Abstract
Objectives
The aim of the study is to identify clusters of lymphocyte subsets within treatment-naive systemic lupus erythematosus (SLE) patients and evaluate the potential association of these clusters with disease activities.
Methods
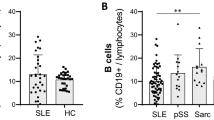
We conducted a cross-sectional study of consecutive 143 treatment-naive SLE patients in the Affiliated Hospital of Nantong University, China. We used hierarchical cluster analysis to classify individuals into clusters based on circulating lymphocyte subset proportions (CD3+CD4+T cell, CD3+CD8+T cell, CD19+B cell, and CD3-CD16 + CD56 NK cell) via R software. Demographic variables, clinical manifestations, laboratory variables, and disease activities were compared among clusters.
Results
The SLE patients (median age 35 (26–48) years, 90.9% female) were divided into four clusters. The clustering features were as follows: cluster 1 (B high), cluster 2 (CD4 high), cluster 3 (CD8 high), and cluster 4 (NK high). SLE patients in cluster 1 showed the highest incidence of arthritis (70.6%, 34.2%, 48.3%, and 42.9% in clusters 1, 2, 3, and 4, respectively; P = 0.046), and patients in cluster 3 and cluster 4 showed significantly a higher incidence of nephritis (35.3%, 25.0%, 48.3%, and 61.9% in in clusters 1, 2, 3, and 4, respectively; P = 0.008). Patients in cluster 2 suffered from lower SLE Disease Activity Index (SLEDAI) score (12.1 ± 5.0, 10.3 ± 5.6, 12.2 ± 4.6, and 14.4 ± 7.3 in clusters 1, 2, 3, and 4, respectively; P = 0.046). Regression analysis indicated that, compared with patients in cluster 2, patients in cluster 1 exhibited higher rate of arthritis (OR 4.53, 95% CI 1.38–14.86, P = 0.013), while patients in cluster 3 (OR 2.85, 95%CI 1.15–7.08, P = 0.024) and cluster 4 (OR 4.93, 95%CI 1.76–13.85, P = 0.002) exhibited higher rate of nephritis.
Conclusion
This study supports the existence of lymphocyte subset clusters with different clinical features in treatment-naive SLE patients, which could help to differentiate between various subsets of SLE.
Key Points • Lymphocyte subsets may occur in a pattern of cluster in treatment-naive SLE patients. |

Similar content being viewed by others
References
Hurd K, Barnabe C (2018 Feb) Mortality causes and outcomes in Indigenous populations of Canada, the United States, and Australia with rheumatic disease: a systematic review. Semin Arthritis Rheum 47(4):586–592. https://doi.org/10.1016/j.semarthrit.2017.07.009
Durcan L, O'Dwyer T, Petri M (2019) Management strategies and future directions for systemic lupus erythematosus in adults. Lancet 393(10188):2332–2343. https://doi.org/10.1016/S0140-6736(19)30237-5
Tsokos GC, Lo MS, Costa Reis P, Sullivan KE (2016 Nov 22) New insights into the immunopathogenesis of systemic lupus erythematosus. Nat Rev Rheumatol 12(12):716–730. https://doi.org/10.1038/nrrheum.2016.186
Toro-Domínguez D, Martorell-Marugán J, Goldman D, Petri M, Carmona-Sáez P, Alarcón-Riquelme ME (2018) Stratification of systemic lupus erythematosus patients into three groups of disease activity progression according to longitudinal gene expression. Arthritis Rheum 70(12):2025–2035. https://doi.org/10.1002/art.40653
Barturen G, Beretta L, Cervera R, Van Vollenhoven R, Alarcón-Riquelme ME (2018) Moving towards a molecular taxonomy of autoimmune rheumatic diseases. Nat Rev Rheumatol 14(2):75–93. https://doi.org/10.1038/nrrheum.2017.220 Review
Artim-Esen B, Çene E, Şahinkaya Y, Ertan S, Pehlivan Ö, Kamali S, Gül A, Öcal L, Aral O, Inanç M (2014 Jul) Cluster analysis of autoantibodies in 852 patients with systemic lupus erythematosus from a single center. J Rheumatol 41(7):1304–1310. https://doi.org/10.3899/jrheum.130984
Pego-Reigosa JM, Lois-Iglesias A, Rúa-Figueroa Í, Galindo M, Calvo-Alén J, de Uña-Álvarez J, Balboa-Barreiro V, Ibáñez Ruan J, Olivé A, Rodríguez-Gómez M, Fernández Nebro A, Andrés M, Erausquin C, Tomero E, Horcada Rubio L, Uriarte Isacelaya E, Freire M, Montilla C, Sánchez-Atrio AI, Santos-Soler G, Zea A, Díez E, Narváez J, Blanco-Alonso R, Silva-Fernández L, Ruiz-Lucea ME, Fernández-Castro M, Hernández-Beriain JÁ, Gantes-Mora M, Hernández-Cruz B, Pérez-Venegas J, Pecondón-Español Á, Marras Fernández-Cid C, Ibáñez-Barcelo M, Bonilla G, Torrente-Segarra V, Castellví I, Alegre JJ, Calvet J, Marenco de la Fuente JL, Raya E, Vázquez-Rodríguez TR, Quevedo-Vila V, Muñoz-Fernández S, Otón T, Rahman A, López-Longo FJ (2016) Relationship between damage clustering and mortality in systemic lupus erythematosus in early and late stages of the disease: cluster analyses in a large cohort from the Spanish Society of Rheumatology Lupus Registry. Rheumatology (Oxford) 55(7):1243–1250. https://doi.org/10.1093/rheumatology/kew049
Banchereau R, Hong S, Cantarel B, Baldwin N, Baisch J, Edens M, Cepika AM, Acs P, Turner J, Anguiano E, Vinod P, Kahn S, Obermoser G, Blankenship D, Wakeland E, Nassi L, Gotte A, Punaro M, Liu YJ, Banchereau J, Rossello-Urgell J, Wright T, Pascual V (2016) Personalized immunomonitoring uncovers molecular networks that stratify lupus patients. Cell. 165(3):551–565. https://doi.org/10.1016/j.cell.2016.03.008
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725. https://doi.org/10.1002/art.1780400928
Bombardier C, Gladman DD, Urowitz MB, Caron D, Chang CH (1992) Derivation of the SLEDAI. A disease activity index for lupus patients. The Committee on Prognosis Studies in SLE. Arthritis Rheum 35:630–640. https://doi.org/10.1002/art.1780350606
Torres-Ruiz J, Mejía-Domínguez NR, Zentella-Dehesa A, Ponce-de-León A, Morales-Padilla SR, Vázquez-Rodríguez R (2019) The systemic lupus erythematosus infection predictive index (LIPI): a clinical-immunological tool to predict infections in lupus patients. Front Immunol 9:3144. https://doi.org/10.3389/fimmu.2018.03144 eCollection 2018
Kubo S, Nakayamada S, Yoshikawa M, Miyazaki Y, Sakata K, Nakano K, Hanami K, Iwata S, Miyagawa I, Saito K, Tanaka Y (2017) Peripheral immunophenotyping identifies three subgroups based on t cell heterogeneity in lupus patients. Arthritis Rheum 69(10):2029–2037. https://doi.org/10.1002/art.40180
Jacobi AM, Mei H, Hoyer BF, Mumtaz IM, Thiele K, Radbruch A, Burmester GR, Hiepe F, Dörner T (2010) HLA-DRhigh/CD27high plasmablasts indicate active disease in patients with systemic lupus erythematosus. Ann Rheum Dis 69(1):305–308. https://doi.org/10.1136/ard.2008.096495
Robinson GA, Peng J, Dönnes P, Coelewij L, Naja M, Radziszewska A, Wincup C, Peckham H, Isenberg DA, Ioannou Y, Pineda-Torra I, Ciurtin C, Jury EC (2020) Disease-associated and patient-specific immune cell signatures in juvenile-onset systemic lupus erythematosus: patient stratification using a machine-learning approach. Lancet Rheumatol 2(8):e485–e496. https://doi.org/10.1016/S2665-9913(20)30168-5
Manzi S, Sánchez-Guerrero J, Merrill JT, Furie R, Gladman D, Navarra SV, Ginzler EM, D’Cruz DP, Doria A, Cooper S, Zhong ZJ, Hough D, Freimuth W, Petri MA, BLISS-52 and BLISS-76 Study Groups (2012) Effects of belimumab, a B lymphocyte stimulator-specific inhibitor, on disease activity across multiple organ domains in patients with systemic lupus erythematosus: combined results from two phase III trials. Ann Rheum Dis 71(11):1833–1838. https://doi.org/10.1136/annrheumdis-2011-200831
Crispín JC, Kyttaris VC, Terhorst C, Tsokos GC (2010) T cells as therapeutic targets in SLE. Nat Rev Rheumatol 6(6):317–325. https://doi.org/10.1038/nrrheum.2010.60
von Spee-Mayer C, Siegert E, Abdirama D, Rose A, Klaus A, Alexander T, Enghard P, Sawitzki B, Hiepe F, Radbruch A, Burmester GR, Riemekasten G, Humrich JY (2016) Low-dose interleukin-2 selectively corrects regulatory T cell defects in patients with systemic lupus erythematosus. Ann Rheum Dis 75(7):1407–1415. https://doi.org/10.1136/annrheumdis-2015-207776
Teh CL, Wan SA, Ling GR (2018) Severe infections in systemic lupus erythematosus: disease pattern and predictors of infection-related mortality. Clin Rheumatol 37(8):2081–2086. https://doi.org/10.1007/s10067-018-4102-6
Lu Z, Li J, Ji J, Gu Z, Da Z (2019) Mortality prediction in systemic lupus erythematosus patients with pulmonary infection. Int J Rheum Dis 22(6):1077–1083. https://doi.org/10.1111/1756-185X.13555
Yuan Q, Xing X, Lu Z, Li X (2020 Jun 17) Clinical characteristics and risk factors of infection in patients with systemic lupus erythematosus: a systematic review and meta-analysis of observational studies. Semin Arthritis Rheum 50(5):1022–1039. https://doi.org/10.1016/j.semarthrit.2020.06.004
Lu Z, Li J, Ji J, Gu Z, Da Z (2019) Altered peripheral lymphocyte subsets in untreated systemic lupus erythematosus patients with infections. Braz J Med Biol Res 52(4):e8131. https://doi.org/10.1590/1414-431X20198131
Wolfe RM, Peacock JE Jr (2017 Jun) Pneumocystis pneumonia and the rheumatologist: which patients are at risk and how can PCP be prevented? Curr Rheumatol Rep 19(6):35. https://doi.org/10.1007/s11926-017-0664-6
Zimmer CL, Cornillet M, Solà-Riera C, Cheung KW, Ivarsson MA, Lim MQ, Marquardt N, Leo YS, Lye DC, Klingström J, MacAry PA, Ljunggren HG, Rivino L, Björkström NK (2019) NK cells are activated and primed for skin-homing during acute dengue virus infection in humans. Nat Commun 10(1):3897. https://doi.org/10.1038/s41467-019-11878-3
Fritsch RD, Shen X, Illei GG, Yarboro CH, Prussin C, Hathcock KS, Hodes RJ, Lipsky PE (2006) Abnormal differentiation of memory T cells in systemic lupus erythematosus. Arthritis Rheum 54(7):2184–2197. https://doi.org/10.1002/art.21943
Spada R, Rojas JM, Barber DF (2015) Recent findings on the role of natural killer cells in the pathogenesis of systemic lupus erythematosus. J Leukoc Biol 98(4):479–487
Huang Z, Fu B, Zheng SG, Li X, Sun R, Tian Z, Wei H (2011) Involvement of CD226+ NK cells in immunopathogenesis of systemic lupus erythematosus. J Immunol 186(6):3421–3431
Spada R, Rojas JM, Pérez-Yagüe S, Mulens V, Cannata-Ortiz P, Bragado R et al (2015) NKG2D ligand overexpression in lupus nephritis correlates with increased NK cell activity and differentiation in kidneys but not in the periphery. J Leukoc Biol 97(3):583–598
Sciascia S, Radin M, Yazdany J, Levy RA, Roccatello D, Dall'Era M, Cuadrado MJ (2017) Efficacy of belimumab on renal outcomes in patients with systemic lupus erythematosus: a systematic review. Autoimmun Rev 16(3):287–293. https://doi.org/10.1016/j.autrev.2017.01.010
Bruce IN, O'Keeffe AG, Farewell V, Hanly JG, Manzi S, Su L, Gladman DD, Bae SC, Sanchez-Guerrero J, Romero-Diaz J, Gordon C, Wallace DJ, Clarke AE, Bernatsky S, Ginzler EM, Isenberg DA, Rahman A, Merrill JT, Alarcón GS, Fessler BJ, Fortin PR, Petri M, Steinsson K, Dooley MA, Khamashta MA, Ramsey-Goldman R, Zoma AA, Sturfelt GK, Nived O, Aranow C, Mackay M, Ramos-Casals M, van Vollenhoven RF, Kalunian KC, Ruiz-Irastorza G, Lim S, Kamen DL, Peschken CA, Inanc M, Urowitz MB (2015) Factors associated with damage accrual in patients with systemic lupus erythematosus: results from the Systemic Lupus International Collaborating Clinics (SLICC) Inception Cohort. Ann Rheum Dis 74(9):1706–1713. https://doi.org/10.1136/annrheumdis-2013-205171
He J, Zhang X, Wei Y, Sun X, Chen Y, Deng J, Jin Y, Gan Y, Hu X, Jia R, Xu C, Hou Z, Leong YA, Zhu L, Feng J, An Y, Jia Y, Li C, Liu X, Ye H, Ren L, Li R, Yao H, Li Y, Chen S, Zhang X, Su Y, Guo J, Shen N, Morand EF, Yu D, Li Z (2016) Low-dose interleukin-2 treatment selectively modulates CD4(+) T cell subsets in patients with systemic lupus erythematosus. Nat Med 22(9):991–993. https://doi.org/10.1038/nm.4148
Acknowledgments
We thank all patients and healthy donors controls involved in the study.
Funding
This work was supported by the National Natural Science Foundation of China (Grant Nos. 81671606, 81601410), the Liaoning Distinguished Professor program (Liao taught 2018 to 2020), Dalian key laboratory of human homeostasis microbiology and disease immunology. Special Fund for Clinical Medicine, Nantong Science and Technology Bureau (Grant Nos. HS2014071 and HS2016003); Jiangsu Provincial Commission of Health and Family Planning (Grant No. H201623); and Nantong 226 Talents Project (Grant No. 2017-13).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
This study was approved by the Ethics Committee of the Affiliated Hospital of Nantong University.
Disclosures
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zhimin Lu and Weiping Li are the co-first authors.
Rights and permissions
About this article
Cite this article
Lu, Z., Li, W., Tang, Y. et al. Lymphocyte subset clustering analysis in treatment-naive patients with systemic lupus erythematosus. Clin Rheumatol 40, 1835–1842 (2021). https://doi.org/10.1007/s10067-020-05480-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-020-05480-y