ (2017) Cerebellar vermis: a vulnerable location of remote brain haemorrhages after thrombolysis for ischaemic stroke. Neurol Sci 38(1):185–187. https://doi.org/10.1007/s10072-016-2728-1
Wardlaw JM, Smith C, Dichgans M (2013) Mechanisms of sporadic cerebral small vessel disease: insights from neuroimaging. Lancet Neurol 12(5):483–497. https://doi.org/10.1016/S1474-4422(13)70060-7
Shi Y, Wardlaw JM (2016) Update on cerebral small vessel disease: a dynamic whole-brain disease. Stroke Vasc Neurol 1(3):83–92. https://doi.org/10.1136/svn-2016-000035
Inzitari D (2003) Leukoaraiosis: an independent risk factor for stroke? Stroke 34(8):2067–2071. https://doi.org/10.1161/01.STR.0000080934.68280.82
Rajani RM, Williams A (2017) Endothelial cell-oligodendrocyte interactions in small vessel disease and aging. Clin Sci 131(5):369–379. https://doi.org/10.1042/CS20160618
Hainsworth AH, Fisher MJ (2017) A dysfunctional blood-brain barrier and cerebral small vessel disease. Neurology 88(5):420–421. https://doi.org/10.1212/WNL.0000000000003561
Shi Y, Thrippleton MJ, Makin SD, Marshall I, Geerlings MI, de Craen AJ, van Buchem MA, Wardlaw JM (2016) Cerebral blood flow in small vessel disease: a systematic review and meta-analysis. J Cereb Blood Flow Metab 36(10):1653–1667. https://doi.org/10.1177/0271678X16662891
Henninger N, Lin E, Haussen DC, Lehman LL, Takhtani D, Selim M, Moonis M (2013) Leukoaraiosis and sex predict the hyperacute ischemic core volume. Stroke 44(1):61–67. https://doi.org/10.1161/STROKEAHA.112.679084
Ay H, Arsava EM, Rosand J, Furie KL, Singhal AB, Schaefer PW, Wu O, Gonzalez RG, Koroshetz WJ, Sorensen AG (2008) Severity of leukoaraiosis and susceptibility to infarct growth in acute stroke. Stroke 39(5):1409–1413. https://doi.org/10.1161/STROKEAHA.107.501932
Henninger N, Khan MA, Zhang J, Moonis M, Goddeau RP Jr (2014) Leukoaraiosis predicts cortical infarct volume after distal middle cerebral artery occlusion. Stroke 45(3):689–695. https://doi.org/10.1161/STROKEAHA.113.002855
Helenius J, Henninger N (2015) Leukoaraiosis burden significantly modulates the association between infarct volume and National Institutes of Health stroke scale in ischemic stroke. Stroke 46(7):1857–1863. https://doi.org/10.1161/STROKEAHA.115.009258
Liu Y, Gong P, Sun H, Zhang S, Zhou J, Zhang Y (2019) Leukoaraiosis is associated with poor outcomes after successful recanalization for large vessel occlusion stroke. Neurol Sci. https://doi.org/10.1007/s10072-018-3698-2
Curtze S, Haapaniemi E, Melkas S, Mustanoja S, Putaala J, Sairanen T, Sibolt G, Tiainen M, Tatlisumak T, Strbian D (2015) White matter lesions double the risk of post-thrombolytic intracerebral hemorrhage. Stroke 46(8):2149–2155. https://doi.org/10.1161/STROKEAHA.115.009318
Zand R, Tsivgoulis G, Singh M, McCormack M, Goyal N, Ishfaq MF, Shahripour RB, Nearing K, Elijovich L, Alexandrov AW, Liebeskind DS, Alexandrov AV (2017) Cerebral microbleeds and risk of intracerebral hemorrhage post intravenous thrombolysis. J Stroke Cerebrovasc Dis 26(3):538–544. https://doi.org/10.1016/j.jstrokecerebrovasdis.2016.11.127
Huijts M, Duits A, van Oostenbrugge RJ, Kroon AA, de Leeuw PW, Staals J (2013) Accumulation of MRI markers of cerebral small vessel disease is associated with decreased cognitive function. A study in first-ever lacunar stroke and hypertensive patients. Front Aging Neurosci 5:72. https://doi.org/10.3389/fnagi.2013.00072
Staals J, Booth T, Morris Z, Bastin ME, Gow AJ, Corley J, Redmond P, Starr JM, Deary IJ, Wardlaw JM (2015) Total MRI load of cerebral small vessel disease and cognitive ability in older people. Neurobiol Aging 36(10):2806–2811. https://doi.org/10.1016/j.neurobiolaging.2015.06.024
Brenner D, Labreuche J, Pico F, Scheltens P, Poirier O, Cambien F, Amarenco P, Investigators G (2008) The renin-angiotensin-aldosterone system in cerebral small vessel disease. J Neurol 255(7):993–1000. https://doi.org/10.1007/s00415-008-0816-8
Pico F, Labreuche J, Touboul PJ, Leys D, Amarenco P (2005) Intracranial arterial dolichoectasia and small-vessel disease in stroke patients. Ann Neurol 57(4):472–479. https://doi.org/10.1002/ana.20423
Klarenbeek P, van Oostenbrugge RJ, Rouhl RP, Knottnerus IL, Staals J (2013) Ambulatory blood pressure in patients with lacunar stroke: association with total MRI burden of cerebral small vessel disease. Stroke 44(11):2995–2999. https://doi.org/10.1161/STROKEAHA.113.002545
Uiterwijk R, van Oostenbrugge RJ, Huijts M, De Leeuw PW, Kroon AA, Staals J (2016) Total cerebral small vessel disease MRI score is associated with cognitive decline in executive function in patients with hypertension. Front Aging Neurosci 8:301. https://doi.org/10.3389/fnagi.2016.00301
Wardlaw JM, Smith EE, Biessels GJ, Cordonnier C, Fazekas F, Frayne R, Lindley RI, O'Brien JT, Barkhof F, Benavente OR, Black SE, Brayne C, Breteler M, Chabriat H, Decarli C, de Leeuw FE, Doubal F, Duering M, Fox NC, Greenberg S, Hachinski V, Kilimann I, Mok V, Oostenbrugge R, Pantoni L, Speck O, Stephan BC, Teipel S, Viswanathan A, Werring D, Chen C, Smith C, van Buchem M, Norrving B, Gorelick PB, Dichgans M, nEuroimaging STfRVco (2013) Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol 12(8):822–838. https://doi.org/10.1016/S1474-4422(13)70124-8
Doubal FN, MacLullich AM, Ferguson KJ, Dennis MS, Wardlaw JM (2010) Enlarged perivascular spaces on MRI are a feature of cerebral small vessel disease. Stroke 41(3):450–454. https://doi.org/10.1161/STROKEAHA.109.564914
Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA (1987) MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol 149(2):351–356. https://doi.org/10.2214/ajr.149.2.351
Staals J, Makin SD, Doubal FN, Dennis MS, Wardlaw JM (2014) Stroke subtype, vascular risk factors, and total MRI brain small-vessel disease burden. Neurology 83(14):1228–1234. https://doi.org/10.1212/WNL.0000000000000837
Arba F, Inzitari D, Ali M, Warach SJ, Luby M, Lees KR, Collaboration SVI (2017) Small vessel disease and clinical outcomes after IV rt-PA treatment. Acta Neurol Scand 136(1):72–77. https://doi.org/10.1111/ane.12745
Lau KK, Li L, Schulz U, Simoni M, Chan KH, Ho SL, Cheung RTF, Kuker W, Mak HKF, Rothwell PM (2017) Total small vessel disease score and risk of recurrent stroke: validation in 2 large cohorts. Neurology 88(24):2260–2267. https://doi.org/10.1212/WNL.0000000000004042
Bandettini di Poggio M, Finocchi C, Brizzo F, Altomonte F, Bovis F, Mavilio N, Serrati C, Malfatto L, Mancardi G, Balestrino M (2019) Management of acute ischemic stroke, thrombolysis rate, and predictors of clinical outcome. Neurol Sci 40(2):319–326. https://doi.org/10.1007/s10072-018-3644-3
Abdul-Rahim AH, Fulton RL, Sucharew H, Kleindorfer D, Khatri P, Broderick JP, Lees KR, Collaborators V (2015) National institutes of health stroke scale item profiles as predictor of patient outcome: external validation on independent trial data. Stroke 46(2):395–400. https://doi.org/10.1161/STROKEAHA.114.006837
Adams HP Jr, Davis PH, Leira EC, Chang KC, Bendixen BH, Clarke WR, Woolson RF, Hansen MD (1999) Baseline NIH stroke scale score strongly predicts outcome after stroke: a report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST). Neurology 53(1):126–131
Yaghi S, Willey JZ, Cucchiara B, Goldstein JN, Gonzales NR, Khatri P, Kim LJ, Mayer SA, Sheth KN, Schwamm LH, American Heart Association Stroke C, Council on C, Stroke N, Council on Clinical C, Council on Quality of C, Outcomes R (2017) Treatment and outcome of hemorrhagic transformation after intravenous alteplase in acute ischemic stroke: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 48(12):e343–e361. https://doi.org/10.1161/STR.0000000000000152
Yaghi S, Eisenberger A, Willey JZ (2014) Symptomatic intracerebral hemorrhage in acute ischemic stroke after thrombolysis with intravenous recombinant tissue plasminogen activator: a review of natural history and treatment. JAMA Neurol 71(9):1181–1185. https://doi.org/10.1001/jamaneurol.2014.1210
Funding
This study was funded by the National Key R&D Program of China (2017YFC0114300) and Science and Technology Department Key Diseases Standardized Diagnosis and Treatment Project of Jiangsu Provincial.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
The study was approved by the ethics committees of the First Hospital Affiliated to Soochow University (No. 2018104) without need for informed consent.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Liu, X., Li, T., Diao, S. et al. The global burden of cerebral small vessel disease related to neurological deficit severity and clinical outcomes of acute ischemic stroke after IV rt-PA treatment. Neurol Sci 40, 1157–1166 (2019). https://doi.org/10.1007/s10072-019-03790-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-019-03790-x