Abstract
Objective
Narcolepsy is a lifelong disease, manifesting with excessive daytime sleepiness and cataplexy, arising between childhood and young adulthood. The diagnosis is typically made after a long delay that burdens the disease severity. The aim of the project, promoted by the “Associazione Italiana Narcolettici e Ipersonni” is to develop Red Flags to detect symptoms for early referral, targeting non-sleep medicine specialists, general practitioners, and pediatricians.
Materials and methods
A multidisciplinary panel, including patients, public institutions, and representatives of national scientific societies of specialties possibly involved in the diagnostic process of suspected narcolepsy, was convened. The project was accomplished in three phases. Phase 1: Sleep experts shaped clinical pictures of narcolepsy in pediatric and adult patients. On the basis of these pictures, Red Flags were drafted. Phase 2: Representatives of the scientific societies and patients filled in a form to identify barriers to the diagnosis of narcolepsy. Phase 3: The panel produced suggestions for the implementation of Red Flags.
Results
Red Flags were produced representing three clinical pictures of narcolepsy in pediatric patients ((1) usual sleep symptoms, (2) unusual sleep symptoms, (3) endocrinological signs) and two in adult patients ((1) usual sleep symptoms, (2) unusual sleep symptoms). Inadequate knowledge of symptoms at onset by medical doctors turned out to be the main reported barrier to diagnosis.
Conclusions
This report will hopefully enhance knowledge and awareness of narcolepsy among non-specialists in sleep medicine in order to reduce the diagnostic delay that burdens patients in Italy. Similar initiatives could be promoted across Europe.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Narcolepsy is characterized by the pentad of excessive daytime sleepiness, cataplexy, hypnagogic or hypnopompic hallucinations, sleep paralysis, and disrupted nighttime sleep [1,2,3]. It is a chronic and disabling disorder, with a bimodal peak for age at onset, with a maximal rate of onset at 15 years and the second peak at 35 years, needing a lifelong treatment [4].
Narcolepsy has a prevalence between 20 and 50 per 100,000 [5,6,7,8,9,10,11] and is recognized as rare disease (RF 0150) by the Italian Ministry of Health [attachment 1 at DM N. 279/2001]. At December 31, 2014, 610 patients were recorded in Italy by the National Registry for Rare Diseases [12], with an average national annual incidence in the 3-year period 2012–2014 of 0.97 per 1 million person-years [13] compared to an annual incidence of 1.37 per 100,000 person-years in Olmsted County, Minnesota (USA) [7].
The current classification [1] distinguishes narcolepsy type 1 (NT1) and narcolepsy type 2 (NT2). Both types feature daytime sleepiness confirmed by polysomnographic studies, while hypocretin level of less than 110 pg/mL and the presence of cataplexy characterize only NT1. Therefore, NT1 is linked to the loss of hypothalamic hypocretinergic neurons, while the cause of NT2 remains unknown. Both genetic and environmental factors play a crucial role in the pathogenesis of narcolepsy. Most patients with narcolepsy carry HLA-DQB1*0602 and a link to polymorphisms in other non-HLA genes that may affect immune regulatory function and to several infectious triggers, supporting an autoimmune pathogenesis [2, 3].
Although narcolepsy has an early onset, a diagnostic delay that often exceeds 10 years from symptoms onset is reported [14,15,16,17,18]. Lately, there has been a trend toward a shorter diagnostic delay, which could potentially be attributed to an increased awareness of narcolepsy, as for example in Italy through media campaigns [https://www.narcolessia.org]. However, as emerged from a recent survey conducted by the Italian association of patients with narcolepsy and hypersomnia (Associazione Italiana Narcolettici e Ipersonni – AIN; https://www.narcolessia.org), diagnostic delay continues to be an issue, which makes identifying its causes a priority.
Data from several studies and reviews suggest that the primary reason for diagnostic delay is likely the lack of symptoms recognition, often resulting in misdiagnosis [14,15,16, 18,19,20,21,22]. This may originate from several factors, including lack of recognition, on the part of the clinician, of the signs and symptoms of narcolepsy, leading to multiple referrals before receiving a proper diagnosis [14, 20,21,22] as well as misdiagnosis of narcolepsy as another condition, such as epilepsy, depression, or attention-deficit/hyperactivity disorder, which further delays treatment [14, 19, 20, 23, 24].
Receiving a correct narcolepsy diagnosis is especially relevant in children, in order to timely face consequences, such as low academic achievement and social difficulties [18]. This is an important pitfall to be addressed, as misdiagnosis is more common in pediatric narcolepsy [19, 20, 25]. Indeed, the strongest predictor of a delayed diagnosis, along with the absence of cataplexy, has been reported to be pediatric onset of symptoms [26]. Diagnosis of narcolepsy indeed may be particularly challenging in children as symptoms may manifest differently from adults. Excessive daytime sleepiness can manifest as attentional problems, paradoxical hyperactivity, elongation of nighttime sleep, and resuming of postprandial sleep [3]. Hallucinations can be underrecognized because of the difficulty for children to recognize and describe them and for the possible coexistence of nightmares, rapid eye movement (REM) sleep behavior disorder (RBD), sleep terrors, and confusional arousals [26, 27]. Children with NT1 may have peculiar features of cataplexy with subcontinuous hypotonia, mainly involving the facial district “cataplectic face” and superimposed dyskinesia [23, 24, 28].
Timely diagnosis means better outcomes and it has been reported that patients diagnosed before age 30 years exhibit lower unemployment rates and have better health perception than those diagnosed at a later age [29], therefore resulting in reduced psychological distress along with socioeconomic and healthcare consequences [30,31,32,33,34]. Accordingly, it is important to understand the reason of this pitfall in diagnosis and to act in order to correct this gap and improve the rate of a timely diagnosis.
Considering these premises and the result of the above-mentioned AIN survey, AIN itself has promoted this document with the specific aim of exploring, at multiple levels of the healthcare system, the causes of diagnostic pitfalls and of proposing corrective actions. We propose of doing this through Red Flags aimed at detecting narcolepsy symptoms early and timely referring potentially affected individuals to specialist care.
Objective
The aim of the project is to develop Red Flags to improve the knowledge about the symptoms suggestive of narcolepsy among non-sleep medicine expert physicians potentially involved in the first referral of patients (neurologists, pediatric neurologists, general practitioners, and pediatricians) for early referral to sleep medicine centers. The focus is the definition of the exemplary (chief complaint) and atypical (variant complaint) clinical presentations of narcolepsy, at its onset or when fully developed, in children and in adults. The analysis of barriers and facilitators of the diagnostic suspicion of narcolepsy was carried out with the aim of suggesting strategies for the implementation of the Red Flags.
Methods
The current document is a position paper, promoted by AIN, based on experts’ and stakeholders’ opinions. The following scientific societies endorsed the project by appointing a representative member of each society: the Italian society of neurology (Società Italiana di Neurologia, SIN; P. C.); the Italian society of pediatric neurology (Società Italiana Neurologia Pediatrica, SINP; V. M.); the Italian society of social and preventive medicine (Società Italiana di Pediatria Preventiva e Sociale, SIPPS; M.C. V.); the Italian society of pediatrics (Società Italiana di Pediatria, SIP; E. V.); the Italian society of general practitioners (Società Italiana di Medicina Generale, SIMG; M. B.); the Italian society of neurophychiatrists for children and adolescents (Società italiana di neuropsichiatria dell’infanzia e dell’adolescenza, SIMPIA; R. G., F. M.); the World Association of Sleep Medicine (WASM; L. F-S.); the Italian association of sleep medicine (Associazione Italiana Medicina del Sonno, AIMS; R. F.), the Italian association of healthcare managers (Associazione Nazionale Medici di Direzione Ospedaliera; ANMDO; G. P.). A scientific committee was established, including a patients’ representative (I. C., AIN), methodology experts from IRCCS Istituto delle Neuroscienze di Bologna (L. V.) and Italian institute of health - National Centre for Rare Diseases (Istituto Superiore di Sanità, ISS: C. C., D. T.), and narcolepsy experts (E. A., F. P., F. I., L. F-S., R. F. and G. P.).
The document was planned at an initial meeting of the scientific committee and scientific societies spokespersons in Bologna (Italy), July 21, 2017. Three phases were conceived: (1) Red Flags editing; (2) barriers and facilitators analysis; (3) suggestions for Red Flags implementation.
Red Flags editing
Based on the AASM ICSD 3 [1] criteria for narcolepsy and by consulting evidence-based summaries [35,36,37], sleep experts defined the exemplary and atypical clinical pictures of narcolepsy, at onset or fully developed, in children and in adults. In particular, each Red Flag was edited as a short statement including the alerting symptom(s), either according to the possible chief complaints or the possible variant complaints. An explanation box, reporting examples of real-life presentation of symptoms, equipped each Red Flag. For each piece of evidence at the basis of the statement, the possible references labeled with their study design were reported. A first draft was submitted to the whole members group and a final consensus version was achieved. Red Flags were edited in Italian then translated into English (See Supplementary Material).
Barriers and facilitators analysis
An electronic questionnaire was built to investigate barriers and facilitators of the diagnostic suspicion of narcolepsy. The questionnaire was designed according to the “Tailored Implementation for Chronic Diseases” (TICD) checklist [38], a comprehensive tool that identifies determinants, that is barriers and facilitators, of healthcare professional practice. Briefly, it includes 57 potential determinants of practice, grouped in seven domains (guideline factors; individual health professional factors; patient factors; professional interactions; incentives and resources; capacity for organizational change; and social, political, and legal factors). The scientific committee chose the relevant domains and determinants conceivably involved in the diagnostic process of patients with suspicion of narcolepsy. Each determinant was transformed as question with a 4-point Likert scale (possible answers: “strongly agree,” “agree,” “disagree,” “strongly disagree”). The checklist was then edited in three versions and submitted to the scientific societies spokespersons, child patient caregivers, and adult patients. Patients and caregivers were invited by AIN.
Suggestions for Red Flags implementation
A list of suggestions aiming at the implementation of the Red Flags, based on the results of the Phase 2 analysis, was edited by the whole group during a final meeting.
Results
Red Flags were produced representing three clinical pictures of narcolepsy in children (picture with (1) usual sleep symptoms, (2) unusual sleep symptoms, (3) metabolic symptoms) and two in adults (picture with (1) usual sleep symptoms, (2) unusual sleep symptoms). See Supplementary Material for original version in Italian.
Red flags for pediatric patients
Narcolepsy should be suspected in pediatric patients that present with…
➔In this case, it is recommended that the patient should be referred to the reference centers for the diagnosis.
-
2.
peculiar sleep-related disorders, i.e., hypnagogic-hypnopompic hallucination, sleep paralysis, and impaired nocturnal sleep (see Table 3 for explanations).
➔ In this case, it is recommended that the presence of excessive daytime sleepiness and cataplexy (as indicated in Red Flag 1) should be investigated, even if these symptoms are not directly reported by the patient. In case of positive history of excessive daytime sleepiness and/or cataplexy, it is recommended that the patient should be referred to the reference centers for the diagnosis
-
3.
signs of precocious puberty and/or increase of weight until the development of obesity (see Table 4 for explanations).
➔ In this case, it is recommended that the presence of excessive daytime sleepiness and cataplexy (as indicated in Red Flag 1) should be investigated, even if these symptoms are not directly reported by the patient. In case of positive history of excessive daytime sleepiness and/or cataplexy, it is recommended that the patient should be referred to the reference centers for the diagnosis.
Red flags for adult patients
Narcolepsy should be suspected in adult patients that present with …
➔In this case, it is recommended that the patient should be referred to the reference centers for the diagnosis.
-
2.
peculiar sleep-related disorder, i.e., hypnagogic-hypnopompic hallucination, sleep paralysis, and impaired nocturnal (see Table 7 for explanations).
➔ In this case, it is recommended that the presence of excessive daytime sleepiness and cataplexy (as indicated in Red Flag 1) should be investigated, even if these symptoms are not directly reported by the patient. In case of positive history of excessive daytime sleepiness and/or cataplexy, it is recommended that the patient should be referred to the reference centers for the diagnosis.
Barriers and facilitators analysis
The following domains and determinants were selected from the TICD checklist to design and to analyze questionnaire results: (a) individual health professional factors (knowledge and skills; cognition and attitudes; professional behavior); (b) patient factors (needs; beliefs and knowledge; preferences; motivation; behavior); (c) professional interactions (referral processes); (d) incentives and resources (nonfinancial incentives and disincentives; assistance for clinicians); (e) capacity for organizational change (regulations, rules policies); (f) social, political, and legal factors (legislation).
Scientific societies spokespersons
Five specialist spokespersons completed the survey (a general practitioner, a neurologist, a child neuropsychiatrist, a child neurologist, a general pediatrician).
For most specialists, main barriers of diagnostic suspicion of narcolepsy are the insufficient knowledge of symptoms at onset, and the insufficient skill or propensity to examine symptoms when they are considered atypical (elongation of 24-h sleep, hallucinations, cataplexy, nighttime sleep disruption with rapid eye movement (REM) sleep behavior disorder, sleep terrors) or when they are reported as disease consequences (attentional problems, paradoxical hyperactivity, worsening of school or work performances). Another barrier is represented by the difficult referral process to expert sleep centers, due to the geographical distance or the difficulty of booking an appointment. Social or legal factors are not deemed as a relevant cause of the diagnostic delay; however, the fear of losing the driving license was raised by one specialist as a possible diagnostic barrier. Possible facilitators are tools to elicit the diagnostic suspicion or to improve the knowledge (questionnaires and educational materials, both printed and on the web; toll-free number) and organizational changes to simplify the access to expert sleep centers (dedicated outpatients’ clinic; diagnostic–therapeutic pathway).
Pediatric patients
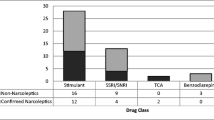
Twenty-three caregivers of pediatric patients (14 males/9 females) completed the survey; narcolepsy type 1 was the prevalent diagnosis (21). The sample was quite homogeneously distributed in the Italian areas (north west 39%; north east 14%; middle 30%; south and islands 17%). Median age at onset was 9 years, and mean diagnostic delay 2.1 years (SD 3.5; median 1; range 0–14). Narcolepsy was not suspected at the first visit in 61% of patients; 47% of them consulted more than two physicians, and up to 10 in one case. Reported alternative diagnoses (in 48% of patients) are other organic disorders (epilepsy, obstructive sleep apnea syndrome, brain neoplasm, iron deficiency, drug abuse, tics, precocious puberty), psychological problems, abnormal attitudes/behaviors (boredom, laziness).
Main barrier to the diagnostic suspicion of narcolepsy was the inadequate knowledge of the disease by physicians (see Table 8). Relevant was also the scarce awareness of symptoms in their child by parents. To be noticed, the presence of more popular competing disorders (see above) among the possible barriers to diagnostic suspicion.
Adult patients
Forty-eight adult patients (25 males/23 females) completed the survey; narcolepsy type 1 was the prevalent diagnosis (32). The sample was quite homogeneously distributed in the Italian areas (north west 26%; north east 22%; middle 22%; south and islands 30%). Median age at onset was 11 years, mean diagnostic delay 6.7 years (SD 7.3; median 3.5; range 0–42). Narcolepsy was not suspected at first visit in 67% of patients; 59% of them consulted more than two physicians, and up to 10 in three cases. Reported alternative diagnoses (in 48% of patients) included other organic disorders (42%: epilepsy, obstructive sleep apnea syndrome, restless leg syndrome, gastroesophageal reflux, post-viral syndrome, obesity) and psychiatric disorders (43%: depression, anxiety), abnormal attitudes/behaviors (15%: laziness, tiredness).
Main barrier to the diagnostic suspicion of narcolepsy is the insufficient knowledge of the disease by physicians (see Table 8) and the scarce awareness of symptoms by patients. To be noticed, the presence of more popular competing disorders among the possible barriers to diagnostic suspicion. The presence of social/legislation factors (not acceptance of the disease, fear of social and work limitations, fear of driving license loss) is also reported as relevant by 1/3 of patients.
Suggestions for Red Flags implementation
After the analysis of the above reported data, the multidisciplinary panel agreed on the following suggestions to implement the above reported Red Flags.
-
The Red Flags should be the object of a national campaign, with presentation at national congresses and meetings and publications in Italian journals targeted to the specialties relevant to the project.
-
The Red Flags should be disseminated with simple educational materials, such as leaflets with cartoons or as web movies that can be distributed in primary care centers, or at school, where symptoms can be firstly recognized.
-
To facilitate the access to the reference centers, in collaboration with the National Helpline on Rare Diseases (Telefono Verde Malattie Rare 800 89 69 49) of the Istituto Superiore di Sanità (National Centre for Rare Diseases), a national central call-center could be designed in order to drive and help clinicians in referring the patients to the nearest and more appropriate center.
-
The recognition of the symptoms by physicians could be elicited by validated questionnaires. Due to the scarcity of these tools in the Italian language (e.g., [61, 62] considering only excessive daytime sleepiness), a tool including the whole Red Flags should be devised and validated.
-
The efficacy of the Red Flags implementation in reducing the diagnostic gap of patients with narcolepsy could be the object of a national multi-center study (e.g., an interrupted time series study).
-
Similar initiatives could be promoted across European countries.
Discussion
Narcolepsy is still a disease burdened by an unacceptable diagnostic delay [18, 26] and possibly by missed diagnoses in Italy [12, 13].
The persistence of a substantial delay in recognizing symptoms of narcolepsy, even among sleep medicine specialists, has been highlighted also by the Awareness and Knowledge of Narcolepsy (AWAKEN) study [21]. This is a survey including a sample of 1000 US adults, 300 primary care physicians (PCPs), and 100 sleep medicine specialists conducted in the USA. The study showed that even if 62% of sleep specialists and 24% of PCPs considered themselves “very” or “extremely” knowledgeable about narcolepsy, only 42% and 9% of sleep specialists and PCPs, respectively, felt “very” or “extremely” comfortable diagnosing the disorder. The striking finding was however that only 22% of sleep specialists and 7% of PCPs identified all 5 key narcolepsy symptoms; particularly, while excessive daytime sleepiness and cataplexy were more easily recognized, the other symptoms were instead more rarely investigated and recognized.
An Italian survey disclosed that pediatricians and child neuropsychiatrists scored low in all areas of sleep knowledge and particularly in questions about narcolepsy, sleep apnea, and parasomnias [63].
In order to reach patients’ needs and overcome the diagnostic gap, AIN has promoted the initiative at issue aiming at analyzing the reasons that hamper a timely diagnosis and to offer to general clinicians, pediatricians, and neurologists a document containing Red Flags that can help in a prompt recognition of symptoms that can lead to suspect narcolepsy, in order to refer the patient to the reference centers for the diagnosis.
As far as barriers analysis is concerned, results of questionnaires confirmed that both patients and clinicians judged lack of knowledge of symptoms as a main factor hampering a right and timely diagnosis. Particularly, as emerged also in the AWAKEN study [21], the scarce knowledge about symptoms different from excessive daytime sleepiness and cataplexy emerges as one of the main causes in delaying the proper recognition of the disease.
Indeed, in more than 60% of both pediatric and adult patients, narcolepsy was not suspected at the first outpatient evaluation; and therefore nearly 60% of patients needed to consult more than two physicians. In over 50% of cases, a diagnosis of different organic conditions (epilepsy, sleep apnea, brain lesions) or of a psychiatric condition was made.
Noteworthy, what came to light from our survey was the shorter mean diagnostic delay in Italy compared to other European data (namely 2.1 years for pediatric cases and 6.7 years for adults). This could be due to the shortening of the delay in the last years (note the difference between children and adults), also thanks to awareness campaigns on narcolepsy that AIN has been promoting since 2000. These data could also be biased by the small sample size and the recruitment process (voluntary).
Considering the differences in phenotypic presentations in adults and children, different sets of Red Flags have been produced for the two populations and we distinguished two different scenarios: the first one with symptoms that are already sufficient to suspect the diagnosis and two additional conditions for children and one for adults that concern associated symptoms in which we recommend instead to investigate the presence of excessive daytime sleepiness and cataplexy, prior referring patients to the reference centers for the diagnosis.
The panel focused particularly in defining the peculiar features of narcolepsy in children and mainly the discrete manifestation of excessive daytime sleepiness, which not always presents with sleep attacks and the typical phenotype of cataplexy in children.
Indeed, the best predictor of a delayed diagnosis, along with the absence of cataplexy, is known to be the pediatric onset of symptoms [26]. This is because pediatric narcolepsy near the onset of the disease may have peculiar features [3, 36], as excessive daytime sleepiness may be manifested as paradoxical hyperactivity, elongation of nighttime sleep, resume of post prandial sleep and symptoms like hallucinations, RBD, and confusional arousals may be difficult to be articulated by children [26, 27]. Similarly, cataplexy at onset may present with the peculiar subcontinuous hypotonia and “cataplectic face” with superimposed dyskinesia or motor hyperactivity resembling other neurodevelopmental disorders [23, 24, 28].
Experts also focused on the description of symptoms different from excessive daytime sleepiness and cataplexy, since both the AWAKEN survey [21] and our own survey highlighted that clinicians may be more confident in investigating the cardinal features of narcolepsy (i.e., excessive daytime sleepiness and cataplexy), while less so in identifying the remaining symptoms typical of the narcolepsy pentad, i.e., hallucinations, sleep paralysis, and disrupted nocturnal sleep with RBD.
This report, by producing Red Flags guiding in suspecting the diagnosis of narcolepsy, has been therefore an attempt to overcome the major barriers identified through the survey.
References
American Academy of Sleep Medicine (2005) The International Classification of Sleep Disorders: Diagnostic & Coding Manual. 2nd ed. Rochester, MN: American Academy of Sleep Medicine
Scammell TE (2015) Narcolepsy. N Engl J Med 373:2654–2662
Postiglione E, Antelmi E, Pizza F, Lecendreux M, Dauvilliers Y, Plazzi G (2018) The clinical spectrum of childhood narcolepsy. Sleep Med Rev 38:70–85
Dauvilliers Y, Montplaisir J, Molinari N, Carlander B, Ondze B, Besset A, Billiard M (2001) Age at onset of narcolepsy in two large populations of patients in France and Quebec. Neurology 57:2029–2033
Hublin C, Partinen M, Kaprio J, Koskenvuo M, Guilleminault C (1994) Epidemiology of narcolepsy. Sleep 17:S7–12
Ohayon MM, Priest RG, Zulley J, Smirne S, Paiva T (2002) Prevalence of narcolepsy symptomatology and diagnosis in the European general population. Neurology 58:1826–1833
Silber MH, Krahn LE, Olson EJ, Pankratz VS (2002) The epidemiology of narcolepsy in Olmsted County, Minnesota: a population-based study. Sleep 25:197–202
Wing YK, Li RH, Lam CW, Ho CK, Fong SY, Leung T (2002) The prevalence of narcolepsy among Chinese in Hong Kong. Ann Neurol 51:578–584
Longstreth WT Jr, Koepsell TD, Ton TG, Hendrickson AF, van Belle G (2007) The epidemiology of narcolepsy. Sleep 30:13–26
Shin YK, Yoon IY, Han EK, No YM, Hong MC, Yun YD, Jung BK, Chung SH, Choi JB, Cyn JG, Lee YJ, Hong SC (2008) Prevalence of narcolepsy-cataplexy in Korean adolescents. Acta Neurol Scand 117:273–278
Wijnans L, Lecomte C, de Vries C, Weibel D, Sammon C, Hviid A, Svanström H, Mølgaard-Nielsen D, Heijbel H, Dahlström LA, Hallgren J, Sparen P, Jennum P, Mosseveld M, Schuemie M, van der Maas N, Partinen M, Romio S, Trotta F, Santuccio C, Menna A, Plazzi G, Moghadam KK, Ferro S, Lammers GJ, Overeem S, Johansen K, Kramarz P, Bonhoeffer J, Sturkenboom MCJM (2013) The incidence of narcolepsy in Europe: before, during, and after the influenza A(H1N1)pdm09 pandemic and vaccination campaigns. Vaccine 31:1246–1254
Taruscio D, Rocchetti A, Torreri P, Ferrari G, Kodra Y, Salerno P, Vittozzi L (2017). Il Registro Nazionale Malattie Rare nel contesto nazionale e internazionale. 3° Rapporto (dati al 31 dicembre 2014). Roma: Istituto Superiore di Sanità. (Rapporti ISTISAN 17/8)
Taruscio D, Vittozzi L, Rocchetti A, Torreri P, Ferrari L (2018) The occurrence of 275 rare diseases and 47 rare disease groups in Italy. Results from the National Registry of Rare Diseases. Int J Environ Res Public Health 15:1470
Kryger MH, Walid R, Manfreda J (2002) Diagnoses received by narcolepsy patients in the year prior to diagnosis by a sleep specialist. Sleep 25:36e41
Morrish E, King MA, Smith IE, Shneerson JM (2004) Factors associated with a delay in the diagnosis of narcolepsy. Sleep Med 5:37–41
Thorpy MJ, Krieger AC (2014) Delayed diagnosis of narcolepsy: characterization and impact. Sleep 15:502–507
Taddei RN, Werth E, Poryazova R, Baumann CR, Valko PO (2016) Diagnostic delay innarcolepsy type 1: combining the patients’ and the doctors’ perspectives. J Sleep Res 25:709–715
Thorpy MJ, Hiller G (2017) The medical and economic burden of narcolepsy: implications for managed care. Am Health Drug Benefits 10:233–241
Macleod S, Ferrie C, Zuberi SM (2005) Symptoms of narcolepsy in children misinterpreted as epilepsy. Epileptic Disord 7:13–17
Kauta SR, Marcus CL (2012) Cases of pediatric narcolepsy after misdiagnoses. Pediatr Neurol 47:362–365
Rosenberg R, Kim AY (2014) The AWAKEN survey: knowledge of narcolepsy among physicians and the general population. Postgrad Med 26:78–86
Carter LP, Acebo C, Kim A (2014) Patients’ journeys to a narcolepsy diagnosis: a physician survey and retrospective chart review. Postgrad Med 126:216–224
Plazzi G, Pizza F, Palaia V, Franceschini C, Poli F, Moghadam KK, Cortelli P, Nobili L, Bruni O, Dauvilliers Y, Lin L, Edwards MJ, Mignot E, Bhatia KP (2011) Complex movement disorders at disease onset in childhood narcolepsy with cataplexy. Brain 134:3477–3489
Pizza F, Franceschini C, Peltola H, Vandi S, Finotti E, Ingravallo F, Nobili L, Bruni O, Lin L, Edwards MJ, Partinen M, Dauvilliers Y, Mignot E, Bhatia KP, Plazzi G (2013) Clinical and polysomnographic course of childhood narcolepsy with cataplexy. Brain 136:3787–3795
Aran A, Einen M, Lin L, Plazzi G, Nishino S, Mignot E (2010) Clinical and therapeutic aspects of childhood narcolepsy-cataplexy: a retrospective study of 51 children. Sleep 33:1457–1464
Maski K, Steinhart E, Williams D, Scammell T, Flygare J, McCleary K, Gow M (2017) Listening to the patient voice in narcolepsy: diagnostic delay, disease burden, and treatment efficacy. J Clin Sleep Med 13:419–425
Dunne L, Patel P, Maschauer EL, Morrison I, Riha RL (2016) Misdiagnosis of narcolepsy. Sleep Breath 20:1277–1284
Serra L, Montagna P, Mignot E, Lugaresi E, Plazzi G (2008) Cataplexy features in childhood narcolepsy. Mov Disord 23:858–865
Ingravallo F, Gnucci V, Pizza F, Vignatelli L, Govi A, Dormi A, Pelotti S, Cicognani A, Dauvilliers Y, Plazzi G (2012) The burden of narcolepsy with cataplexy: how disease history and clinical features influence socio-economic outcomes. Sleep Med 13:1293–1300
Dodel R, Peter H, Walbert T et al (2004) The socioeconomic impact of narcolepsy. Sleep 27:1123e8
Smolensky MH, Di Milia L, Ohayon MM, et al (2011) Sleep disorders, medical conditions, and road accident risk. Accid Anal Prev; 43:533e48
Jennum P, Ibsen R, Petersen ER et al (2012) Health, social, and economic consequences of narcolepsy: a controlled national study evaluating the societal effect on patients and their partners. Sleep Med 13:1086e93
Ohayon MM (2013) Narcolepsy is complicated by high medical and psychiatric comorbidities: a comparison with the general population. Sleep Med 14:488e92
Ohayon MM, Black J, Lai C et al (2014) Increased mortality in narcolepsy. Sleep 37:439e44
DynaMed Plus [Internet]. Ipswich (MA): EBSCO Information Services. 1995 - . Record No. 116132, Narcolepsy; [updated 2018 Mar 09, cited place cited date here]; [about 29 screens]. Available from http://www.dynamed.com/login.aspx?direct=true&site=DynaMed&id=116132. Registration and login required. Last access May 28, 2018
Kotagal S. Narcolepsy in children. Scammell TE, Chervin RD, Eichler AF, eds. UpToDate. Waltham, MA: UpToDate Inc. http://www.uptodate.com. Last access May 28, 2018
Scammell TE. Clinical features and diagnosis of narcolepsy in adults. Benca R, Eichler AF, eds. UpToDate. Waltham, MA: UpToDate Inc. http://www.uptodate.com. Last access May 28, 2018
Flottorp SA, Oxman AD, Krause J et al (2013) A checklist for identifying determinants of practice: a systematic review and synthesis of frameworks and taxonomies of factors that prevent or enable improvements in healthcare professional practice. Implement Sci 23:8–35
Wise J, Lynch J (2001) Narcolepsy in children. Semin Pediatr Neurol 8:198–206
Babiker MO, Prasad M (2015) Narcolepsy in children: a diagnostic and management approach. Pediatr Neurol 52:557–565
Partinen M, Saarenpää-Heikkilä O, IlveskoskIi et al (2012) Increased incidence and clinical picture of childhood narcolepsy following the 2009 H1N1 pandemic vaccination campaign in Finland. Plos One 2:e33723
Lee J, Na G, Joo EY, Lee M, Lee J (2017) Clinical and polysomnographic characteristics of excessive daytime sleepiness in children. Sleep Breath 21:967–974
Prasad M, Setty G, Ponnusamy A et al (2014) Cataplectic facies: clinical marker in the diagnosis of childhood narcolepsy-report of two cases. Pediatr Neurol 515:517
Dhondt K, Verhelst H, Pevernagie D, Slap F, Van Coster R (2009) Childhood narcolepsy with partial facial cataplexy: a diagnostic dilemma. Sleep Med 10:797–798
Jardri R, Bartels-Velthuis DM et al (2014) From phenomenology to neurophysiological understanding of hallucinations in children and adolescents. Schizophr Bull 40:S221–S232
Nevsimalova S, Prihodova I, Kemlink D, Lin L, Mignot E (2007) REM behavior disorder (RBD) can be one of the first symptoms of childhood narcolepsy. Sleep Med 8:784–786
Lloyd R, Tippmann-Peikert M, Slocumb N, Kotagal S (2012) Characteristics of REM sleep behavior disorder in childhood. J Clin Sleep Med 8:127
Pisko J, Pastorek L, Buskova J, Sonka K, Nevsimalova S (2014) Nightmares in narcolepsy: underinvestigated symptoms? Sleep Med 15:967–972
Antelmi E, Pizza F, Vandi S, Neccia G, Ferri R, Bruni O, Filardi M, Cantalupo G, Liguori R, Plazzi G (2017) The spectrum of REM sleep-related episodes in children with type 1 narcolepsy. Brain 140:1669–1679
Wang Z, Wu H, Stone WS, Zhuang J, Qiu L, Xu X, Wang Y, Zhao Z, Han F, Zhao Z (2016) Body weight and basal metabolic rate in childhood narcolepsy: a longitudinal study. Sleep Med 25:139–144
Ponziani V, Gennari M, Pizza F, Balsamo A, Bernardi F, Plazzi G (2016) Growing up with type 1 narcolepsy: its anthropometric and endocrine features. J Clin Sleep Med 12:1649–1657
Poli F, Pizza F, Mignot E, Ferri R, Pagotto U, Taheri S, Finotti E, Bernardi F, Pirazzoli P, Cicognani A, Balsamo A, Nobili L, Bruni O, Plazzi G (2013) High prevalence of precocious puberty and obesity in childhood narcolepsy with cataplexy. Sleep 36:175–181
Dahmen N, Bierbrauer J, Kasten M (2001) Increased prevalence of obesity in narcoleptic patients and relatives. Eur Arch Psychiatry Clin Neurosci 251:85–89
Vetrugno R, D’Angelo R, Moghadam KK et al (2010) Behavioural and neurophysiological correlates of human cataplexy: a video-polygraphic study. Clin Neurophysiol 121:153–162
Overeem S, van Nues SJ, van der Zande WL, Donjacour CE, van Mierlo P, Lammers GJ (2011) The clinical features of cataplexy: a questionnaire study in narcolepsy patients with and without hypocretin-1 deficiency. Sleep Med 12(12):12–18
Pizza F, Antelmi E, Vandi S, Meletti S, Erro R, Baumann CR, Bhatia KP, Dauvilliers Y, Edwards MJ, Iranzo A, Overeem S, Tinazzi M, Liguori R, Plazzi G (2018) The distinguishing motor features of cataplexy: a study from video-recorded attacks. Sleep 41(5). https://doi.org/10.1093/sleep/zsy026
Plazzi G, Serra L, Ferri R (2008) Nocturnal aspects of narcolepsy with cataplexy. Sleep Med Rev 12:109–128
Dauvilliers Y, Jennum P, Plazzi G (2013) Rapid eye movement sleep behavior disorder and rapid eye movement sleep without atonia in narcolepsy. Sleep Med 14:775–781
Franceschini C, Ferri R, Pizza F, Ricotta L, Vandi S, Detto S, Poli F, Pruneti C, Mazzetti M, Cipolli C, Lugaresi E, Plazzi G (2011) Motor events during REM sleep in patients with narcolepsy-cataplexy: a video-polysomnographic pilot study. Sleep Med 12:S59–S63
Cipolli C, Franceschini C, Mattarozzi K, Mazzetti M, Plazzi G (2011) Overnight distribution and motor characteristics of REM sleep behaviour disorder episodes in patients with narcolepsy-cataplexy. Sleep Med 12:635–640
Rinaldi R, Vignatelli L, D’Alessandro R et al (2001) Validation of symptoms related to excessive daytime sleepiness. Neuroepidemiology 20:248–256
Vignatelli L, Plazzi G, Barbato A, Ferini-Strambi L, Manni R, Pompei F, D’Alessandro R, GINSEN (Gruppo Italiano Narcolessia Studio Epidemiologico Nazionale (2003) Italian version of the Epworth sleepiness scale: external validity. Neurol Sci 23:295–300
Bruni O, Violani C, Luchetti A, Miano S, Verrillo E, Di Brina C, Valente D (2004) The sleep knowledge of pediatricians and child neuropsychiatrists. Sleep and Hypnosis 6:130–138
Acknowledgments
We are indebted to all the participants of the survey, members of the Associazione Italiana Narcolettici e Ipersonni (AIN onlus; http://www.narcolessia.it/). We thank Cecilia Baroncini for editing the English text.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Additional information
This manuscript is dedicated to the memory of Icilio Ceretelli (15.04.1948- 07.11.2018), founder of the Italian Narcolepsy Association (AIN). He deeply wanted and promoted this project and hardly worked for its fulfillment.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Promoted by: the Italian association of patients with narcolepsy and hypersomnia (Associazione Italiana Narcolettici e Ipersonni, AIN). The following scientific societies and institutions endorsed the project by appointing a representative member: the Italian society of neurology (Società Italiana di Neurologia, SIN); the Italian society of pediatric neurology (Società Italiana Neurologia Pediatrica, SINP); the Italian society of social and preventive medicine (Società Italiana di Pediatria Preventiva e Sociale, SIPPS); the Italian society of pediatrics (Società Italiana di Pediatria, SIP); the Italian society of general practitioners (Società Italiana di Medicina Generale, SIMG); the Italian society of neurophychiatrists for children and adolescents (Società italiana di neuropsichiatria dell’infanzia e dell’adolescenza, SIMPIA); the World Association of Sleep Medicine (WASM); the Italian association of sleep medicine (Associazione Italiana Medicina del Sonno, AIMS), the Italian association of healthcare managers (Associazione Nazionale Medici di Direzione Ospedaliera), the Italian institute of health (Istituto Superiore di Sanità, ISS).
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 48.9 mb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Vignatelli, L., Antelmi, E., Ceretelli, I. et al. Red Flags for early referral of people with symptoms suggestive of narcolepsy: a report from a national multidisciplinary panel. Neurol Sci 40, 447–456 (2019). https://doi.org/10.1007/s10072-018-3666-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10072-018-3666-x